Back to Journals » International Medical Case Reports Journal » Volume 9
Successful closure of treatment-naïve, flat edge (Type II), full-thickness macular hole using inverted internal limiting membrane flap technique
Received 18 July 2016
Accepted for publication 16 August 2016
Published 6 October 2016 Volume 2016:9 Pages 313—316
DOI https://doi.org/10.2147/IMCRJ.S117518
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ronald Prineas

Nazimul Hussain,1 Anjli Hussain2
1Department of Ophthalmology, Al Zahra Hospital, 2Al Zahra Medical Center, Dubai, United Arab Emirates
Objective: The objective of this study was to present the outcome of the internal limiting membrane (ILM) peeling flap technique for a treatment-naïve, flat edge (Type II), full-thickness macular hole (MH).
Methods: A 52-year-old man presented with complaints of decreased vision and seeing black spot. He was diagnosed to have a flat edge, full-thickness MH, which was confirmed by optical coherence tomography (OCT). He underwent 23G vitrectomy with brilliant blue G-assisted inverted ILM peeling with an inverted flap over the hole followed by fluid gas exchange.
Results: Postoperative follow-up until 3 months showed successful closure of the MH, which was confirmed by OCT. The best-corrected visual acuity improved from baseline 6/60 to 6/12 at the final follow-up.
Conclusion: Using the inverted ILM flap technique, a treatment-naïve, flat edge (Type II), full thickness MH achieved successful anatomical and functional outcomes.
Keywords: macular hole, inverted ILM, optical coherence tomography
Introduction
Macular hole (MH) is a full-thickness defect of the retinal tissue involving the fovea. It is confirmed by optical coherence tomography (OCT), and clinically, an MH appears like full-thickness defect with its edges lifted toward the vitreous and cystic changes seen at the edges of the neurosensory retina. This appearance of the MH is amenable to successful surgical outcome of its closure besides other known prognostic factors affecting the outcome.1–3
A large MH has increased risk of surgical failures, with 44% remains open after surgery.4 Similarly, it is also difficult to achieve successful closure in the refractory MH.5,6 In the recent past, such a surgically challenging MH had a promising outcome using the inverted internal limiting membrane (ILM) peeling flap technique.4–6 We report a successful closure of a treatment-naïve, flat edge, full-thickness MH (Type II appearance) using the inverted ILM peeling flap technique.
Case report
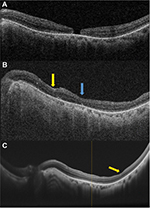
A 52-year-old man presented with complaints of seeing black spot in his vision in the left eye. He had a history of undergoing phacoemulsification with intraocular lens implantation and retinal laser done (for peripheral lattice degeneration) 2 years ago in the right eye. On examination, his best-corrected visual acuity was 6/9 in the right eye and 6/60 in the left eye. Anterior segment examination was unremarkable in both eyes except posterior chamber intraocular lens in place in the right eye and Grade 2 nuclear sclerosis with early cortical cataract in the left eye. Intraocular pressure was 16 mmHg and 18 mmHg in the right and left eyes, respectively. Dilated fundus examination showed clear ocular media, attached retina, inferior peripheral lattice degeneration, and vitreous liquefaction in the left eye. Macula showed a full-thickness MH without any cuff of fluid. The right eye showed clear ocular media, attached retina, and peripheral laser marks. OCT showed a full-thickness MH with flat edge in the left eye (Figure 1A) and a maintained foveal contour in the right eye. Based on the above mentioned clinical evaluation, a diagnosis of the full-thickness MH with flat edge, inferior peripheral lattice degeneration and cataract in the left eye, and pseudophakia in the right eye was made.
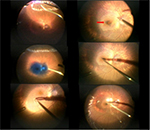
He underwent 23G vitrectomy, brilliant blue G-assisted ILM peeling (inverted flap technique), fluid gas exchange, and endolaser in the left eye. Intraoperatively, after induction of posterior vitreous detachment, vitrectomy was completed and endolaser was barraged around the inferior lattice degeneration (Figure 2, left top). Brilliant blue G was then injected over the macular area to stain the ILM (Figure 2, left middle). ILM peeling was initiated from the temporal side all around the MH, at approximately two-disk diameter area, and hinged at the edges of the hole (Figure 2, left bottom). ILM was then trimmed, and adequate residual ILM was inverted over the hole (Figure 2, right top/middle). Following this, fluid air exchange was performed and ILM was pushed into the MH (Figure 2, right bottom). Then air gas (SF6) exchange was done. Postoperative facedown positioning was maintained 6 hours a day for 5 days.
One week postoperative follow-up showed a closed MH in the left eye. Two months follow-up examination showed the best-corrected visual acuity of 6/24. Anterior segment examination showed Grade 2 nuclear sclerosis with early posterior subcapsular cataract and cortical spokes. Fundus examination showed attached retina, laser marks around the inferior lattice degeneration, and closed MH. OCT showed closed MH with a maintained foveal contour and dimpling in the temporal macula (Figure 1B). Three months follow-up examination showed the best-corrected visual acuity of 6/12 and N8. Repeat OCT showed a maintained foveal contour (Figures 1C and 3). Written informed consent for treatment and use of data was provided by the patient.
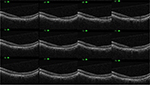  | Figure 3 Multiple line scan showing a closed MH 3 months after surgery. Abbreviation: MH, macular hole. |
Discussion
Inverted ILM peeling flap technique has improved the confidence of approach to successful surgical outcome in refractory and large MHs.4–6 Michalewska et al4 have shown that using the inverted ILM flap technique in eyes with a large MH (>400 μm size) had a 98% success rate of MH closure compared to 88% in eyes that underwent the standard technique. They suggested that the inverted ILM flap technique prevents postoperative flat open appearance of an MH and also improves the functional and anatomical outcomes of an MH >400 μm. They have also shown that the mean visual acuity at month 12 was 0.28 with the ILM flap technique and 0.17 without the flap technique (P=0.001).
Pires et al5 have also shown successful closure of the reopened MH that had undergone previous surgery using the ILM peeling translocation technique. The technique could achieve anatomic closure in eleven of 12 eyes (91%).
The current case presented closure of a treatment-naïve, Type II pattern MH appearance with flat edge3 in the eye that has not undergone any previous surgery. This has never been reported (in the PubMed). Using the ILM flap technique in this eye, successful anatomical and functional improvements (Figure 1) could be achieved. Our case and other publications4–6 imply that whatever is the technique, the concept of leaving the ILM over the hole remains the same and can improve the functional outcome. In Stage 2, usually there will be evidence of some form of vitreomacular adhesion or vitreomacular traction, which was not evident in this case besides the flat appearance of edges like a Type II closure. The size of the hole had a minimum diameter of 319 μm and base diameter of 345 μm. Since this was also associated with symptomatic vision decrease, the case was advised for surgery. Ideally, in small Stage 2 MH, one may defer surgery as there is a possibility of spontaneous closure and the hole size is usually <200 μm. The inverted ILM flap technique is usually performed for a chronic large MH, a failed MH, or high myopia with MH and foveal schisis. In this case, possibly because of the flat edge, there is less likelihood of vitrectomy alone being successful in the closure of MH. The ILM flap technique in such kind of eyes allows the Müller cells and external limiting membrane to grow along the ILM as a scaffold to close the hole. Our case demonstrates that a treatment-naïve, flat edge MH can achieve successful anatomical and functional outcomes using the ILM flap technique.
Disclosure
The authors report no conflicts of interest in this work.
References
Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW, Kampik A. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002;86(4):390–393. | ||
Freeman WR, Azen SP, Kim JW, et al. Vitrectomy for the treatment of full thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol. 1997;115(1):11–21. | ||
Kang SW, Ahn K, Ham D-I. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003;87(8):1015–1019. | ||
Michalewska Z, Michalewski J, Adelman RA, Nowrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117(10):2018–2025. | ||
Pires J, Nadal J, Gomes NL. Internal limiting membrane translocation for refractory macular holes. Br J Ophthalmol. Epub 2016 May 4. | ||
Gekka T, Watanabe A, Ohkuma Y, et al. Pedicle internal limiting membrane transposition flap technique for refractory macular hole. Ophthalmic Surg Lasers Imaging Retina. 2015;46(10):1045–1046. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.