Back to Journals » Clinical Ophthalmology » Volume 15
Success of Primary Trabeculectomy in Advanced Open Angle Glaucoma
Authors Pantalon A, Feraru C, Tarcoveanu F, Chiselita D
Received 24 February 2021
Accepted for publication 21 April 2021
Published 27 May 2021 Volume 2021:15 Pages 2219—2229
DOI https://doi.org/10.2147/OPTH.S308228
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Anca Pantalon,1 Crenguta Feraru,2 Filip Tarcoveanu,2,3 Dorin Chiselita1,2
1Ophthalmology Clinic, St. Spiridon Emergency University Hospital, Iași, Romania; 2Ophthalmology Department, Gr. T. Popa University of Medicine and Pharmacy, Iași, Romania; 3Ophthalmology Department, Countess of Chester Hospital NHS Trust, Chester, UK
Correspondence: Anca Pantalon
Ophthalmology Clinic, St. Spiridon University Hospital, Iași, Romania
Tel +40740686865
Email [email protected]
Crenguta Feraru
Ophthalmology Department, Gr. T. Popa University of Medicine and Pharmacy, Iași, Romania
Tel +40722752677
Email [email protected]
Aim: The study assesed trabeculectomy survival in advanced open angle glaucoma (OAG).
Methods: This is a retrospective longitudinal study in advanced OAG undergoing primary trabeculectomy. Clinical and demographic parameters were recorded. Surgical survival (qualified/complete) was calculated by Kaplan–Meier analysis for multiple upper limits of intraocular pressure (IOP) with/without medication (≤ 21 mmHg, ≤ 18 mmHg, ≤ 15 mmHg, ≤ 12 mmHg); Cox hazard ratio analysis identified parameters influencing survival.
Results: We included 165 eyes from 165 OAG patients: primary forms (POAG) – 86 eyes and secondary (pseudoexfoliative, SOAG) – 79 eyes; mean follow-up interval was 36.21 ± 13.49 months. Clinical parameters were comparable between sub-groups at baseline, except a higher IOP in SOAG vs POAG (36.6 ± 13.2 vs 32.7 ± 11.1 mmHg, p = 0.04); IOP reduction was similar (SOAG vs POAG) 53.93% vs 56.19%, p = 0.45, yet longer hospitalization (8.47 ± 4.39 (SOAG) vs 6.69 ± 3.01 days (POAG), p=0.03) and more medications (0.65 ± 0.24 vs 0.36 ± 0.16, p = 0.05) were needed to achieve comparable final IOP (16.0 ± 9.1 vs 15.1 ± 7.8 mmHg, p = 0.45). Kaplan Meier survival analysis applied for IOP ≤ 21 mmHg, ≤ 18 mmHg, ≤ 15 mmHg and ≤ 12 mmHg, revealed complete success in 26.2%, 27.3%, 34.5% and 54.6% eyes, respectively; qualified success was found in 45.7%, 48.6%, 77% and 88.6% eyes, respectively. Multiple medications at baseline diminished survival in all tested models (hazard ratio HR > 1, p< 0.05), while 5FU+needling improved survival, mostly if combined with lower IOP regime: HR = 0.15, 95% CI = [0.07 − 1.12], p = 0.06, if IOP ≤ 15 mmHg and HR = 0.09, 95% CI = [0.02– 1.25], p = 0.06, if IOP ≤ 12 mmHg.
Conclusion: Trabeculectomy in advanced OAG reached very good survival rates (77% and 88.6%) at 36 months postoperative, if IOP could be maintained ≤ 15 mmHg, respectively ≤ 12 mmHg with medication and additional needling+5FU maneuvers. Specific factors influencing survival were identified for each success definition.
Keywords: trabeculectomy, long term success, advanced open angle glaucoma
Introduction
Glaucoma is a progressive optic neuropathy which left untreated, leads to irreversible blindness.1 The goal of treatment is vision preservation by medical or surgical methods, aiming to correct the only treatable risk factor in glaucoma – the intraocular pressure (IOP).2,3 Developed by Cairns,4 trabeculectomy remains the “gold standard” in glaucoma filtering surgery, especially when low teens in IOP are aimed for in the postoperative interval to stabilize progression.5,6
In the last decade, there has been an active preoccupation to implement alternative methods to replace trabeculectomy.7 Recent literature reports declining rates of trabeculectomy,7,8 mostly if minimally invasive glaucoma surgery (MIGS) is addressed simultaneously with phacoemulsification.9–11 However MIGS procedures are mostly applicable in early to moderate stages of glaucoma, whereas in advanced stages filtering surgery offers a greater reduction in IOP, required to prevent glaucoma progression.12 In these circumstances, trabeculectomy still provides excellent IOP lowering capability,13 while having a comparable or lower risk of serious complications than other surgical options (e.g. tubes as primary choice).14,15 Considering the cost-effectiveness rationale, trabeculectomy remains the most frequent surgical procedure in glaucoma.16
After primary trabeculectomy performed in different types of glaucoma, multiple studies reported variable long-term success rates (between 48 – 98%), depending on definition and time-to-failure calculations,17 but fewer studies reported results after trabeculectomy in advanced glaucoma only.18
The aim of the study was to assess the efficacy of trabeculectomy in advanced open angle glaucoma (OAG) in a tertiary center.
Materials and Methods
This was a retrospective longitudinal study (2014–2019) that included advanced glaucoma patients in need for filtering surgery. We selected only advanced OAG cases, either primary (POAG) or secondary (SOAG), pseudoexfoliative forms, as defined by the European Glaucoma Society (EGS) and Hodapp criteria described elsewhere.6 All procedures were approved by the “Gr. T. Popa” University of Medicine and Pharmacy Ethics Committee and the Institutional Review Board of “St. Spiridon” University Hospital and respected the Declaration of Helsinki. All patients agreed and signed a written informed consent form. Clinical trial registration was not required, as the treatments being performed were standard of care at the hospital. Data were collected retrospectively from the clinical charts. Due to the retrospective nature of the study, the Institutional Review Board and the Ethics Committee waived the consent of the study, but privacy of the participants was kept; all data were anonymized and maintained with greatest confidentiality.
Indications for primary trabeculectomy were: uncontrolled IOP despite maximal tolerated medication, lifespan, status of fellow eye, non-compliance to therapy, allergy to medication, significant IOP fluctuations, defined as differences >10 mmHg between consecutive visits. Exclusion criteria eliminated other glaucoma subtypes, primary or secondary, significant ocular comorbidities or previous surgeries more recent than <180 days (e.g., phacoemulsification, laser procedures etc.). Eyes with normal tension glaucoma were excluded for homogeneity reasons. All patients underwent complete ophthalmic examination preoperatively. Clinical variables of interest were: age (years), gender, best corrected visual acuity (BCVA, logMAR), type of OAG (primary or secondary), baseline IOP (mmHg) as measured by Goldmann applanation tonometry (Haag-Streit, Koeniz, Switzerland), number of glaucoma medications, cup/disk (C/D) ratio (DRI OCT Triton™, Topcon), gonioscopy, lens status (phakic, pseudophakic) and fundus photography. Where possible and conditioned by a functional BCVA, visual field (VF) examination was performed (Humphrey Field Analyzer® II, Carl Zeiss Meditech Inc. California, central 10–2, size V stimulus); patients with a mean deviation (MD) greater than −20dB were identified at baseline. Goldmann perimetry was not available in the clinic. Conversion to logMAR for non-optotype BCVA was possible using Bojikian et al.19 recommendations.
For consistency, a primary fornix-based trabeculectomy was performed by a single experienced surgeon (D.C.), with or without placement of a soaked sponge of Mitomycin C (MMC, 0.03%) for 2–5 min. The MMC dosage and exposure time were adjusted in each patient individually, according to the individual risk factors for surgical failure; final decision was made once the sclera was exposed. Postoperative topical antibiotics were prescribed four times a day for a month and corticosteroids were instilled every 2 h for two weeks, then four times a day for the next four weeks with slow tapering afterwards, according to the bleb healing appearance. Patients were followed up daily in the first week post-trabeculectomy, then weekly in the first month, monthly in the first six months and then every three months for the remaining time. Needling maneuvers, performed at the slit lamp, were not considered re-intervention. For failing bleb, as considered by Hefetz20 and Mattox,21 5 fluorouracil (5FU) injections were used if: IOP ≥ 25 mmHg or IOP ≥ 21 mmHg with increasing IOP since the last visit ≥ 3 mmHg or if clinical aspect indicated failure(e.g. increased conjunctival vascularization and/or flat bleb).
Outcome Measures
Parameters at release and at each follow-up visit were recorded, when tests identical with baseline were carried out. Intra and postoperative complications (inflammation, persistent hypotony or hyphema, flat anterior chamber (AC), choroidal detachment, bleb failure etc.), additional maneuvers (laser suture lysis, flap re-suturing, reformation of the anterior chamber, needling procedures etc.) or major changes in BCVA were recorded.
The overall success was achieved if postoperative IOP ranged between 6–21 mmHg. Complete success according to World Glaucoma Association (WGA)17 was considered in eyes with IOP ≤ 21 mmHg without additional medication; qualified success was defined if IOP ≤ 21 mmHg, with medication. Failure of trabeculectomy was defined for medicated IOP > 21 mmHg or ≤ 5 mmHg, confirmed at two consecutive follow-up visits, at least one week apart. Persistent hypotony with anatomic changes, loss of light perception or need for a second surgery, performed in the operation theater, were categorized also as failure in our study. Based on the glaucoma advanced status, success (qualified and complete) was additionally calculated for different IOP upper limits, as following: ≤ 18 mmHg, ≤ 15 mmHg, ≤ 12 mmHg.
Statistical Analysis
We used IBM SPSS Statistics ver. 21.0 software (SPSS, Chicago, IL, USA) for the statistical analysis. Numeric data were analyzed as means ± standard deviation (SD) and frequency percentage. For categorical data, the Chi-square and Fisher exact tests were used. Intra-group differences, obtained from data taken at different time points, were evaluated using the Wilcoxon rank sum test. Surgical success was assessed by Kaplan–Meier survival curve analysis, with the p-value derived from a Log rank test. A p-value < 0.05 was considered significant. Factors influencing trabeculectomy success were tested using Cox proportional hazard calculations. Multivariate analysis was performed for all factors proving relevance at levels of p < 0.1 in initial univariate model. Association with success at level p < 0.05 was defined as significant.
Results
We included 165 eyes from 165 patients with OAG: 86 eyes with primary and 79 eyes with secondary (pseudoexfoliative) glaucoma forms. Sex distribution showed 45.4% females (75/165 eyes) and 54.6% males (90/165 eyes) in the study. Mean baseline IOP was 34.5 ± 12.3 mmHg, with a higher mean in SOAG vs POAG eyes, despite comparable intensity of treatment. A total of 121/165 eyes (73.33%) were phakic, with a significantly larger proportion in POAG vs SOAG eyes (84% vs 62%, p = 0.04). Perimetry was possible in 12 eyes. Baseline parameters are presented in Table 1.
 |
Table 1 Baseline Demographics and Clinical Parameters in the Study |
A fornix-based trabeculectomy was performed in all cases (165 eyes); the non-augmented trabeculectomy was employed in 54/165 (30.9%), while the augmented procedure (MMC, 0.03%) was performed in 114/165 eyes (69.1%). Mean exposure time to MMC, applied as a soaked sponge onto the sclera, was 3.06 ± 0.89 min (range: 2–5 minutes), with no difference between primary and secondary OAG forms (3.05 ± 0.93 min vs 3.08 ± 0.85 min, p = 0.87). Table 2 provides a comparison of baseline vs final parameters throughout the study.
 |
Table 2 Parameters in the Study (Baseline vs Final). Global Analysis and Sub-Groups Comparison |
Overall, BCVA decreased from baseline to the final visit (1.38 ± 1.09 vs 1.52 ± 1.09, p = 0.006), but at the last follow-up visit there was no difference between groups POAG vs SOAG, p = 0.85.
The need for medication was also significantly decreased at final vs baseline visit, as reflected both by the overall and by the sub-group analysis (p < 0.001); in SOAG vs POAG eyes we found a longer hospitalization interval (8.47 ± 4.39 days vs 6.69 ± 3.01 days, p = 0.03) and, at the last follow-up visit, more substances were needed in SOAG eyes to reach the same IOP control as POAG eyes (0.65 ± 0.24 vs 0.36 ± 0.16, p = 0.05). Effect of trabeculectomy in reducing IOP was significant and maintained until the last available follow-up visit. Table 3 shows that the IOP reduction in all OAG cases at the last follow-up visit was over 50–55% from baseline, without significant difference between sub-groups at each time point.
 |
Table 3 Variation of the IOP After Trabeculectomy in the Sub-Groups |
Tenonectomy was performed intraoperatively (47/165 eyes, 28.5%), before conjunctival flap closure upon surgeon’s judgment in each case individually; in comparable proportions (p = 0.851) POAG (25/86 eyes, 29%) vs SOAG (22/79 eyes, 27.8%), tenonectomy was added to the trabeculectomy procedure.
Modulation of bleb scarring by 5FU injections ± needling in the first three months post-op was applied in 63/165 eyes (38.18%); an overall mean number of 2.11 ± 1.44 (limit = 1–7) 5FU injections/eye were made, with comparable numbers in SOAG vs POAG eyes: 2.25 ± 1.68 vs 2.02 ± 1.23, p = 0.862. However, the proportion of eyes (%) in each sub-group where anti-fibrotic therapy was needed, was significantly higher in SOAG vs POAG: 45.5% (36/79 eyes) vs 31.3% (27/86 eyes), p = 0.04.
Complications
Early (<3 months) and late (>3 months) postoperative complications were analyzed and compared between groups. Early after trabeculectomy, a mean of 7.2% eyes needed laser suture lysis for high IOP, with significantly more interventions in SOAG vs POAG cases (p = 0.029). Overfiltration with low IOP and persistent shallow AC requiring intervention was met in 14.5% eyes. Ophthalmic viscosurgical devices (OVDs) injection, hexafluoride (SF6) gas injection or adjustment of scleral flap sutures were applied in these circumstances; significantly more SOAG vs POAG eyes (ratio = 2.6:1, p = 0.013) required corrective interventions, as presented in Table 4.
 |
Table 4 Early and Late Postoperative Complications After Trabeculectomy |
Compressive bandage or scleral contact lenses for deepening the AC due to postoperative over-filtration were not considered “interventions”. Transitory hyphema that appeared in 14/86 (16%) POAG eyes and in 17/79 (22%) SOAG eyes (p > 0.05) resolved spontaneously, under conventional post-op medication, with no need for additional interventions. Failed bleb (flat/encapsulated) needing a second surgical intervention after three months was noted in 6% eyes, with comparable distributions (%) and absolute values between groups (p > 0.05, Table 4). A single late case of blebitis (0.06%) with Staphylococcus spp. due to wound leakage was encountered in a pseudoexfoliative glaucoma patient at two months post-op. It required aggressive treatment and scleral patching, but eventually resolved after four weeks of intensive topical treatment. Late hypotonia with anatomical changes (persistent choroidal detachment, hypotony maculopathy) occurred in eight eyes (IOP = 2–5 mmHg), two eyes in the POAG group and six in the SOAG group. Throughout the study, 32/165 (19.4%) eyes completely lost the light perception and were also categorized as surgical failure; sub-group analysis found 14/86 (16.3%) eyes in POAG group and 18/79 (22.8%) eyes in SOAG group, p = 0.04.
Success of Trabeculectomy
According to the definition, surgical success and IOP control (≥ 6 mmHg and ≤ 21mmHg) without complete loss of vision was overall achieved in 127/165 (77%) eyes at the last available follow-up visit in 81.4% POAG vs 72.2% SOAG eyes, p = 0.36.
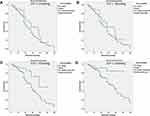
Based on the comparable survival proportions and similarities in the clinical outcomes, Kaplan Meier survival analysis with Log rank test was used to compare survival curves between complete vs qualified success in OAG cases all together, after a mean follow-up interval of 36.21 ± 13.49 months. General model for surgical success included all eyes with postoperative IOP between 6–21 mmHg, yet multiple IOP upper limits were analyzed, as following: ≤ 18 mmHg, ≤ 15 mmHg, ≤12 mmHg. Cumulative survival plots for all models are depicted below (Figure 1A-D).
Trabeculectomy survival for IOP ≤ 21 mmHg was 26.2% (complete) vs 45.7% (qualified); for IOP ≤ 18 mmHg, survival rate increased slightly to 27.3% complete and 48.6% qualified. Despite visible differences in absolute values between survival curves (complete vs qualified), statistical validation in the first two tested models was not found (p > 0.05), most likely due to uneven pattern of censorship per group when Kaplan Meier analysis was employed. For success definition with postoperative IOP ≤ 15 mmHg, complete success was achieved in 34.5% eyes and qualified success in 77% eyes (p = 0.004). Optimal survival rate occurred if IOP ≤ 12 mmHg and was found in 54.6% (complete) and 88.6% (qualified) eyes, respectively (p = 0.006).
Multivariate Cox Proportional Hazard Ratio analyzed the effect of several risk factors on trabeculectomy survival, according to each definition interval. Parameters such as age, tenonectomy, baseline IOP, intensity of treatment (number of medications) and needling maneuvers + 5FU injections were considered. Results are summarized in Table 5.
 |
Table 5 Hazard Ratio (HR) Analysis for Factors Influencing Trabeculectomy Surgical Success |
In all considered models, intensity of treatment at baseline impacted the surgical success, increasing the risk of failure by a factor of 1.62 up to 2.92 (p<0.05) if more medications were initially used (Table 5). If the lower IOP target was analyzed, a protective role in survival could be attributed to the needling maneuvers associated with 5FU injections, as HR<1 (95% CI) (p<0.05). In models where “bleb revision” as parameter gained statistical significance, few trabeculectomies failed at rates of 9% and 15%, respectively, as calculated if success was defined by an IOP ≤ 12 mmHg or ≤ 15 mmHg, respectively.
In our study, tenonectomy was performed in 47/165 eyes. There was no difference between groups “no tenonectomy” vs “tenonectomy” in terms of baseline IOP (35.4 ± 12.6 mmHg vs 32.5 ± 11.3 mmHg, p = 0.174), baseline medication (3.08 ± 0.95 vs 3.38 ± 0.70, p = 0.05), final IOP (15.8 ± 8.6 mmHg vs 14.9 ± 7.9 mmHg, p = 0.528), and post-operative medication (0.47 ± 0.94 vs 0.57 ± 1.19, p = 0.538). In addition, tenonectomy did not influence the survival of primary trabeculectomy at 36 months, according to the Cox hazard ratio analysis.
Discussion
Adequate IOP control in advanced glaucoma cases represents a challenge, especially when long-term monitoring is considered. In such patients, the concept of “target pressure” constitutes almost a philosophical term. Usually associated with cataract surgery, MIGS techniques offer a reduction in IOP around 20%, if applied in early to moderate glaucoma.12 Recently a “triple procedure” (phacoemulsification, iStent inject® trabecular micro-bypass insertion and endoscopic cyclophotocoagulation) offered IOP reduction of 35% from baseline in early-to-moderate glaucoma eyes at 12 months follow-up.22 However, in advanced glaucoma eyes, lower target pressures (low teens = 8–10 mmHg) are required, which can still best be achieved by trabeculectomy, offering 40–50% IOP reduction from baseline and various long-term success rates, according to definitions and follow-up interval.23–26
Postoperative complications are often described, of which excessive healing leading to surgical failure is the most feared.23 It is commonly accepted that almost 50% of trabeculectomies fail after five years, yet studies such as Landers and Watson’s25 report impressive survival time, using the conventional WGA definition for success: IOP between 5–21 mmHg, with or without medication.17,24 These recommendations are frequently used in most clinical trials, but in daily practice, assessment of surgical survival at different IOP targets could be more informative about progression risk in the studied population. Such evaluation might also reveal specific risk/protective factors for/against failure at different IOP targets and orient the clinician in having a correct insight upon the surgical outcome in glaucoma patients, especially when advanced stage glaucomas are studied. In this particular category, a recent WGA consensus suggested several alternative upper limits (≤ 21, ≤ 18, ≤ 15, and ≤ 12 mmHg) and one lower limit (6 mmHg) when assessing success definition by IOP criteria. Concept of “qualified/complete” success, if achieved with/without medications still applies.25
We used these cut-off values to assess the surgical success of trabeculectomy in advanced OAG, both primary and pseudoexfoliative forms, in Caucasian patients 65 ± 15 years of age, with IOP > 34 mmHg under multiple glaucoma medications (>3 substances), un-recordable VF (HFA II, 10–2 strategy) and low BCVA (logMAR > 1). Subgroup analysis revealed that mean baseline IOP in SOAG vs POAG cases was higher, under the same intensity of treatment. Reduction in IOP (%) after trabeculectomy was comparable between groups, yet a more aggressive treatment was needed to achieve the same IOP level throughout the study and longer hospitalization intervals were calculated for SOAG vs POAG eyes, before release.
A higher proportion of phakic eyes were described in primary vs secondary OAG forms (84% vs 62%, p = 0.04), probably related to the narrower angles present in pseudoexfoliation eyes that mandated cataract extraction earlier than in POAG cases.
As known, due to a substantial blood-aqueous breakdown in eyes with pseudoexfoliation,27 more trabeculectomy complications were met in SOAG eyes compared to POAG eyes. Pressure-wise, achievement of a satisfactory surgical outcome was conditioned by more corrective maneuvers (e.g. laser suture-lysis, AC reformation by OVD injection or suture readjustment) in SOAG vs POAG eyes. Also, significant anatomical changes occurring post-op were more frequent in SOAG vs POAG eyes. Both choroidal effusion (<3 months post-op) or hypotony maculopathy (≥3 months post-op) were met more often after trabeculectomy in SOAG than in POAG cases; nevertheless, the proportion of flat or encapsulated blebs at the last follow-up visit was similar. Based on this finding and according to the general WGA definition for success (6 mmHg < IOP ≤ 21 mmHg), success was achieved in 127/165 eyes (77%) at the last available follow-up visit (81.4% POAG vs 72.2% SOAG eyes, p = 0.36); further calculations in our trabeculectomy survival study were performed for all advanced OAG cases together. Previous studies described on short/medium term, similar survival rates between POAG and SOAG cases.28 Contrary, Ehrnrooth et al. described better survival rate in POAG vs pseudoexfoliation glaucoma at two and five years respectively, but acknowledged that the difference might have been caused by uneven sample sizes, changes in success definition, follow-up interval and demographics.23 A similar “layered” approach as in our study was reported by Li et al.29 By comparing survival rates between POAG and pseudoexfoliation glaucoma at different IOP targets, authors found comparable surgical success between sub-categories at three to six months postoperatively and better survival of POAG trabeculectomies at three to five years, regardless of any success interval.29 Previous studies brought even more controversy, as they reported better success rates in pseudoexfoliative glaucoma vs POAG after trabeculectomy as well as longer VF preservation.30–32 In our cohort of patients, VF and perimetric follow-up could not be performed due to very low BCVAs (logMAR>1) at baseline. As such, the decay in BCVA at the last available visit vs baseline could not be separated strictly between glaucoma progression and cataract formation, as a late complication after trabeculectomy in phakic eyes.
Functional criteria for success were equally important, as loss of light perception despite successful IOP lowering, was still considered failure in our OAG eyes. Achieving long-term success in pseudoexfoliative glaucoma is a very difficult task and a target maximum of 21 mmHg might be too hazardous for preventing progression.33 Therefore, we tested multiple upper limits for assessment of survival rates in real clinical life in an advanced OAG group, containing almost 50% pseudoexfoliation cases. Pseudoexfoliation is associated with a higher risk of surgical failure, higher IOP spikes and a more rapid progression; still no documentation of a greater rate of progression to blindness was reported after trabeculectomy in pseudoexfoliative glaucoma.25 This explains our statistical approach of testing all cases of advanced disease as a single clinical entity. In addition, regardless of glaucoma type, the level of disease (degree of VF loss) has been considered a major risk factor for progression to blindness. In our study, only 12 eyes could initially perform the VF, but due to the very advanced disease and low BCVA, this parameter could not be further exploited in our study and used for guidance. Eyes with severe glaucoma are more likely to fail after trabeculectomy. Since comparable baseline clinical characteristics were seen, homogeneity of the sub-groups (POAG vs SOAG) could be considered. Several parameters were described as being involved in failing blebs: age > 60 years, pseudoexfoliation, inflammation–uveitis/trauma, aphakia, multiple glaucoma medications (≥ 2 substances with preservatives), advanced forms of glaucoma.24,25 In addition, male patients exhibit an increased risk of failure by early encapsulation.34 In our study, sex distribution was relatively even, but the majority of the above cited risk factors were present, namely higher age, pseudoexfoliation, multiple anti-glaucoma medications – all containing preservatives – as a reflection of health policies and insurance coverage in our country at the time of the study. In such high-risk trabeculectomies, especially when associated with needling maneuvers and anti-fibrotic therapy,35 Mardelli et al. recommended 18 mmHg as the upper limit of the postoperative success interval.36 In terms of surgical survival in our study, there was no major change in rate when employing 21 mmHg or 18 mmHg as upper IOP limit with 26.6% vs 27.2% (complete success) and 45.7% vs 48.6% (qualified success), respectively. However, in advanced glaucoma cases, a postoperative IOP ≤ 18 mmHg was shown to be associated with lower progression risk and better vision preservation.37–40 Moreover, this limit was previously reported as an indirect hint for the need of re-intervention after primary trabeculectomy.26 Therefore, we presented the results for clinical orientation and comparison, even though no major changes in trabeculectomy survival were observed if IOP upper limit was lowered from 21 mmHg to 18 mmHg. Such low rates of success seemed to be influenced by the preoperative IOP (>34 mmHg) and number of medications (≥ 3), which have also been described by other studies as having a HR > 1 (95% CI, p < 0.05).41,42 In our study, better survival rates were met if lower medicated post-op IOP could be achieved during follow-up. If superior IOP limit was lowered from ≤15 mmHg to ≤12 mmHg, surgical success increased from 34.6% to 54.6% eyes (complete success) and from 77.0% to 88.6% eyes (qualified success), respectively. In both success intervals intensity of treatment at baseline, as reflected by the number of topical anti-glaucoma preserved medications, increased the risk of late trabeculectomy failure, whereas 5FU injections+needling maneuvers protected against failure as only 10% trabeculectomies failed, if such interventions were employed postoperatively. Similar results were described in multiple studies in eyes with failing blebs, rescued from failure by needling augmented with 5FU28,43 or MMC.29
Limitations of the study consist in the retrospective design and the global assessment of trabeculectomy survival in POAG and pseudoexfoliative glaucoma, altogether. Still, the authors consider that the statistical analysis would have become laboriously extended (complete vs qualified success rates in POAG vs SOAG), mostly when analyzed according to all four definitions of success, utilized in this study. In addition, if a similar amount of censored data is not present in both compared sub-groups, curves cannot be compared due to “confusing” differences in censoring patterns with actual group differences in survival distributions.44,45 This could also explain why, despite visible differences in the absolute values of the survival rates, in models with success definition “IOP ≤ 21 mmHg” or “IOP ≤ 18 mmHg”, the statistical significance could not validate the statistical model that compared absolute vs qualified success (p > 0.05) in these definitions. General success criteria provide homogeneity in academic studies, but in daily clinical practice, each glaucoma specialist should discuss trabeculectomy survival in an individualized manner, so that the best orientation is served for both doctor and patient.
The selection of patients with such advanced forms of glaucoma reflected the real-life data in a specific region and in a certain type of Caucasian population from Eastern Europe. In such areas, poor compliance of patients in undertaking regular check-ups and attending screening programs for early detection might be a game changer in the overall prognosis, if early stages could be timely detected. Implementing MIGS techniques and devices in our population, combined with limited access to optimal health care and financial resources represent the ultimate challenge for the glaucoma sub-specialist in this geographical area.
Studies report that if trabeculectomy survives at four years, there is a 40% chance for longer favorable outcome.26 As such, the authors intend to provide additional data, beyond five years and more in this particular Caucasian population.
Conclusions
Our study in advanced OAG (primary and pseudoexfoliative forms) showed that a target IOP in the range of low teens≤ 12 mmHg, achieved post-operatively with or without medication, is mandatory for increasing the chances of long-term trabeculectomy survival. Additional maneuvers such as needling+5FU injections further modulate healing and prevent surgical failure at three years postoperatively.
Author Contributions
All authors AP, CF, FT and DC made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):E1221–E1234.
2. Mayro EL, Wang M, Elze T, Pasquale LR. The impact of artificial intelligence in the diagnosis and management of glaucoma. Eye (Lond). 2020;34(1):1–11.
3. Wurster P, Harris A, Gonzalez AC, et al. Risk factors for open-angle glaucoma in persons of latin american descent. J Glaucoma. 2020;29(3):217–225.
4. Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66(4):673–679.
5. Kansal V, Armstrong JJ, Hutnik CM. Trends in glaucoma filtration procedures: a retrospective administrative health records analysis over a 13-year period in Canada. Clin Ophthalmol. 2020;14:501–508.
6. European Glaucoma Society. European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 2: classification and terminologySupported by the EGS Foundation: part 1: foreword; Introduction; Glossary; Chapter 2 Classification and Terminology. Br J Ophthalmol. 2017;101(5):73–127.
7. Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142.
8. Bhartiya S, Dhingra D, Shaarawy T. Revisiting results of conventional surgery: trabeculectomy, glaucoma drainage devices, and deep sclerectomy in the era of MIGS. J Curr Glaucoma Pract. 2019;13(2):45–49.
9. Vinod K, Gedde SJ, Feuer WJ, et al. Practice preferences for glaucoma surgery: a survey of the American glaucoma society. J Glaucoma. 2017;26(8):687–693.
10. Arriola-Villalobos P, Martinez-de-la-casa JM, Diaz-Valle D, Morales-Fernandez L, Fernandez-Perez C, Garcia-Feijoo J. Glaukos iStent inject(R) trabecular micro-bypass implantation associated with cataract surgery in patients with coexisting cataract and open-angle glaucoma or ocular hypertension: a long-term study. J Ophthalmol. 2016;2016:1056573.
11. Francis BA, Berke SJ, Dustin L, Noecker R. Endoscopic cyclophotocoagulation combined with phacoemulsification versus phacoemulsification alone in medically controlled glaucoma. J Cataract Refract Surg. 2014;40(8):1313–1321.
12. Bloom P, Au L. “Minimally Invasive Glaucoma Surgery (MIGS) is a poor substitute for trabeculectomy”The great debate. Ophthalmol Ther. 2018;7(2):203–210.
13. Gabai A, Cimarosti R, Battistella C, Isola M, Lanzetta P. Efficacy and safety of trabeculectomy versus nonpenetrating surgeries in open-angle glaucoma: a meta-analysis. J Glaucoma. 2019;28(9):823–833.
14. HaiBo T, Xin K, ShiHeng L, Lin L. Comparison of Ahmed glaucoma valve implantation and trabeculectomy for glaucoma: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0118142.
15. Namavari A, Hyde RA, Wang D, Vajaranant TS, Aref AA. Primary Baerveldt Shunt implantation: outcomes and complications. Ophthalmol Ther. 2016;5(2):253–262.
16. Agrawal P, Bradshaw SE. Systematic literature review of clinical and economic outcomes of Micro-Invasive Glaucoma Surgery (MIGS) in primary open-angle glaucoma. Ophthalmol Ther. 2018;7(1):49–73.
17. Heuer DK, Barton K, Grehn F, Shaarawy T, Sherwood M. Consensus on definitions of success. In: Shaarawy T, Sherwood M, Grehn F, editors. Guidelines on Design and Reporting of Surgical Trials. Amsterdam, The Netherlands: Kugler Publications; 2009:15–24.
18. Stead RE, King AJ. Outcome of trabeculectomy with mitomycin C in patients with advanced glaucoma. Br J Ophthalmol. 2011;95(7):960–965.
19. Bojikian KD, Stein AL, Slabaugh MA, Chen PP. Incidence and risk factors for traumatic intraocular pressure elevation and traumatic glaucoma after open-globe injury. Eye (Lond). 2015;29(12):1579–1584.
20. Hefetz L, Keren T, Naveh N. Early and late postoperative application of 5-fluorouracil following trabeculectomy in refractory glaucoma. Ophthalmic Surg. 1994;25(10):715–719.
21. Mattox C. Glaucoma filtration surgery and antimetabolites. Ophthalmic Surg Lasers. 1995;26(5):473–480.
22. Pantalon AD, Barata ADO, Georgopoulos M, Ratnarajan G. Outcomes of phacoemulsification combined with two iStent inject trabecular microbypass stents with or without endocyclophotocoagulation. Br J Ophthalmol. 2020;104(10):1378–1383.
23. Ehrnrooth P, Lehto I, Puska P, Laatikainen L. Long-term outcome of trabeculectomy in terms of intraocular pressure. Acta Ophthalmol Scand. 2002;80(3):267–271.
24. Casson R, Rahman R, Salmon JF. Long term results and complications of trabeculectomy augmented with low dose mitomycin C in patients at risk for filtration failure. Br J Ophthalmol. 2001;85(6):686–688.
25. Landers J, Martin K, Sarkies N, Bourne R, Watson P. A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology. 2012;119(4):694–702.
26. Dulku S. Trabeculectomy success rates. Ophthalmology. 2012;119(10):
27. Nguyen NX, Kuchle M, Martus P, Naumann GO. Quantification of blood–aqueous barrier breakdown after trabeculectomy: pseudoexfoliation versus primary open-angle glaucoma. J Glaucoma. 1999;8(1):18–23.
28. Lim SH, Cha SC. Long-term outcomes of Mitomycin-C trabeculectomy in exfoliative glaucoma versus primary open-angle glaucoma. J Glaucoma. 2017;26(4):303–310.
29. Li F, Tang G, Zhang H, Yan X, Ma L, Geng Y. The effects of trabeculectomy on pseudoexfoliation glaucoma and primary open-angle glaucoma. J Ophthalmol. 2020;2020:1723691.
30. Hollo G, Katsanos A, Konstas AG. Management of exfoliative glaucoma: challenges and solutions. Clin Ophthalmol. 2015;9:907–919.
31. Popovic V, Sjostrand J. Course of exfoliation and simplex glaucoma after primary trabeculectomy. Br J Ophthalmol. 1999;83(3):305–310.
32. Konstas AG, Jay JL, Marshall GE, Lee WR. Prevalence, diagnostic features, and response to trabeculectomy in exfoliation glaucoma. Ophthalmology. 1993;100(5):619–627.
33. Landa G, Pollack A, Rachmiel R, Bukelman A, Marcovich A, Zalish M. Results of combined phacoemulsification and trabeculectomy with mitomycin C in pseudoexfoliation versus non-pseudoexfoliation glaucoma. Graefes Arch Clin Exp Ophthalmol. 2005;243(12):1236–1240.
34. Schwartz AL, Van Veldhuisen PC, Gaasterland DE, Ederer F, Sullivan EK, Cyrlin MN. The Advanced Glaucoma Intervention Study (AGIS): 5. Encapsulated bleb after initial trabeculectomy. Am J Ophthalmol. 1999;127(1):8–19.
35. Shetty RK, Wartluft L, Moster MR. Slit-lamp needle revision of failed filtering blebs using high-dose mitomycin C. J Glaucoma. 2005;14(1):52–56.
36. Mardelli PG, Lederer CM
37. Rotchford AP, King AJ.Moving the goal posts definitions of success after glaucoma surgery and their effect on reported outcome. Ophthalmology. 2010;117(1):18–23.
38. Van Veldhuisen PC, Ederer F, Gaasterland DE, et al. The advanced glaucoma intervention study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440.
39. Sihota R, Angmo D, Ramaswamy D, Dada T. Simplifying “target” intraocular pressure for different stages of primary open-angle glaucoma and primary angle-closure glaucoma. Indian J Ophthalmol. 2018;66(4):495–505.
40. Quigley HA. 21st century glaucoma care. Eye (Lond). 2019;33(2):254–260.
41. Issa de Fendi L, Cena de Oliveira T, Bigheti Pereira C, Pereira Bigheti C, Viani GA. Additive effect of risk factors for trabeculectomy failure in glaucoma patients: a risk-group from a cohort study. J Glaucoma. 2016;25(10):e879–e883.
42. Romero P, Hirunpatravong P, Alizadeh R, et al. Trabeculectomy with Mitomycin-C: outcomes and risk factors for failure in primary angle-closure glaucoma. J Glaucoma. 2018;27(2):101–107.
43. Pathak-Ray V, Choudhari N. Rescue of failing or failed trabeculectomy blebs with slit-lamp needling and adjunctive mitomycin C in Indian eyes. Indian J Ophthalmol. 2018;66(1):71–76.
44. Bland JM, Altman DG. The logrank test. BMJ. 2004;328(7447):1073.
45. Hosmer D, Lemeshow S, May S. Applied Survival Analysis: Regression Modeling of Time to Event Data.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.