Back to Journals » Risk Management and Healthcare Policy » Volume 11
Stroke prevention in Europe: how are 11 European countries progressing toward the European Society of Cardiology (ESC) recommendations?
Authors Karnad A, Pannelay A , Boshnakova A, Lovell AD, Cook RG
Received 23 January 2018
Accepted for publication 30 May 2018
Published 22 August 2018 Volume 2018:11 Pages 117—125
DOI https://doi.org/10.2147/RMHP.S163439
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Kent Rondeau
Aditi Karnad, Annie Pannelay, Anelia Boshnakova, Alan D Lovell, Robert G Cook
The Economist Intelligence Unit (EIU), London, UK
Purpose: Stroke is a leading cause of death and disability, although studies show that 90% of strokes can be prevented. The evidence base for stroke prevention is well established, and this study aimed to investigate how well European countries are adopting the European Society of Cardiology (ESC) guidelines, particularly toward implementation of the recommended best practice in stroke prevention.
Materials and methods: We developed a stroke prevention scorecard – populated with World Health Organization (WHO) data, secondary research, time-series data, and a survey of 550 physicians – to benchmark 11 European countries in the context of the ESC guidelines.
Results: All countries were found to have policies in place to manage general behavioral risk factors of noncommunicable disease (NCD), but we found that more needs to be done to address cardiovascular disease – specifically, stroke risk factors. Although ten of the countries in this study endorse the ESC cardiovascular clinical guidelines, implementation is lacking. Eight out of the 11 countries received the lowest score in regard to raising awareness around stroke, and 7 countries were found not to have a stroke registry. Among physicians surveyed in primary care it was reported that less than 30% of patients over 40 years old were screened for blood pressure, whereas even fewer were screened for atrial fibrillation; in 10 out of the 11 countries, less than 20% of patients over 65 years old were screened for atrial fibrillation.
Conclusion: Although progress is being made in managing the burden of NCDs, our findings reveal opportunities for improvement in the primary prevention of stroke. Further developments in strategic planning, raising awareness, and monitoring disease are required, as is research on barriers to the implementation of best practice screening of blood pressure and atrial fibrillation in primary care.
Keywords: stroke, risk factors, prevention, benchmarking, screening, clinical practice guideline
Introduction
Over one million people suffer a stroke every year in Europe; by 2025, that figure is estimated to rise to 1.5 million, due to the aging population.1 Although there has been a global trend since the 1990s toward a reduction in stroke incidence, prevalence, and mortality, the overall stroke burden in terms of absolute number of people affected by stroke continues to increase.2
A recent burden of stroke review published in the Lancet reported that ±90% of stroke burden is attributable to modifiable risk factors, including ±75% being due to behavioral factors such as smoking, poor diet, and low physical activity.3 These numbers suggest that achieving control of behavioral and metabolic risk factors could avert more than three-quarters of the global stroke burden.
However, the prevention of stroke is complex – with not only medical but also social and political issues that need to be addressed. Behavioral risk factors for stroke overlap with those associated with other noncommunicable diseases (NCDs), and policies have been enacted in a number of countries to promote healthy diets and increase physical activity, whereas also reducing alcohol consumption and smoking.4,5 Medical risk factors for stroke include atrial fibrillation, diabetes mellitus, hypertension, and high levels of cholesterol. Unrecognized hypertension and atrial fibrillation are particularly significant: hypertension is the leading risk factor for stroke, responsible for nearly half of all ischemic strokes,6 whereas atrial fibrillation is held responsible for 20–30% of cases.7 For these medical risk factors, there needs to be improved monitoring and screening through community-wide, primary-care-led initiatives.5,8
To tie these preventive activities together, several governments around the world have developed national strategies or plans of action to prevent and control NCDs. These plans, which should be routinely updated and monitored for implementation, provide a roadmap for health care systems to address the growing threat of stroke and other cardiovascular diseases (CVDs), cancer, diabetes, and chronic respiratory diseases. Although these plans vary from country to country, the World Health Organization (WHO) recommends that they be concrete and contain objectives, priorities, targets, timetables, and budgets.9
National plans, furthermore, recommend the use of evidence-based guidelines specifically ideally, ones that incorporate primary prevention and patient preferences.8,10,11 In Europe, the European Society of Cardiology (ESC), a not-for-profit medical society, develops recommendations to guide action around the prevention of CVD in clinical practice, including stroke. The guidelines are designed with the aim to support health care professionals and provide tools for integration into national and regional prevention frameworks.7,8,12 They include recommendations around screening for hypertension and atrial fibrillation, monitoring of preventive strategies, and population-level interventions.
How effectively are countries in Europe progressing toward management and promotion of stroke prevention, and is it enough? The aim of this research was to evaluate 11 European countries in terms of their progress toward improving stroke prevention. More specifically, this study explores progress made in the existence of operational national health policies from 2010 to 2016 and in regard to the endorsement and implementation of ESC clinical guideline recommendations by all 11 countries.7,8,12
Materials and methods
This is a retrospective observational study and international comparison of 11 European countries, including an analysis of data from WHO sources and a survey of 550 physicians – 50 in each country.
A review of the literature followed by an editorial advisory board was used to build the scorecard which assessed countries in terms of their stroke prevention activities. Data from the WHO were used to score countries, complemented by information from secondary research. No comparable national data were available for current screening behavior by general practitioners (GPs); therefore, a short survey was conducted. Data were extracted by one author and checked by members of the research team in order to populate the scorecard. The 11 European countries, chosen to represent a broad selection of health systems, were: Belgium, France, Germany, Italy, the Netherlands, Norway, Russia, Spain, Sweden, Turkey, and the UK.
Review of literature and expert consultation
A narrative review of the literature was conducted to support the development of the scoring framework. The PubMed database and gray literature sources were searched to identify relevant cross-country studies, assessment tools, frameworks, and indexes. Supplemental search techniques such as reference harvesting and citation searching in Scopus and Google Scholar were used to identify further research reports from “pearl” articles. The search was pragmatic, iterative, and targeted in scope, and was carried out by a health information specialist.
The review reported on eight frameworks and programs that have previously been used to prioritize policy approaches for the prevention and control of stroke or CVDs in a range of countries. From analysis of these documents, the Economist Intelligence Unit (EIU) outlined a draft set of concepts, domains, and indicators for the scorecard. An editorial advisory board – comprising five stroke experts including academicians, physicians, and policymakers from the UK, US, Italy, People’s Republic of China, and South Africa – met to review and discuss which indicators would be beneficial to include. The board contributed greatly to the development of the scorecard, but did not have final editorial control.
Scorecard
Primary and secondary researches were conducted to develop a scorecard which evaluated different aspects of stroke prevention practices. The full scorecard is described in an EIU briefing paper and contains 16 indicators categorized into four domains: 1) health care system and infrastructure; 2) national NCD plans; 3) addressing CVD and stroke prevention; and 4) tobacco.13 The full scorecard focused on 20 countries globally.
This paper focuses on nine scorecard indicators from the full scorecard – specifically looking at two domains covering clinical and modifiable risk factors of stroke: national NCD policies and plans as well as addressing CVD and stroke prevention in 11 European countries. These nine indicators look at the existence of NCD plans and policies and awareness campaigns, the development of stroke registries, and screening practices for hypertension and atrial fibrillation.
Table 1 shows the indicators used in this research, their scoring guidelines, and data sources. The indicators were split into two categories. “NCD policies and plans” looked at national NCD strategic plans and at policies addressing modifiable risk factors such as diet, physical activity, tobacco, and alcohol consumption.14,15 “Addressing cardiovascular (CVD) prevention” measured initiatives more specific to stroke, such as those recommended in the ESC guidelines: awareness campaigns, stroke registries, and screening for blood pressure and atrial fibrillation.
Primary physician survey
A primary research survey was conducted in association with the field agency Medefield, London, UK, to provide a pragmatic snapshot of current screening activity in primary care. It aimed to find data for the following two indicators, as the two leading risk factors of stroke:
- Hypertension screening – how many patients aged 40 and over are screened for hypertension, who are not already monitored for hypertension? The age limits were determined using recommendations from the National Health Service (NHS) in England.16
- Atrial fibrillation screening – how many patients aged 65 and over are screened for atrial fibrillation, who are not already monitored for atrial fibrillation? The age limit was determined using recommendations outlines in the ESC Guidelines on atrial fibrillation.7
The primary research surveyed 550 physicians – 50 physicians working in general practice in each country – through an online survey to identify the percentage of patients screened for blood pressure and atrial fibrillation. Medefield recruited physicians to complete the online survey who met the screening criteria within their existing clinician database. Physicians were included if:
- they specialized in general practice, primary care practice, or family practice
- they had >3 years of experience in their specialty
- they saw >40 adult patients (18 years and older) in 2 weeks
- they were not employed full-time by a pharmaceutical company or medical diagnosis company in any way other than for clinical trials
Once 50 physicians’ responses were received in each country, data collection was stopped. The physicians were asked questions covering their monitoring and screening practices over the previous 2 weeks. Surveying GPs in this pragmatic manner offered an indicative representation of general practice. The aim was to understand screening practices within everyday practice rather than assessing knowledge in specialists within cardiology.
In order to try and prevent survey respondents from “second guessing” the focus of the research, the survey included questions on a wide range of screening activities. Respondents were asked for information on their use of the following screening measures: weight measurement; blood glucose test; blood pressure measurement; blood cholesterol/lipid test; irregular pulse by palpation and electrocardiogram (ECG). The survey was built in order to discriminate monitoring practices from screening. For each question, GPs were asked about their screening practices for patients 1) with and 2) without preexisting conditions.
Progress toward – and alignment with – ESC guidelines
Progress toward ESC guideline recommendations was assessed using information on the websites of ESC member national cardiac societies that state which ESC clinical guidelines are endorsed by each national society: “ESC Clinical Practice Guidelines endorsed by your National Society”.17
The following ESC guidelines were referred to in this study:
- 2016 European Guidelines on CVD prevention in clinical practice;
- 2013 European Society of Hypertension European Society of Hypertension (ESH)/ESC guidelines for the management of arterial hypertension;
- 2016 ESC Guidelines for the management of atrial fibrillation that was developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS).
The ESC website, however, is unable to indicate whether the national societies implement the guidelines.
Table 2 shows ESC recommendations around CVD prevention, diagnosis, and management of hypertension and atrial fibrillation, as well as around monitoring of preventive strategies and population-level interventions. Using our survey findings, we assessed how the 11 countries are aligned with the recommendations outlined in these guidelines.
Ethics approval and consent to participate
Ethical approval was not required for this survey of health professionals as it was assessed to have no ethical risk. Informed consent to participate in the survey was obtained by the field agency, Medefield, London, UK.
Results
The scorecard provides a snapshot of how countries are progressing and performing in the prevention of NCDs, CVD, and – more specifically – stroke prevention.
Table 3 shows the indicator scores for each country in terms of NCD planning and progress made from 2010 to 2016 using data from the WHO Capacity Survey.14,15 Policies to address NCDs and modifiable risk factors, which can be attributed to several chronic conditions including stroke, were generally found to be in place. Based on the most recent data collected in 2015, seven of the 11 countries included in the study had an operational NCD plan. This was an increase from 2010 to 2013 when five of the countries had NCD plans in place.
Furthermore, there was some progress from 2010 in regard to the more specific policies where ten of the 11 countries included in this study had policies targeting diet and tobacco use, and eight of the 11 countries had a plan for physical activity. This number increased in 2013 when ten of the 11 countries had policies for all three lifestyle factors. In 2015, all 11 countries had policies around healthy diets, physical activity, and tobacco use, and ten countries had alcohol consumption policies. The number of countries with an alcohol consumption policy increased from eight to ten between 2013 and 2015. Nine countries had implemented an alcohol policy in 2010.
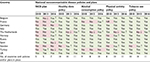
Table 4 shows the indicator scores for each country in regard to addressing CVD prevention, alongside which countries have endorsed each of the ESC guidelines referred to in this study. The principal finding highlighted by this category is the significant room for improvement around CVD- and stroke-specific initiatives in all 11 countries.
  | Table 4 Endorsement of ESC clinical guidelines and implementation of cardiovascular and stroke-specific prevention initiatives. Country assessment Notes: *As indicated on ESC member national cardiac society websites. Yes/no shows whether or not the national society has endorsed the ESC clinical practice guideline.17 #% of patients screened as described in Table 1. ∞The UK registry covers England, Northern Ireland, and Wales; however Scotland has its own stroke registry. Abbreviation: ESC, European Society of Cardiology. |
In 2013, seven of the 11 countries had endorsed the ESC guidelines on management of arterial hypertension and, in 2016, only eight of the 11 countries had endorsed recommendations around the management of atrial fibrillation. However, ten countries had endorsed, and continue to endorse, the 2016 ESC guidelines on CVD prevention in clinical practice that cover aspects of both the hypertension and atrial fibrillation guidelines. Five of the 11 countries – Belgium, France, Russia, Spain, and Turkey – have endorsed all three guidelines.
Two indicators reported on the findings from the primary survey of 550 GP screening practices for hypertension and atrial fibrillation. Less than 30% of patients aged 40 and older in GP clinical practice settings were screened for blood pressure in all 11 countries; in two countries, 10% or fewer patients were screened; in five countries, 11–20% of patients were screened, leaving four countries screening 20–30% of patients. The numbers of patients being screened for arrhythmias, specifically atrial fibrillation, were even less. Except for Russia, in which 42% of patients were screened, less than 20% of patients were screened for AF in the remaining ten countries. In two countries, physicians were screening less than 10% of patients.
Only four out of the 11 countries have stroke registries as part of their health information reporting systems; three countries have one stroke registry, and one country has two.
Eight countries received the lowest scoring in regard to initiatives to raise stroke awareness, having not observed World Stroke Day in 2016 or not having a stroke support organization affiliated with the World Stroke Organization. Only two countries received the top score, highlighting the need for increased awareness around stroke in the general population.
Discussion
Our findings suggest that progress is being made in regard to adoption of national-level policies and endorsement of evidence-based ESC clinical guidelines, but more can still be done to prevent stroke in regard to their implementation.
Several global organizations have focused on addressing NCDs (e.g. the WHO’s Global Action Plan for the Prevention and Control of NCDs 2013–2020 and the United Nations’ Sustainable Development Goals).18 We investigated the progress achieved by 11 European countries toward adoption of NCD policies. An area where we found room for improvement is the development of NCD plans or national strategies. Despite the increased interest from international organizations, a number of countries remain without an overall strategic plan to minimize and manage the burden of stroke and other NCDs. On the positive side, for the 11 countries in this study, the number of operational plans or strategies has increased: from five out of 11 countries to seven countries, between 2010 and 2015. In the past, NCDs were not necessarily a priority in the broader national agenda; however, as can be seen from our findings, this is changing. NCD plans are important; by acting as catalysts for further action, they are able to gain attention and commitment from governments, triggering funding and a road to implementation. Although Table 3 shows that Spain responded “no” to the WHO Capacity Survey in 2016 for existence of an NCD plan, Spain adopted a national NCD strategy (National Strategy for Addressing Chronicity in the National Health System) in June 2012 that was to operate between 2013 and 2020.
Plans also need to address the unhealthy behaviors of people including tobacco use, unhealthy diets, insufficient physical activity, and the harmful use of alcohol. Policies addressing modifiable risk factors are generally operational across the European region; this was already the case in 2010, and the 2015 figures build on that. National plans and any recommendations that stem from them are instrumental in having a positive impact on the burden of disease. For example, a 2017 study published in the Lancet showed an increase in the implementation of key tobacco control measures between 2005 and 2014 in 126 countries and found that, during the same time-frame, the mean smoking prevalence decreased by 2.55%.19 The ESC guidelines note that the advantage of having a population-wide approach to NCDs is the ability to address cardiovascular risk over a lifetime. Individual behavior is influenced by several factors – most obviously, an individual’s environment such as family influence, workplace, health care, and policy at both state and international levels. Still, influencing behavioral change at individual level can be challenging.8 These figures highlight room for improvement around changing individual behavior and the need for further efforts in the implementation of initiatives at ground level.
In addition to policies, a multifactorial approach toward stroke prevention is needed on the ground, such as through the presence and implementation of several initiatives that tackle both behavioral and clinical risk factors. Using the background that all of the 11 countries included in this study endorse at least one of the three previously mentioned ESC guidelines, we discuss our findings in the context of those recommendations.
Hypertension is a major risk factor for stroke.6 High blood pressure usually does not manifest with specific signs or symptoms and, therefore, goes unnoticed by many individuals. However, it has, for example, been recommended by the UK’s NHS that healthy adults over the age of 40 years should have their blood pressure checked once every 5 years and, if at increased risk, it is to be conducted annually.16 The ESC Guidelines on arterial hypertension recommend routine office blood pressure tests for the screening and monitoring of hypertension stating that diagnosis should be based on at least two measurements per visit and on at least two visits.8,12 Seven of the 11 countries endorsed these guidelines in 2013 and continue to do so; yet, our findings suggest that the recommendations are not being undertaken in clinical practice.
Furthermore, the ESC recommends that all hypertensive patients undergo palpation of the pulse at rest to determine heart rate and to search for arrhythmias – especially, atrial fibrillation.12 The guidelines on the management of atrial fibrillation further recommend opportunistic screening for silent atrial fibrillation in all individuals aged 65 years and over – either via pulse palpation or ECG measurements – and suggest systematic screening in patients over the age of 75 years or in those at high risk.7 There is growing concern around this topic because undiagnosed atrial fibrillation is common in older patients and there are also a growing number of patients who are only diagnosed with “silent” atrial fibrillation after having suffered a stroke. A recent systematic review found that almost a quarter of stroke patients are newly diagnosed with atrial fibrillation during cardiac monitoring following a stroke or transient ischemic attack (TIA).20 Additionally, a 2014 Swedish study showed that approximately 33% of patients with ischemic stroke had been either previously or newly diagnosed with atrial fibrillation.21
However, similar to our findings on screening of blood pressure, we found that screening for atrial fibrillation is not being carried out as recommended although eight of the 11 countries endorse this clinical guideline. Russia had much higher screening rates for atrial fibrillation than other countries – potentially, as a result of the 2006 governmental National Priority Project, Health, which has introduced free screening of risk factors and preventive counseling in primary care. This was followed by implementation of a vascular program from 2008 to 2011 that had a more specific focus on CVD and stroke.22
Our study findings, however, are not without precedent. Recommended procedures are rarely followed in health care on a routine basis, citing potential reasons such as lack of information, training, and time.23 More specifically, it has been found that almost all GPs and physicians are aware of the European guidelines addressing CVD prevention but, only 36–57% use them in clinical practice.8 GPs reported that the main reasons for this were that they tend to base advice on their own experiences, that guidelines have unrealistic targets around risk factor control, and that physicians lack knowledge around comprehensive risk assessment.8 Moreover, previous research has suggested that timely measurement of blood pressure in higher-risk persons may be a better use of time and resources rather than measuring all patients during every office visit. This could be one explanation toward why the number of patients being screened is so low; physicians may be screening patients based on suspected cardiovascular risk.8
National plans should also cover the need for and design of disease registries – another underperforming area in our findings. ESC Guidelines recommend the systematic monitoring of the process of delivery around CVD prevention activities as well as suggesting that patient outcomes be considered.8 Monitoring and surveillance data are crucial for understanding the scale of the stroke burden in each country, in order to highlight potential gaps and inform policy development and national strategies around patient care. It is imperative that health information systems are strengthened in order to improve data collection.24
Initiatives for raising awareness about stroke are thin on the ground. The ESC Guidelines discuss the importance of population-level interventions and the involvement of nongovernmental organizations in promoting awareness; they have the ability to initiate mass media awareness campaigns.8 Disease awareness campaigns are important to educate and empower patients; awareness of risk factors can lead to behavioral change toward a healthier lifestyle – for example, stroke awareness campaigns such as Act FAST (Face–Arms–Speech–Time) in the UK and KNOW STROKE in the US.25,26 Eight out of the 11 countries in our study did not observe World Stroke Day in 2016 or have a stroke support organization affiliated with the World Stroke Organization. Although these scoring criteria are a useful benchmark, we recognize that they do not capture all awareness initiatives.
Strengths and limitations
Our study has strengths and limitations. This study reports on findings from a scorecard constructed using carefully selected indicators to assess initiatives addressing stroke prevention in several countries. Moreover, the country selection represents different regions of Europe and different levels of wealth. Many of our indicators rely on data collected from the WHO. The WHO uses data from the Global Health Observatory (GHO), which follows quality assurance procedures to aid the collection of comparable country data. Data are collected via a global survey called the NCD Country Capacity Survey, wherein a questionnaire is completed by either a national agency or the ministry of health. In order to respond “yes” to the questions, the country had to have sufficient resources and funding available in order to use and implement the policy. However, we appreciate that no data source is perfect; a limitation of using WHO data is that it is reliant on responses from country representatives to their Capacity Survey. Additionally, the data are not able to capture any changes to policies in between surveys. Furthermore, the survey size used as part of the primary research phase is adequate for this type of observational study. We believe that acquiring an average of 50 respondents per country was sufficient, given the overall aim of the survey – which was to provide an insight into how common screening is for hypertension and atrial fibrillation. However, we do acknowledge that physicians recruited for the survey were more likely to be from urban areas due to larger cities having a higher concentration of physicians. It is possible that screening practices differ between urban and rural environments, and between physicians in the wider countries.
Conclusion
The 9 indicators referred to in this paper were used to provide a pragmatic snapshot of the current stroke prevention landscape in 11 European countries, but we believe that the basis of these indicators could be used to create a database to monitor stroke prevention activities on a wider scale with the aim of achieving best practice.13 Though the real figures may vary from our estimates, the estimates are sufficient to gain an understanding of the gap between policy and action on the ground.
It is evident that despite broad endorsement of the ESC guidelines, implementation of these recommendations is still lacking, and more concerted efforts at European, national, and regional levels are needed.
Acknowledgments
This research was funded by Bristol-Myers Squibb and Pfizer. All authors are employees of The Economist Intelligence Unit (EIU) who were paid consultants to Bristol-Myers Squibb and Pfizer in connection with conducting this research and with the development of this manuscript. The sponsors had no role in any of the stages from study design to submission of the paper for publication.
Author contributions
AK, AP, AB, and RGC contributed to conception and design of the work. AK, AP, AB, and RGC analyzed and interpreted the data; ADL contributed to interpretation of the data. AK and ADL drafted the manuscript. All authors critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Disclosure
The authors report no conflicts of interest in this work.
References
Béjot Y, Bailly H, Durier J, Giroud M. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med. 2016;45(12 Pt 2):e391–e398. | ||
Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120(3):439–448. | ||
Feigin VL, Roth GA, Naghavi M, et al; Global Burden of Diseases, Injuries and Risk Factors Study 2013 and Stroke Experts Writing Group. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15(9):913–924. | ||
Pearson TA. Public policy approaches to the prevention of heart disease and stroke. Circulation. 2011;124(23):2560–2571. | ||
Karwalajtys T, Kaczorowski J. An integrated approach to preventing cardiovascular disease: community-based approaches, health system initiatives, and public health policy. Risk Manag Healthc Policy. 2010;3:39–48. | ||
World Heart Federation. Stroke and hypertension [webpage on the Internet]. World Heart Federation; 2017. Available from: https://www.world-heart-federation.org/resources/stroke-and-hypertension/. Accessed July 2, 2018. | ||
Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50(5):e1–e88. | ||
Piepoli MF, Hoes AW, Agewall S, et al; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. | ||
WHO. National noncommunicable diseases policies: National NCD policies, strategies and plans of action [webpage on the Internet]. Geneva: World Health Organization; 2017. Available from: http://www.who.int/ncds/governance/policies/en/. Accessed March 31, 2017. | ||
Ashley SW. Foreword. The need for evidence-based guidelines to direct decisions regarding the appropriateness of our interventions. Curr Probl Surg. 2014;51(5):193. | ||
Montori VM, Brito JP, Murad MH. The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. JAMA. 2013;310(23):2503–2504. | ||
Mancia G, Fagard R, Narkiewicz K, et al; Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–1357. | ||
The Economist Intelligence Unit. Preventing stroke: uneven progress. The Economist Intelligence Unit, 2017. Available from: https://www.eiuperspectives.economist.com/healthcare/policy-approaches-stroke-prevention/white-paper/preventing-stroke-uneven-progress. Accessed November 20, 2017. | ||
WHO. National capacity to address and respond to NCDs (key informant response by country) [webpage on the Internet]. Geneva: World Health Organization. Available from: http://www.who.int/gho/ncd/health_system_response/policy/en/. Accessed November 20, 2017. | ||
WHO. Noncommunicable diseases country profiles 2011 [Internet]. Geneva: World Health Organization. Available from: http://www.who.int/nmh/countries/2011/en/. Accessed October 30, 2017. | ||
NHS Choices. High blood pressure (hypertension) [webpage on the Internet]. London: Department of Health; 2017. Available from: http://www.nhs.uk/Conditions/Blood-pressure-(high)/Pages/Introduction.aspx. Accessed May 11, 2017. | ||
ESC. Member National Cardiac Societies [webpage on the Internet]. Brussels: European Society of Cardiology. Available from: https://www.escardio.org/The-ESC/Member-National-Cardiac-Societies. Accessed November 30, 2017. | ||
WHO. NCD and the Sustainable Development Goals [webpage on the Internet]. Geneva: World Health Organization; 2017. Available from: http://www.who.int/global-coordination-mechanism/ncd-themes/sustainable-development-goals/en/. Accessed May 11, 2017. | ||
Warner KE. Understanding the association between the WHO Framework Convention on Tobacco Control, adoption of tobacco control policies, and reduction in smoking prevalence. Lancet Public Health. 2017;2(4):e158–e159. | ||
Sposato LA, Cipriano LE, Saposnik G, Ruíz Vargas E, Riccio PM, Hachinski V. Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. 2015;14(4):377–387. | ||
Friberg L, Rosenqvist M, Lindgren A, Terént A, Norrving B, Asplund K. High prevalence of atrial fibrillation among patients with ischemic stroke. Stroke. 2014;45(9):2599–2605. | ||
Pogosova N, Sokolova O. Governmental efforts for cardiovascular disease prevention efforts in the Russian Federation. Cardiovasc Diagn Ther. 2017;7(Suppl 1):S48–S54. | ||
Piper MA, Evans CV, Burda BU, et al. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Screening for High Blood Pressure in Adults: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. | ||
WHO. Prevention and control of noncommunicable diseases in the European Region: a progress report. Geneva: World Health Organization; 2014. | ||
NHS Choices. Stroke - Act F.A.S.T [Internet]. Department of Health; 2017. Available from: http://www.nhs.uk/actfast/Pages/stroke.aspx#UAHM5f1XajCOFvrX.97. Accessed March 31, 2017. | ||
National Institute of Neurological Disorders and Stroke (NINDS). Know Stroke. Know the Signs. Act in Time. [webpage on the Internet]. National Institute of Neurological Disorders and Stroke; 2017. Available from: https://stroke.nih.gov/. Accessed March 31, 2017. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.