Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
Statin therapy for preventing cardiovascular diseases in patients treated with tacrolimus after kidney transplantation
Authors Han N, Han SH, Song YK, Kim MG, Kim YS, Kim IW, Oh JM
Received 26 July 2017
Accepted for publication 12 October 2017
Published 21 November 2017 Volume 2017:13 Pages 1513—1520
DOI https://doi.org/10.2147/TCRM.S147327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Nayoung Han,1,* Seung Hee Han,1,2,* Yun-Kyoung Song,1 Myeong Gyu Kim,1 Yon Su Kim,3,4 In-Wha Kim,1,* Jung Mi Oh1,*
1Research Institute of Pharmaceutical Sciences, College of Pharmacy, Seoul National University, Seoul, 2Department of Pharmacy, Asan Medical Center, Seoul, 3Department of Internal Medicine, Seoul National University Hospital, Seoul, 4College of Medicine, Seoul National University, Seoul, Republic of Korea
*These authors contributed equally to this work
Background: Lipid abnormalities are prevalent in tacrolimus-treated patients. The aim of the study was to evaluate the preventive effects of statin therapy on major adverse cardiovascular events (MACE) in patients treated with tacrolimus-based immunosuppression after kidney transplantation (KT), and to identify the risk factors.
Methods: This observational cohort study included adult patients who underwent KT and were treated with tacrolimus. Patients who received any lipid-lowering agents except statins, or had a history of immunosuppressant use before transplantation were excluded. The primary outcome was the adjusted risk of the first occurrence of MACE. The secondary outcomes included the risk of individual cardiovascular disease (CVD) and changes in cholesterol level. Subgroup analyses were performed in the statin-user group according to the dosage and/or type of statin.
Results: Compared with the control group (n=73), the statin-users (n=92) had a significantly reduced risk of MACE (adjusted HR, 0.31; 95% CI, 0.13–0.74). In the Cox regression analysis, old age, history of CVD, and comorbid hypertension were identified as independent factors associated with increased MACE. The total cholesterol levels were not significantly different between the two groups. Subjects with higher cumulative defined daily dose of statins had significantly lower risks of MACE.
Conclusion: Statin therapy in patients treated with tacrolimus after KT significantly lowered the risk of MACE. Long-term statin therapy is clearly indicated in older kidney transplant recipients for secondary prevention.
Keywords: kidney transplantation, tacrolimus, HMG-CoA reductase inhibitors, major adverse cardiovascular events (MACE)
Introduction
It is known that there is higher cardiovascular morbidity in kidney transplant patients and, in particular, increased incidence of angina, compared to in age-matched controls from the general population.1,2 This can be attributed to various risk factors, including conventional risk factors such as age, gender, family history, smoking, and comorbid diseases.3,4 As one of the prominent risk factors, dyslipidemia is a common finding and the prevalence is higher in patients treated with immunosuppressive agents including calcineurin inhibitors.5–7
The HMG-CoA reductase inhibitors, known as statins, have beneficial effects on endothelial function through various anti-inflammatory and immunomodulatory actions as well as lowering cholesterol levels.8–12 This effect has resulted in a reduction in cardiovascular events in transplant recipients treated with cyclosporine,13,14 which is linked with transplant outcomes.15–17 However, previous studies were mostly conducted in patients receiving cyclosporine-based regimens, and there is currently a paucity of evidence supporting the use of statins in patients being treated with tacrolimus-based regimens.18 Tacrolimus-based regimens, the mainstay of immunosuppression in solid organ transplantation medicine, are now used in more than 95% of kidney transplant recipients.19 Although the impact of tacrolimus on lipid profiles is lower than that of cyclosporine,20 both drugs can contribute to hyperlipidemia, resulting in increased risk of cardiovascular disease (CVD).21 Moreover, since the metabolism of tacrolimus is very similar to that of cyclosporine, it is possible that tacrolimus may increase the blood levels of statins, through interaction with the hepatic enzymes of the CYP gene family that are responsible for the metabolization of statins.22,23
We therefore hypothesized that statins may also have benefits in CVD outcomes in patients treated with tacrolimus after kidney transplantation (KT). In addition, the effects of statin therapy may vary depending on the intensity of statins,10 treatment duration,24 and cumulative dose of statins.25,26 Therefore, the aims of this study were to evaluate the preventive effects of statins on the risk of CVD in patients who received tacrolimus-based regimens after KT and identify the factors that affect the incidence of CVD.
Patients and methods
Study design and population
This retrospective observational cohort study was conducted at a single tertiary medical center in the Republic of Korea. In accordance with the 2008 Declaration of Helsinki, the guidelines for Good Clinical Practice, and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines,27 the study protocol was planned and approved by the Ethics committee of Seoul National University Hospital (IRB no C-1504-009-662). Informed consent was waived because of the retrospective nature of the study and because the analysis used anonymous clinical data.
Patients aged 30 to 75 years who had KT from January 2006 through June 2009 at the hospital, and received tacrolimus-based regimens as initial maintenance therapy were screened for inclusion in the study. Statins (simvastatin, lovastatin, pravastatin, fluvastatin, atorvastatin, rosuvastatin, and pitavastatin) in any dosage approved in Korea were included. Patients who used other lipid-lowering agents (eg, fibrates and omega-3 fatty acids) during the follow-up period or had a history of prior use of immunosuppressant agents before transplantation, were excluded from the study. Patients who had no information about the use of statins prior to transplantation were also excluded.
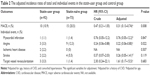
A total of 200 patients were screened, and 165 patients were included. They were classified into two groups, a “statin-user” group (92 patients, 55.6%) and a “statin-naïve” (73 patients, 44.2%) control group. Patient characteristics including age, gender, body mass index (BMI), smoking status, and kidney function were comparable between the two groups at baseline (Table 1). The prevalence of dyslipidemia and mean blood total cholesterol level at the index date were both significantly higher in statin-user group (statin-users vs control: comorbid dyslipidemia, 33.7% vs 4.1%; total cholesterol [mean ± SD], 201.4±37.3 mg/dL vs 174.7±36.6 mg/dL; both P<0.001). The frequency of having a living donor was greater in the statin-user group than in the control group (73.9% vs 49.3%; P<0.001).
  | Table 1 Demographic characteristics of subjects at the index date |
Data collection
Data about comorbid diseases, clinical and laboratory tests, cardiac function, and administered medications were obtained from the patients’ medical records. Comorbidities were identified based on diagnoses recorded within a year before the subject’s index date, including hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease (IHD), myocardial infarction (MI), angina, stroke, thyroid disease, and chronic liver disease.
All patients were followed-up for a maximum of 5 years after the date of cohort entry or index date, which was defined as the earlier date of either hospital discharge or 28 days of admission after KT. Patients whose immunosuppressive regimen was changed from tacrolimus to other immunosuppressive agents at any time during the follow-up period were withdrawn, and the data collected up to that time point were included in the analysis. Statin usage data (medication, dose, schedule, and treatment duration) were collected from 1 year prior to the index date to the end of the study. Any prescription medications taken during the follow-up period were identified, and any that could potentially affect lipid profile or CVD risks, eg, other lipid-lowering agents, anti-hypertensive drugs (including diuretics), diabetes medications, antiplatelet agents, and vitamin K antagonists, were considered as concomitant drugs.
Study outcomes and data analysis
The primary outcome was the first occurrence of major adverse cardiovascular events (MACE), defined as cardiovascular death, MI, angina, IHD, stroke, and target vessel revascularization (TVR).12,28 These events were identified in the medical records by new diagnoses, new treatments such as dual-antiplatelet agents, or other physician notations and records. The secondary outcomes included the incidence of individual cardiovascular events and changes in blood lipid levels. All outcomes were evaluated from the index date up to 5 years in both groups.
Subgroup analyses were performed for the primary outcome in the statin-user group according to either: 1) intensity of the statin therapy based on the American College of Cardiology (ACC)/American Heart Association (AHA) guideline,10 and average percent of LDL-C reduction (high ≥50%, moderate =30% to 50%, and low <30%), or 2) cumulative defined daily dose (cDDD) of statin calculated as Σ (length of continuation period) × (amount of statin a day)/(DDD for the statin).
Statistical analysis
Continuous variables and categorical variables in baseline characteristics were compared using the Student’s t-test and chi-square test, or if linear, by the linear association method (for categories ≥2), respectively. The primary outcome was evaluated using the Kaplan–Meier method and formally tested by the log-rank test for comparison of cumulative incidence for 5 years between the statin-user group and the statin-naïve group. The Cox proportional hazard regression models were used to calculate HR, adjusted for potential confounding factors including age, gender, BMI, smoking status, dialysis type and duration before KT, any history or presence of CVDs, use of concomitant drugs, and level of total cholesterol over the course of time. The final model was determined using the forward selection process in multivariate analysis, in which all covariates were included that had a level of significance 0.05 or less in the univariate analysis. Changes in the blood lipid profile for total cholesterol were analyzed using the linear mixed model at each annual time point after KT, depending on the use of statins at every time. A two-sided P-value of ≤0.05 was considered statistically significant. Statistical analyses were conducted with SPSS software (version 24.0; IBM Corporation, Armonk, NY, USA).
Results
Characteristics of the study population
During the study follow-up period, only three deaths occurred in the two groups, one from graft rejection and two from opportunistic infections. No cardiovascular deaths occurred during the 5-year follow-up period. In the 92 statin-users, the median (range) time to start statins from the index date was 202 (0–1,772) days and the median (range) duration of statin therapy was 1,146 (28–1,825) days. Median (range) cDDD was 985 (8–2,435) days. During this period, use of moderate intensity statins was most common (59.3%), followed by high intensity (33.3%) and low intensity statins (7.3%) (data not shown).
Association between statin therapy and MACE
The total cumulative incidence of MACE over 5 years was 15.2% (n=25), of which ten subjects (10.9%) were in the statin-user group and 15 subjects (20.5%) in the control group, respectively (P=0.059) (Table 2). After adjustment for confounding factors in the regression models, statin therapy was significantly associated with a lower risk of MACE (adjusted HR: 0.31; 95% CI: 0.13–0.74) (Figure 1). The Kaplan–Meier analysis showed that MACE were somewhat delayed in the statin-user group compared to the controls, but this trend was not significant.
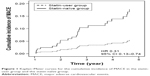  | Figure 1 Kaplan–Meier curves for the cumulative incidence of MACE in the statin-user group and the statin-naïve group. |
Of the total events (n=25), angina was the most common (n=12) and there were significantly fewer cases among statin-users (statin-user vs control: 3.3% vs 12.3%; P=0.022) (Table 2). A significantly lower risk of angina was observed in the statin-user group (adjusted HR: 0.22; 95% CI: 0.06–0.80). However, none of the other individual events except for angina, were significantly different between the two groups (Table 2). MI occurred in one patient in each group. IHD was observed only in the statin-user group and statistical significance could not be assessed. Strokes occurred in two subjects (2.2%) in the statin-user group and four subjects (5.5%) in the control group during the follow-up period. Although the incidence of TVR was three times more in the statin-user group, the difference was not statistically significant.
Independent factors associated with MACE
The risk factors for MACE by the Cox proportional hazards regression model are listed in Table 3. In the univariate analysis, age ≥60 years, dialysis of 5 or more years’ duration before KT, history of CVD, and comorbid hypertension or diabetes mellitus were found to be associated with MACE. However, gender, BMI, smoking, and total cholesterol levels at baseline did not significantly affect the incidence of MACE. On the multivariable analysis, independent predictors of MACE were age ≥60 years (HR: 5.81; 95% CI: 1.09–31.01) and history of CVD (HR: 5.76; 95% CI: 2.24–14.77). Although the initial univariate analysis suggested that a history of dialysis for more than 5 years, comorbid hypertension, or comorbid diabetes mellitus could be associated with MACE, after the multiple regression analysis they were not significant risk factors (Table 3).
  | Table 3 Cox regression analysis for factors associated with MACE |
There was no significant difference between the two groups as a result of comparing blood pressure and blood glucose control at the time of MACE. In the statin-user group, average ± SD of SBP and DBP were 137.7±11.2 and 77.5±8.4 mmHg, compared with control group (136.6±22.6 and 76.8±13.8 mmHg) (P=0.886 and 0.876, respectively). Furthermore, the HbA1c value at the time of MACE was similar between the two groups (statin-users vs control: 7.4%±1.5% vs 6.4%±1.2%; P=0.198) (data not shown).
Changes in lipid profiles
Total cholesterol levels were higher in the statin-user group than in the control group at all time points after the index date (P<0.001) (Figure 2). During the follow-up period, statin use reduced the total cholesterol levels, by an average (±standard error) of −23.43±2.76 mg/dL, as compared with the mean change of total cholesterol levels in the control group (−6.13±2.28 mg/dL). But, there was no significant difference in the change of total cholesterol levels between the two groups during the follow-up period.
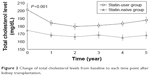  | Figure 2 Change of total cholesterol levels from baseline to each time point after kidney transplantation. |
Subgroup analysis by the patterns of statin usage
The incidence of MACE was 9.09% in the high intensity statin group, 11.3% in the moderate intensity group, and 16.7% in the low intensity group (P=0.59) (Table 4). The statin-user group with greater than median cDDD (higher cDDD group) had a lower risk of MACE than both the statin-user group with less than median cDDD (lower cDDD group) (adjusted HR: 0.17; 95% CI: 0.04–0.87) and the control group (adjusted HR: 0.13; 95% CI: 0.03–0.60). However, there was no significant difference between the lower cDDD group and the control group (adjusted HR: 0.80; 95% CI: 0.33–1.92).
Discussion
This is the first study to identify the preventive effect of statin therapy on tacrolimus induced CVD in kidney transplant recipients. The results demonstrate that statin therapy decreases the incidence of MACE, especially angina, and that the impact was particularly significant, with a high cDDD in the elderly, or patients with a history of CVD and comorbid hypertension.
The presence of CVD history before KT was identified as the most significant risk factor in the multivariate analysis. Among patients treated with tacrolimus after KT, patients with a history of CVD had a 6-fold increased risk of further CVD events. Comorbid hypertension, defined as the use of anti-hypertensive agents during the follow-up period, conferred a 2.5-fold increased risk of CVD in our study. These results are consistent with the Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) which showed that CVD history correlated with an increased incidence of new-onset other CVD as well as 5-year mortality.29 Lloyd-Jones et al30 reported that hypertension contributes to more CVD deaths than any other modifiable cardiac risk factor. And, the study of Prasad et al31 showed that patients with hypertension had a 4.1-fold increase in the risk of MACE (HR: 4.13, 95% CI: 2.16–7.86).
There are several reports stating that statin is effective as secondary prevention in high-risk patients with underlying CVD.8,32 Statins not only reduce the level of LDL-C but also improve endothelial dysfunction,33,34 reduce inflammation,35,36 maintain plaque stability,37 exert antioxidant effects,38 and inhibit thrombus formation.39 Kidney transplant recipients are at high risk for CVD because they have the high prevalence of comorbid diseases (eg, diabetes, hypertension, dyslipidemia) and are exposed to transplant-specific risk factors including the use of immunosuppressive agents, graft function, or infection.40,41 Particularly, tacrolimus-based immunosuppression regimens are still associated with post-transplant metabolic diseases including hypertension, diabetes, and dyslipidemia.42 Thus, statin therapy is a reasonable intervention to consider for reducing the risk of MACE in patients treated with tacrolimus.
Older age (≥60 years) was identified as an independent risk factor of CVD, with those over 60 years old having a 5.8-fold higher risk of incident MACE compared to younger subjects. In the study of Morales et al,43 patients aged 60 years or older had lower survival rates than those under 60 years, with CVD and infections the most frequent cause of mortality. Moreover, the risk of CVD increased by 1.7 times each year in the general population.44 Long-term dialysis is also associated with increased CVD mortality from left ventricular hypertrophy,45 high prevalence of atheromatous plaques,46 and vascular calcifications leading to impaired coronary perfusion.47,48 Because these cardiovascular abnormalities are not reversed by renal transplants, the duration of dialysis before transplantation may be correlated with higher risk of CVD, as has been reported in previous studies.49,50 However, although comorbid diabetes mellitus caused a 1.7-fold increased risk of MACE, this did not prove to be statistically significant, perhaps because of the small size of the sample.
A comparison of statins across the intensity spectrum did not reveal a significant pattern for reducing MACE incidence in our results. But, as an indicator, it appeared that considering both the intensity and duration of statin use together, by examining the cDDD of statins was useful. The higher cDDD of statins in the statin-user group was associated with a significantly lower risk of CVD than that of the statin-naïve subjects. These results are consistent with previous studies that reported that both longer treatment durations and higher potency levels for chronically used statins reduced the risk of CVD.25,26
Our study did not show any significant correlation between the incidence of CVD and changes in lipid profile by statin therapy, although subjects who received statin therapy had the greater reduction rate of total cholesterol compared with control subjects. This may be due to the fact that the cholesterol level remained within the normal range of both groups. These results strongly suggest that cholesterol levels and long-term CVD outcomes are independent.51 Accordingly, the ACC/AHA guideline suggests that reduction in LDL-C can be used as guide to treatment but is not in and of itself a treatment goal.10 The guideline also provided the “fire-and-forget” strategy that focuses on patients’ original risks of CVD other than lipid status, instead of the “target-to-treat” strategy that titrates the medication dosage to reach a specific target lipid level.9,10
There are several concerns to consider when interpreting the findings of our study. First, because this study was performed at a single center, it may not be directly applicable to all other clinical settings. In addition, we included only patients who underwent KT in a single center and were treated with tacrolimus. Because prior to 2006, there were more patients using cyclosporine after transplantation. Nevertheless, the incidence of MACE in the present study was comparable with the results reported previously in the ALERT study.12 Also, we could not evaluate confounding factors such as diet, life style, and smoking status because of the retrospective study design. Third, we could only examine the incidence of MACE for 5 years after KT, but the possible long-term effects on CVD have not been fully investigated. In addition, since no significant change was observed in graft function over 5 years, we could not evaluate the association between statin therapy and graft outcomes. Thus, further prospective, longitudinal, and multicenter studies will be needed to confirm the impact of consistent use of statins on survival and graft outcomes. Finally, we used total cholesterol levels instead of LDL-C because of a limited data set, although LDL-C is the recommended index of dyslipidemia.52 However, since total cholesterol and LDL-C are highly correlated, LDL-C and total cholesterol may be expected to show similar trends with CVD outcomes.
In conclusion, statin therapy in patients with tacrolimus-based treatment after KT was significantly associated with a reduced risk of MACE when considering clinical variables. The reduced risk associated with cDDD may suggest a significant impact of long-term statin therapy on CVD risk. From those findings, the effects of statin therapy should be more evident in patients over 60 years of age or with comorbid hypertension and previous CVD history, and in patients treated as early as possible after renal transplantation.
Acknowledgments
This research was supported by a grant from the Korea Health technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC15C1045).
Disclosure
The authors report no conflicts of interest in this work.
References
Ojo AO, Hanson JA, Wolfe RA, Leichtman AB, Agodoa LY, Port FK. Long-term survival in renal transplant recipients with graft function. Kidney Int. 2000;57(1):307–313. | ||
Aakhus S, Dahl K, Wideroe TE. Cardiovascular morbidity and risk factors in renal transplant patients. Nephrol Dial Transplant. 1999; 14(3):648–654. | ||
Kasiske B, Cosio FG, Beto J, et al. Clinical practice guidelines for managing dyslipidemias in kidney transplant patients: a report from the Managing Dyslipidemias in Chronic Kidney Disease Work Group of the National Kidney Foundation Kidney Disease Outcomes Quality Initiative. Am J Transplant. 2004;4 Suppl 7:13–53. | ||
Ojo AO. Cardiovascular complications after renal transplantation and their prevention. Transplantation. 2006;82(5):603–611. | ||
Badiou S, Cristol JP, Mourad G. Dyslipidemia following kidney transplantation: diagnosis and treatment. Curr Diab Rep. 2009;9(4):305–311. | ||
Deleuze S, Garrigue V, Delmas S, Chong G, Swarcz I, Cristol JP, Mourad G. New onset dyslipidemia after renal transplantation: is there a difference between tacrolimus and cyclosporine? Transplant Proc. 2006;38(7):2311–2313. | ||
Varghese Z, Fernando RL, Turakhia G, et al. Calcineurin inhibitors enhance low-density lipoprotein oxidation in transplant patients. Kidney Int Suppl. 1999;71:S137–S140. | ||
Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta–analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–1278. | ||
Wanner C, Tonelli M; Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014;85(6):1303–1309. | ||
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–2934. | ||
Blanco-Colio LM, Tunon J, Martin-Ventura JL, Egido J. Anti-inflammatory and immunomodulatory effects of statins. Kidney Int. 2003;63(1):12–23. | ||
Holdaas H, Fellstrom B, Jardine AG, et al. Effect of fluvastatin on cardiac outcomes in renal transplant recipients: a multicentre, randomised, placebo-controlled trial. Lancet. 2003;361(9374):2024–2031. | ||
Raggatt LJ, Partridge NC. HMG-CoA reductase inhibitors as immunomodulators: potential use in transplant rejection. Drugs. 2002; 62(15):2185–2191. | ||
Holdaas H, Fellstrom B, Cole E, et al. Long-term cardiac outcomes in renal transplant recipients receiving fluvastatin: the ALERT extension study. Am J Transplant. 2005;5(12):2929–2936. | ||
Kobashigawa JA, Katznelson S, Laks H, et al. Effect of pravastatin on outcomes after cardiac transplantation. N Engl J Med. 1995; 333(10):621–627. | ||
Cosio FG, Pesavento TE, Pelletier RP, Henry M, Ferguson RM, Kim S, Lemeshow S. Patient survival after renal transplantation III: the effects of statins. Am J Kidney Dis. 2002;40(3):638–643. | ||
Johnson BA, Iacono AT, Zeevi A, McCurry KR, Duncan SR. Statin use is associated with improved function and survival of lung allografts. Am J Resp Crit Care. 2003;167(9):1271–1278. | ||
Palmer SC, Navaneethan SD, Craig JC, et al. HMG CoA reductase inhibitors (statins) for kidney transplant recipients. Cochrane Database Syst Rev. 2014(1):CD005019. | ||
Matas AJ, Smith JM, Skeans MA, et al. OPTN/SRTR 2013 Annual Data Report: kidney. Am J Transplant. 2015;15 Suppl 2:1–34. | ||
Margreiter R; European Tacrolimus vs Ciclosporin Microemulsion Renal Transplantation Study Group. Efficacy and safety of tacrolimus compared with ciclosporin microemulsion in renal transplantation: a randomised multicentre study. Lancet. 2002;359(9308):741–746. | ||
Jardine A. Assessing cardiovascular risk profile of immunosuppressive agents. Transplantation. 2001;72(12 Suppl):S81–S88. | ||
Ichimaru N, Takahara S, Kokado Y, et al. Changes in lipid metabolism and effect of simvastatin in renal transplant recipients induced by cyclosporine or tacrolimus. Atherosclerosis. 2001;158(2):417–423. | ||
Asberg A, Hartmann A, Fjeldsa E, Bergan S, Holdaas H. Bilateral pharmacokinetic interaction between cyclosporine A and atorvastatin in renal transplant recipients. Am J Transplant. 2001;1(4):382–386. | ||
McGowan MP; Treating to New Target (TNT) Study Group. There is no evidence for an increase in acute coronary syndromes after short-term abrupt discontinuation of statins in stable cardiac patients. Circulation. 2004;110(16):2333–2335. | ||
Yu O, Eberg M, Benayoun S, Aprikian A, Batist G, Suissa S, Azoulay L. Use of statins and the risk of death in patients with prostate cancer. J Clin Oncol. 2014;32(1):5–11. | ||
Chiu HF, Chang CC, Ho SC, Wu TN, Yang CY. Statin use and the risk of pancreatic cancer: a population-based case-control study. Pancreas. 2011;40(5):669–672. | ||
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. | ||
Kip KE, Hollabaugh K, Marroquin OC, Williams DO. The problem with composite end points in cardiovascular studies: the story of major adverse cardiac events and percutaneous coronary intervention. J Am Coll Cardiol. 2008;51(7):701–707. | ||
Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group, Armitage J, Bowman L, et al. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: a double-blind randomised trial. Lancet. 2010;376(9753):1658–1669. | ||
Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics – 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):e21–e181. | ||
Prasad GV, Huang M, Silver SA, Al-Lawati AI, Rapi L, Nash MM, Zaltzman JS. Metabolic syndrome definitions and components in predicting major adverse cardiovascular events after kidney transplantation. Transpl Int. 2015;28(1):79–88. | ||
Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013(1):CD004816. | ||
Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation. 2000;101(16):1899–1906. | ||
Anderson TJ, Meredith IT, Yeung AC, Frei B, Selwyn AP, Ganz P. The effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotion. N Engl J Med. 1995;332(8): 488–493. | ||
Albert MA, Danielson E, Rifai N, Ridker PM; PRINCE Investigators. Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 2001;286(1):64–70. | ||
Hackman A, Abe Y, Insull W Jr, et al. Levels of soluble cell adhesion molecules in patients with dyslipidemia. Circulation. 1996;93(7): 1334–1338. | ||
Crisby M, Nordin-Fredriksson G, Shah PK, Yano J, Zhu J, Nilsson J. Pravastatin treatment increases collagen content and decreases lipid content, inflammation, metalloproteinases, and cell death in human carotid plaques: implications for plaque stabilization. Circulation. 2001;103(7):926–933. | ||
Sanchez-Quesada JL, Otal-Entraigas C, Franco M, Jorba O, González-Sastre F, Blanco-Vaca F, Ordóñez-Llanos J. Effect of simvastatin treatment on the electronegative low-density lipoprotein present in patients with heterozygous familial hypercholesterolemia. Am J Cardiol. 1999;84(6):655–659. | ||
Furberg CD. Natural statins and stroke risk. Circulation. 1999;99(2): 185–188. | ||
Gill JS. Cardiovascular disease in transplant recipients: current and future treatment strategies. Clin J Am Soc Nephrol. 2008;3 Suppl 2: S29–S37. | ||
Kasiske BL, Umen AJ. Persistent hyperlipidemia in renal transplant patients. Medicine (Baltimore). 1987;66(4):309–316. | ||
Spinelli GA, Felipe CR, Park SI, Mandia-Sampaio EL, Tedesco-Silva H Jr, Medina-Pestana JO. Lipid profile changes during the first year after kidney transplantation: risk factors and influence of the immunosuppressive drug regimen. Transplant Proc. 2011;43(10):3730–3737. | ||
Morales JM, Marcen R, del Castillo D, et al. Risk factors for graft loss and mortality after renal transplantation according to recipient age: a prospective multicentre study. Nephrol Dial Transplant. 2012;27 Suppl 4: iv39–iv46. | ||
Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294(19):2437–2445. | ||
Silberberg JS, Barre PE, Prichard SS, Sniderman AD. Impact of left ventricular hypertrophy on survival in end-stage renal disease. Kidney Int. 1989;36(2):286–290. | ||
Lindner A, Charra B, Sherrard DJ, Scribner BH. Accelerated atherosclerosis in prolonged maintenance hemodialysis. N Engl J Med. 1974; 290(13):697–701. | ||
Ibels LS, Alfrey AC, Huffer WE, Craswell PW, Anderson JT, Weil R 3rd. Arterial calcification and pathology in uremic patients undergoing dialysis. Am J Med. 1979;66(5):790–796. | ||
Hernandez D, Rufino M, Bartolomei S, González-Rinne A, Lorenzo V, Cobo M, Torres A. Clinical impact of preexisting vascular calcifications on mortality after renal transplantation. Kidney Int. 2005;67(5): 2015–2020. | ||
Vanrenterghem YF, Claes K, Montagnino G, Fieuws S, Maes B, Villa M, Ponticelli C. Risk factors for cardiovascular events after successful renal transplantation. Transplantation. 2008;85(2):209–216. | ||
Meier-Kriesche HU, Port FK, Ojo AO, et al. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58(3):1311–1317. | ||
Chawla V, Greene T, Beck GJ, Kusek JW, Collins AJ, Sarnak MJ, Menon V. Hyperlipidemia and long-term outcomes in nondiabetic chronic kidney disease. Clin J Am Soc Nephrol. 2010;5(9):1582–1587. | ||
Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–239. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.