Back to Journals » Nature and Science of Sleep » Volume 11
Sleep inertia: current insights
Authors Hilditch CJ, McHill AW
Received 2 April 2019
Accepted for publication 10 August 2019
Published 22 August 2019 Volume 2019:11 Pages 155—165
DOI https://doi.org/10.2147/NSS.S188911
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sutapa Mukherjee
Cassie J Hilditch,1 Andrew W McHill2
1Fatigue Countermeasures Laboratory, San Jose State University Research Foundation, Moffett Field, San Jose, CA 94035, USA; 2Oregon Institute of Occupational Health Sciences, Oregon Health and Science University, Portland, OR 97239, USA
Correspondence: Andrew W McHill
Oregon Institute of Occupational Health Sciences, Oregon Health and Science University, 3181 SW Sam Jackson Park Road - L606
Portland, OR 97239 USA
Tel +1 503 494 2594
Fax +1 503 494 4278
Email [email protected]
Abstract: Sleep inertia, or the grogginess felt upon awakening, is associated with significant cognitive performance decrements that dissipate as time awake increases. This impairment in cognitive performance has been observed in both tightly controlled in-laboratory studies and in real-world scenarios. Further, these decrements in performance are exaggerated by prior sleep loss and the time of day in which a person awakens. This review will examine current insights into the causes of sleep inertia, factors that may positively or negatively influence the degree of sleep inertia, the consequences of sleep inertia both in the laboratory and in real-world settings, and lastly discuss potential countermeasures to lessen the impact of sleep inertia.
Keywords: cognitive performance, countermeasures, grogginess
Introduction
“ … immediately after getting up, irrespective of the hour, one is not at one’s best,” Kleitman1 observed, in perhaps the earliest known description of sleep inertia in the sleep literature. Sleep inertia is the term used to refer to the temporary time of sleepiness, disorientation and impaired cognitive performance experienced upon awakening.2 Early investigations3–8 of the paradoxical phenomenon of “waking up tired”, although somewhat limited by low participant numbers and methodological design, have had their findings of impaired performance upon awakening supported by a wealth of subsequent, more rigorous studies. Understanding the underlying causes, consequences, and countermeasures to sleep inertia is important for managing this period of impaired performance for those working on-call or napping on-shift who are then required to perform safety-critical tasks soon after waking. The aim of this review is to summarize decades of research that have led to current insights into the following areas of sleep inertia: characterization of neurophysiological correlates; contributing factors influencing severity; neurobehavioral and real-world consequences; and finally, proactive and reactive countermeasures. The review will first define sleep inertia as part of the three-process model of sleep regulation9 and then address each of the topics listed above.
Sleep inertia: the third process of sleep regulation
The propensity for sleep and sleepiness is governed by two main processes: a homeostatic drive or pressure for sleep (Process S), and a circadian rhythm of arousal (Process C).10,11 Process S promotes sleepiness as hours of wakefulness accumulate and is dissipated with time spent asleep. Process C is driven by a circadian pacemaker, the suprachiasmatic nucleus, to promote sleep at night and alertness during the day.12 Thus, the well-accepted two-process model of sleep regulation would theoretically predict higher alertness and performance following depletion of the homeostatic drive, which often coincides with a rise in the circadian drive for alertness following habitual morning awakenings. What is observed at this time, however, is a short, yet salient, decrease in alertness and performance immediately after waking.4–6 Therefore, a third-process (Process W; or Process I, in some descriptions)9 is necessary to better describe these fluctuations in sleepiness. In a three-process model (Figure 1), sleep inertia (green line) is immediately present at sleep offset, briefly counteracting the low homeostatic drive for sleep (red line) and the rising circadian drive for wakefulness (blue line).
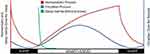 |
Figure 1 A schematic of the three-process model of sleep regulation. |
The exact function of sleep inertia remains largely unknown.13,14 From an evolutionary perspective, one might posit that the ability to rapidly awaken from sleep would be advantageous, for example when awakening in response to a potential threat.13,14 A more gradual awakening, however, may also be protective given the complexity of neural circuitry in transitioning from one state to another,14 as is discussed in the neurophysiology section below. Sleep inertia may, therefore, be an adaptive mechanism to promote sleep upon awakening so that sleep is maintained when the awakening is undesired. For example, as with the timing of the circadian nadir,15 sleep inertia may help to maintain sleep in the later part of a nocturnal sleep episode when homeostatic sleep pressure has largely dissipated. It is only when the restoration of wakefulness needs to be rapid that the process of sleep inertia appears maladaptive. Vyazovskiy et al14 also propose that the gradual awakening following rapid eye movement (REM) sleep may be a “reset” function to minimize hypnopompic intrusions into wakefulness. These theories as to the function of sleep inertia require further research. Animal studies investigating the evolutionary progression of sleep inertia across species may be useful in addressing this gap in the literature. Currently, neurophysiological studies have provided perhaps the best insights into this area, as summarized in the next section.
Neurophysiological basis of sleep inertia
While the transition from sleep to wakefulness has received comparatively little attention relative to the transition from wakefulness to sleep, there is growing evidence for the underlying neurophysiological causes of sleep inertia. For example, spectral analyses of electroencephalography (EEG) after waking have offered insight into the encephalographic substratum of sleep inertia. Compared to pre-sleep wakefulness, post-sleep EEG typically contains higher delta power (associated with deep sleep) and lower beta power (associated with wakefulness).16–19 Reported changes in theta power (associated with drowsiness or REM sleep) have been less consistent.16,17,19 Regional differences in power have also been discovered, with a greater increase in delta waves observed in the posterior regions, which may suggest slower reactivation of these areas after waking.16–18 Further, a recent study by Vallat et al19 assessed the functional connectivity of different brain regions post-awakening and observed that, compared to those waking from lighter N2 sleep (non-REM stage 2 by Rechtschaffen & Kale scoring),20 participants waking from deeper N3 sleep (non-REM Stage 3 and 4) had higher connectivity between the default mode network and brain regions responsible for sensory-motor control and attention. The authors posited that this reduction of functional brain network segregation from the default mode network, which is also observed during sleep and periods of elevated sleepiness,21 may be responsible for the physical and cognitive effects observed during sleep inertia.
Studies of brain activity upon awakening have observed that cerebral blood flow velocity is lower than pre-sleep levels for up to half an hour after waking, reflecting the typical dissipation of cognitive effects.22–24 Additional investigation of these changes discovered brain-region dependent changes, with the prefrontal cortical regions (responsible for executive function) taking longer to return to baseline levels.23,25 Another theory for the neurological basis of sleep inertia came from Van Dongen et al's observation that sleep inertia is suppressed by caffeine consumed just prior to the sleep opportunity.26 Given caffeine acts as an adenosine receptor antagonist, sleep inertia observed following awakenings in sleep restriction scenarios may be partly due to left over adenosine stores that have not been removed during sleep.
While there are few animal studies investigating the transition from sleep to wake, Vyazovskiy et al14 looked at neuronal activity in rodents following spontaneous arousals from sleep. Their study found lower neuronal activity after waking at a population level, but that individual neurons varied, with a subset of neurons being silent for 1 min after waking. Further, the authors observed that neuronal silence was higher following REM sleep compared to waking from non-REM sleep.
Thus, the neurobehavioral impairments observed after waking appear to be due to a delay in transitioning several independent neurophysiological processes and that this transitional lag is most evident in regions related to higher order processes necessary for cognitive tasks.14,16–19,21–26 These transitions could be targeted in the development of novel interventions to enhance the transition from sleep to a fully alert state.
Contributing factors: the influence of sleep and circadian rhythms on sleep inertia
There are several factors influencing the severity and duration of sleep inertia. However, as is discussed at the end of this section, sleep inertia can still occur in the absence of these exacerbating factors.
Waking after prior sleep loss
Sleep inertia is worse under conditions of prior sleep loss. In studies comparing sleep inertia following an 8-h sleep opportunity to partial sleep deprivation, performance upon waking was significantly worse after the partial sleep deprivation night.27,28 Extended wakefulness prior to a recovery sleep episode can also exacerbate the sleep inertia observed following recovery sleep.29,30 In a between-subjects design, Dinges et al30 allocated a 2-h nap to participants after varying durations of prior wakefulness (6, 18, 30, 42 and 54 hrs). Reaction times slowed and the number of correct subtractions decreased as time awake prior to the nap increased. In a within-subjects design, Rosa et al29 also measured performance after a 2-h nap opportunity following either 16 hrs of wakefulness, or up to 64 hrs of wakefulness, with worse performance observed after waking from the nap following 64 hrs. Sleep inertia is also worsened by cumulative sleep loss. Balkin and Badia’s31 observation of increased sleep inertia effects across four nights of disrupted sleep was recently supported by an in-laboratory study in which participants were studied under conditions of chronic sleep restriction (equivalent to sleep opportunities of 5.6 hrs per 24-h day). Notably, compared to a control condition (equivalent to sleep opportunities of 8 hrs per 24-h day), participants undergoing chronic sleep restriction experienced a 10% worsening of performance immediately upon awakening, with average levels of performance failing to reach baseline levels at 70 mins post awakening.32 Together, these studies suggest that sleep loss, in the form of restricted sleep, extended wakefulness, or cumulative sleep loss, contributes to increased sleep inertia effects.
Waking during the night
Sleep inertia effects are greatest during the biological night, near the circadian low in core body temperature.30,33–35 Using a protocol designed to spread behaviors evenly across all hours of the 24-h day (ie, forced desynchrony protocol), Scheer et al33 found that circadian rhythms significantly influenced the number of correct responses on an addition task performed within two minutes of waking. In this study, amplitude in circadian variation observed immediately after waking was greater than that observed at later testing points. This finding suggests that circadian rhythms exert an effect on sleep inertia, independent to its effect on background performance. This effect has also been observed in older participants (>55 y).34
While Scheer et al33 independently assessed the effects of circadian rhythms and sleep pressure on sleep inertia, Dinges et al30 investigated the interaction between the two processes. In their study, participants took a 2-h nap near the peak (approximately 15:00) or trough (approximately 03:00) of the circadian cycle, following varying amounts of prior sleep loss (6–54 hrs of prior wakefulness). This study found that during the peak in alertness, the effect of prior sleep deprivation on sleep inertia appeared to be attenuated. Meanwhile, during the trough, these effects were exacerbated. This interaction between sleep loss, circadian timing, and performance during sleep inertia has also been found under conditions of chronic sleep restriction.32 The results of these studies suggest that circadian rhythms have a direct effect on sleep inertia, and also moderate the effects of sleep deprivation. This interaction creates a non-linear trend in performance as sleep deprivation increases.
Studies designed to systematically assess the impact of circadian rhythms on sleep inertia show clear support for a time-of-day influence, with worse performance immediately after waking during the circadian low. This effect has also been demonstrated to be in addition to circadian effects on background performance and to modulate the influence of homeostatic pressure.
Waking from deep sleep
Mixed observations have been reported on whether the depth of sleep, or the stage of sleep, at awakening has a significant effect on sleep inertia. The increased amount of, and greater propensity to wake from, slow wave sleep (SWS) under conditions of sleep pressure may be associated with the observed increase in sleep inertia following sleep loss. Similarly, the observation that sleep inertia is less likely to occur after short naps (≤30 mins)36–38 may be due to the typical delay in SWS onset of 30 mins.39 This section explores the evidence for and against the influence of SWS on sleep inertia.
Perhaps the most frequently cited evidence for an effect of sleep depth on sleep inertia is Dinges et al's30 study of 2-h naps during 54 hrs of sleep deprivation. Their study measured reaction time by the speed with which participants answered a wake-up phone call and showed that increasing sleep depth was associated with slower response speed. This was particularly evident for awakenings from slow wave Stage 4 sleep (now classified as N3 under the AASM scoring guidelines).40 Furthermore, the amount of SWS during the preceding nap was associated with worse performance on a descending subtraction task performed immediately after answering the phone. Several other studies have also observed sleep stage at awakening as a key predictor of performance impairment upon waking. Stampi41 reported that participants waking from SWS showed a 41% reduction in performance upon awakening compared to performance pre-nap, whereas participants waking from Stage 2 (N2) sleep showed similar performance to those who were already awake. Sleep depth as assessed by power spectral analysis showed that the amount of delta activity (a marker of SWS) in the 10 mins prior to waking from a restricted sleep episode was negatively correlated with performance immediately after waking.27 Further, performance on a decision-making task was significantly worse upon waking from SWS compared to REM sleep.42 Together, the results from the above studies suggest a positive relationship between greater sleep depth and greater sleep inertia.
Many more-recent studies have also found an association between sleep depth and sleep inertia. However, these studies were not necessarily designed to systematically investigate this relationship and therefore rarely support their observations with statistical analysis.36,37,43 In particular, studies of afternoon naps showing that the amount of SWS and the severity of sleep inertia increase with nap length have not confirmed the role of SWS with further analysis.36,37 Regardless of the mechanisms underlying the relationship between greater nap length and greater sleep inertia, these observations lend support to the use of short naps in an effort to minimize sleep inertia.
In contrast, some studies have reported no association between sleep depth33,44,45 or sleep stages at awakening33,45,46 and post-sleep performance. This lack of association has been demonstrated at all times of day under controlled prior sleep–wake conditions.33 and following extended wakefulness during the night and day.45 This lack of association is particularly prevalent in the napping literature (for review see Hilditch et al, 201747).45,48–50 Perhaps the most striking observation comes from Lovato et al48 who, despite 91% of participants waking from SWS and over 50% of the prior sleep period containing SWS, did not observe any performance impairment following a nap taken during a simulated night shift.
The debate in the literature as to whether sleep depth influences sleep inertia may be due to variations in methodologies and definitions of sleep depth. A direct comparison of the studies presented here, however, reveals some common factors that may help to explain the apparent discrepancies. For example, the effects of sleep depth on sleep inertia tend to be observed following longer naps (2 hrs)27,30 compared to shorter naps (20–60 mins),45 and under higher homeostatic pressure27,30 but rarely under reduced homeostatic pressure.27,33,51,52 These studies suggest that the influence of sleep depth on sleep inertia may be mediated by the lengths of both prior wakefulness and prior sleep. From the limited studies reviewed, the effect of time of day does not appear to interact with this relationship;33,44,45 however, its direct influence on sleep inertia33 might still obscure measurement of the direct influence of sleep depth. Thus, interactions with prior sleep–wake factors appear to change the relative influence of sleep depth on subsequent performance, although a direct investigation of these interactions has not been conducted.
Overall, it is difficult to synthesize a clear conclusion as to the role of SWS in sleep inertia. There is long-standing evidence supporting the association between greater sleep depth and greater sleep inertia.27,30,41 This traditional view, however, is now being challenged by more recent literature which suggests that this relationship may not be as robust as initially thought.33,45 Different study designs and measures of sleep depth make it difficult to compare between studies. However, the current literature suggests that the lengths of prior wakefulness and prior sleep may influence the association between sleep depth and sleep inertia.
Impact of contributing factors on sleep inertia duration
The majority of studies examining sleep inertia were not designed to directly assess the duration of sleep inertia and therefore include too few data points to make firm conclusions about the impact of contributing factors on the duration of sleep inertia. In addition, most studies directly observing the time course of sleep inertia have not directly compared contributing factors. One study, however, did directly observe the duration of sleep inertia under two different conditions. Achermann et al's study44 observed that the time course of sleep inertia following an 8-h nocturnal sleep episode and a 2-h evening nap was the same, suggesting that circadian timing and sleep duration under these conditions did not impact duration. Brooks and Lack37 compared four different short, afternoon nap lengths and found that while a 10-min nap resulted in immediate performance improvements, a 30-min nap did not provide improvements until 35 mins or up to 95 mins after waking, depending on the task. This suggests that the duration of sleep inertia is dependent on both length of nap and type of task. Comparing across studies, Hilditch et al38 found that both a 10-min and 30-min nap terminated at 04:00 following acute sleep loss provided no improvements to performance throughout the sleep inertia testing period (up to 60 mins) nor across the remainder of the night (up to 2.5 hrs).53 Taken together, these studies suggest that circadian timing and prior sleep-wake history influence sleep inertia duration as well as severity, although the relative influence of these factors cannot be determined from these observations.
Sleep inertia in the absence of high homeostatic and circadian pressures
While the factors discussed above have been shown to exacerbate sleep inertia effects, it is important to note that sleep inertia has been observed even in the absence of these factors. For example, Wertz et al's54 striking demonstration of the impact of sleep inertia relative to 24 hrs of wakefulness was observed in healthy participants, following an 8-h, habitually-timed sleep opportunity. Similarly, studies have demonstrated sleep inertia effects lasting at least one hour under unremarkable, well-rested conditions.44,51 Results from studies measuring performance and alertness after waking from daytime naps also show signs of sleep inertia, even when the prior night of sleep is unrestricted.44,55 Scheer et al33 demonstrated the circadian influence on sleep inertia magnitude in non-sleep restricted conditions, but also showed that sleep inertia is present, albeit less severe, during times outside of the circadian low. Finally, Hilditch et al50 observed performance impairment immediately following a 10-min nap taken at 07:00 following extended wakefulness, demonstrating that a short nap, depending on the context, does not always avoid sleep inertia. Together, the findings from these studies suggest that sleep inertia is a ubiquitous phenomenon that, while exacerbated by certain factors, can potentially occur at any time.
Consequences: effects of sleep inertia on neurobehavioral outcomes
Despite its relatively short-acting effects, sleep inertia is a notable cause of performance impairment and has been associated with severe, real-world consequences.
Time course of sleep inertia effects
Studies comparing sleep inertia to pre-sleep values have typically shown a return to these levels within 30 mins of awakening36,37,46,48,56 and sometimes as soon as 15 mins after awakening.45,52,57 Studies that have systematically measured alertness and performance across the period after waking, however, report an asymptotic dissipation of sleep inertia.9,44,51 While the initial dissipation of impairment is rapid, full recovery does not appear to be complete until at least an hour after awakening. Jewett et al51 investigated the time course of sleep inertia in a constant routine protocol in which measures of subjective alertness and cognitive throughput were taken regularly from one minute to four hours after scheduled awakening. Under these conditions, Jewett et al51 found, as in the findings of Folkard and Åkerstedt,9 that subjective alertness continued to improve for up to two hours after awakening. Performance impairment on an addition task, however, took up to 3.5 hrs to dissipate.51 These tests were performed following a habitual morning awakening, so the influence of the rise in circadian alertness across this period cannot be extricated from this observation.
Interestingly, subjective alertness recovered faster than objective performance in Jewett et al's51 study, but was slower in Achermann et al's44 study. Achermann et al44 also reported that there was no correlation between objective performance and subjective sleepiness. The difference in time course in performance measures between the two studies may be explained by differences in the tasks performed. However, the desynchronization of time course between subjective and objective measures in both studies highlights a concern when using self-assessment after waking, especially if alertness recovers faster than cognitive performance. Subjective ratings of alertness and performance have been shown to be inconsistent predictors of objective performance under conditions of partial58 and chronic59 sleep loss. Achermann et al's44 study suggests that subjective ratings might also be a poor indicator of performance across the dissipation of sleep inertia. Hilditch et al38 reported a self-rating scale of performance (as opposed to alertness) across the dissipation of sleep inertia and found that despite worse objective performance after waking from a 30-min night-time nap compared to pre-nap, participants rated their performance as significantly better during this period. These findings highlight the need to measure both subjective and objective outcomes when investigating sleep inertia effects. Furthermore, a recent study by Ritchie et al60 suggests that a participant’s morning or evening preference (chronotype) should also be measured when estimating the time course of sleep inertia, with the observation that later chronotypes took longer to recover from sleep inertia than early types.
Comparison of the effects of sleep inertia with the effects of sleep loss
Despite a relatively rapid recovery from sleep inertia in the first 15–30 mins after waking, impairment during this initial period can be equivalent to, or worse than, the effects of sleep loss. For example, Wertz et al54 showed that performance on an addition test immediately after waking was significantly more impaired than after one night of sleep deprivation. Similarly, Miccoli et al28 found no difference in mean response times on a 10-min psychomotor vigilance test (PVT; a simple response time task) for the first hour following a night of sleep deprivation compared to waking from a night of restricted sleep. This indicates that any benefits of the three hours of sleep in the partial sleep restriction condition were masked by sleep inertia for at least an hour after waking. Remarkably, Rosa et al29 found that waking from two hours of recovery sleep following 64 hrs of sleep deprivation was associated with worse performance on both a memory task and auditory reaction time task compared to before the recovery sleep. Performance after waking was also worse than at the same time of day during the prior sleep deprivation period (ie after approximately 41 hrs of wakefulness).
In another study involving 64 hrs of sleep deprivation, a group given 20-min naps every six hours across this period performed worse after waking than the total sleep deprivation group. Furthermore, the sleep inertia experienced after short naps was so intolerable that six participants in the nap condition withdrew from the study, whereas all participants in the sleep deprivation group completed the study.61
Together, the findings from these studies highlight the potential severity of sleep inertia performance deficits relative to extreme sleep loss. Furthermore, these results suggest that, at least in the short term, performance impairment after waking from recovery sleep can actually be worse than the impairment caused by the prior sleep loss itself. Therefore, following prior sleep loss, observable benefits from recovery sleep may be delayed by sleep inertia for up to an hour after waking.
Impact of sleep inertia on different measures of cognitive performance
As the sleep inertia literature expands, a debate has begun as to whether all cognitive tasks are equally affected immediately after waking. Some studies have found that, in contrast to the impairment observed after sleep deprivation, only the reaction time or “speed” component of tasks is negatively affected during sleep inertia.28,46,52,55,61,62 However, several other studies have found equal effects on both speed and accuracy27,31,45 or greater effects on accuracy.63 Variations between studies such as task type, time of testing, instructions to the participants (eg instructed to perform as fast and/or as accurately as possible), and the length and timing of sleep may account for these discrepancies. Two studies have also claimed that, while overall average response speed may slow as a result of sleep inertia, lapses, which represent a substantial delay in response speed, are not a neurobehavioral feature of sleep inertia, but rather are only associated with sleep loss induced microsleeps.28,52
It has also been argued that higher cognitive tasks that require greater attentional load are more susceptible to the effects of sleep inertia than simple tasks.64,65 Studies have reported the effects of sleep inertia on complex cognitive performance tasks such as memory,44 calculations,30,54,65 decision making,42,66 and a spatial-configuration visual search task.65 However, sleep inertia has also been observed using simple reaction time tasks.26,45,62 Conflicting results have also been obtained with regard to effect sizes across different tasks. Santhi et al62 showed the largest effect sizes for simpler tasks such as PVT and a 1-back working memory task compared to a 3-back working memory task. In another study, medium effect sizes were found for moderately complex tasks such as addition and digit-symbol substitution, but the largest effect size was reported for cognitive throughput on a higher-order spatial-configuration task.65 Given the range of methodologies used across these studies, a clear hypothesis for the differential effects observed across tasks has yet to be put forward.
Real-world impacts of sleep inertia
Sleep inertia is a challenge to workers who need to perform safety-critical tasks, make important decisions, or operate a vehicle soon after waking. To this end, several reviews of alertness management in operational settings have highlighted the need to manage sleep inertia in order to maintain safety.64,67–69
While some facets of cognition may be more affected by sleep inertia than others,62,65 real-world tasks often involve a combination of multiple cognitive domains. For example, operating a vehicle safely requires situational awareness, information processing, decision making, memory and, in some instances, rapid response times. Studies of complex psychomotor tasks that better emulate tasks in the real world, for example, a fire management task,42 a military enemy attack exercise,66 or putting on a space suit,8 have all been shown to be susceptible to the effects of sleep inertia. Further, interviews with nurses70 and surveys of emergency service pilots71 have identified sleep inertia as a prevalent issue amongst on-call and night shift workers. In the military, a retrospective analysis of more than 400 US Air Force accidents showed that accidents associated with pilot error were most common during the first hour after waking, suggesting a potential sleep inertia effect.72 Sleep inertia has also been cited as a contributing factor in several commercial incidents across multiple industries which have resulted in damage,73,74 injuries,75 and deaths.76
Taken together, these findings suggest that the effects of sleep inertia on simple, complex, and operational tasks has the potential to negatively impact upon safety-critical activities in the real world.
Countermeasures to sleep inertia
Our knowledge of the factors influencing sleep inertia can help to develop proactive strategies for managing sleep inertia, such as optimal sleep length and timing of awakening. For example, based on the literature summarized above, a planned awakening should take into account as many of the following criteria as possible: limit the duration of the period of wakefulness before the sleep episode; minimize the amount of sleep loss prior to the sleep episode – both acute and chronic; avoid waking during the circadian low in alertness (biological night); and, if waking from a nap, limit sleep duration to less than 30 mins. While following these guidelines can reduce the risk of sleep inertia, as discussed earlier, they do not guarantee a sleep inertia-free wake up. Thus, the most effective proactive countermeasure appears to be caffeine. When taken before a short nap (eg 20 mins), caffeine has been shown to alleviate the symptoms of sleep inertia following the nap.26,77 The limitation of these proactive strategies is that they often require a planned sleep opportunity, a designated wake time, and control over prior sleep-wake history. For many on-call shift workers it is not always feasible to plan the length and timing of a sleep opportunity, and in many cases prior sleep-wake history may be poor. Thus, there is a need for countermeasures that can be implemented upon waking (“reactive” countermeasures).
Hilditch et al78 recently reviewed the literature investigating reactive countermeasures and concluded that there is currently no clear empirical evidence to fully support the use of any reactive countermeasure to provide immediate and objective effects. As mentioned above, when administered before sleep, caffeine has been shown to eliminate the effects of sleep inertia.26 However, there are several limitations to the effectiveness and application of this countermeasure in a reactive scenario. When administered after sleep, even in a rapidly-absorbed chewing gum format, the effects of caffeine are delayed such that while the duration of sleep inertia may be truncated, the initial, most severe period of effects are unaffected by caffeine.79 Furthermore, while caffeine is indeed a field-deployable and operationally viable countermeasure in many cases, the relatively long-lasting stimulant effects may be unwanted in situations in which it is preferable for the worker to fall back asleep within a few hours of waking.80
Other countermeasures such as light, sound, and temperature have been investigated. The outcomes of the trials, however, have been either unsuccessful, or uninterpretable due to methodological limitations such as lack of a control group, not enough testing points, or no evidence of sleep inertia in the control condition.81–86 We below summarize findings of the most commonly investigated countermeasures.
To date, two studies have investigated the use of brief81 and sustained82 light exposure after waking to reduce sleep inertia. Bright light exposure has been shown to directly improve alertness and cognitive performance during the day, night and following sleep restriction.87 Therefore, there is potential for bright light to improve alertness and performance during the sleep inertia period. One study reported a significant improvement to subjective alertness, however, neither study observed a significant improvement on objective performance measures. While these results suggest that both brief and sustained light exposure after waking is of limited effectiveness in reducing sleep inertia effects, it is worth noting that the exposures in these studies were during the day (~07:00 and 13:00). The use of light during nocturnal awakenings may, therefore, have a different effect.
Noise can promote arousal and has previously been shown to attenuate hypo-vigilance during sleep deprivation.88,89 Early investigations on the use of sound to reduce sleep inertia effects have been promising. Tassi et al83 exposed participants to pink noise after a 1-h nap at 01:00 and observed that pink noise eliminated the sleep inertia effect observed in the no-noise group. This effect was less obvious when tested at 04:00. The sleep stage at waking was not controlled in this study and may have contributed to the mixed results at different test times. Hayashi et al84 took a different approach, playing music after waking from a short afternoon nap. While playing music has not been shown to have a long-term alerting effect,90 its short-term effects may be useful in the context of sleep inertia. Indeed, the researchers reported that music reduced subjective sleepiness, and that music preferred by the participants led to improved cognitive performance for up to 20 mins after waking. Sound may be an operationally viable (ie delivered through headphones) and relatively brief and immediate alerting strategy for use in the field.
While the relationship of body temperature to sleep onset has been extensively investigated, its relationship to sleep offset has received less attention. Some studies have shown, however, that changes in the distal-proximal temperature gradient (DPG) after waking correlate with subjective sleepiness.85 This relationship has been demonstrated across different circadian phases in a multi-nap protocol but has yet to be tested with objective performance measures.86 It has been proposed that cooling the extremities immediately after waking may accelerate the DPG changes and, in turn, accelerate recovery from sleep inertia effects. This theory has yet to be tested with an intervention study. Manipulating body temperature may also be a useful deployable strategy, the effects of which may be reversible in situations where a sleep opportunity is presented later in the night.
While there are no studies to our knowledge that have investigated the effectiveness of exercise to reduce sleep inertia effects, anecdotally this is an avenue that may be worthy of research. Sleep inertia is associated with a slow return to waking levels of cerebral blood flow in the anterior cortical regions of the brain;23 therefore, moderate cardiac activity may accelerate this process. Implementation of this strategy would also be relatively convenient in most work place settings.
Given the potential for catastrophic events associated with sleep inertia, the need to develop preventative strategies and reactive countermeasures to minimize both the severity and duration of sleep inertia effects in safety-critical scenarios is crucial.
Summary
As discussed in the previous sections, sleep inertia is characterized by impaired performance and reduced alertness immediately after waking. These effects dissipate asymptotically with the most significant effects occurring within 30 mins of waking. Sleep inertia interacts with the homeostatic and circadian processes to influence performance immediately after waking. Evidence suggests that waking after acute or chronic prior sleep loss, during the circadian low, or from deeper stages of sleep can exacerbate sleep inertia. Sleep inertia is of great importance as the associated performance impairment can be equivalent to, or greater than, that observed after up to 40 hrs of sleep deprivation. Sleep inertia effects have been observed on a range of tasks from simple reaction time tests to complex cognitive tasks. While field studies of sleep inertia are lacking, evidence of sleep inertia in real-world scenarios has been demonstrated in several operational incidents, often with catastrophic consequences. While there is evidence that caffeine can help to reduce the impact of sleep inertia, there is a need for further research into reactive countermeasures that can be deployed in operational scenarios.
Acknowledgment
Dr. Hilditch is supported by a NASA System Wide Safety grant. Dr. McHill is supported by NIH K01HL146992 and the Oregon Institute of Occupational Health Sciences at Oregon Health & Science University. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
Dr. McHill reports speaker honorarium or travel reimbursement fees from the Utah Sleep Research Society and the California Precast Concrete Association. The authors report no other conflicts of interest in this work.
References
1. Kleitman N. Sleep and Wakefulness. Chicago: University of Chicago Press; 1939.
2. Lubin A, Hord DJ, Tracy ML, Johnson LC. Effects of exercise, bedrest and napping on performance decrement during 40 hours. Psychophysiology. 1976;13(4):334–339.
3. Broughton RJ. Sleep disorders: disorders of arousal? Enuresis, somnambulism, and nightmares occur in confusional states of arousal, not in “dreaming sleep”. Science. 1968;159(3819):1070–1078. doi:10.1126/science.159.3819.1070
4. Langdon DE, Hartman B Performance upon sudden awakening. Technical Report SAM-TDR. Brooks AFB, TX: USAF School of Aerospace Medicine; November 1961.
5. Hartman BO, Langdon DE A Second Study on Performance Upon Sudden Awakening. Technical Report SAM-TR-65-61. Brooks AFB, TX: USAF School of Aerospace Medicine; August 1965.
6. Hartman BO, Langdon DE, McKenzie RE A Third Study on Performance Upon Sudden Awakening. Technical Report SAM-TR-65-63. Brooks AFB, TX: USAF School of Aerospace Medicine; August 1965.
7. Webb WB, Agnew H. Reaction time and serial response efficiency on arousal from sleep. Percept Mot Skills. 1964;18(3):783–784. doi:10.2466/pms.1964.18.3.783
8. Seminara JL, Shavelson RJ. Effectiveness of space crew performance subsequent to sudden sleep arousal. Aerosp Med. 1969;40(7):723–727.
9. Folkard S, Åkerstedt T. A three-process model of the regulation of alertness-sleepiness. In: Broughton RJ, Ogilvie RD, editors. Sleep, Arousal, and Performance. Boston: Birkhäuser; 1992:11–26.
10. Borbély AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1(3):195–204.
11. Achermann P. The two-process model of sleep regulation revisited. Aviat Space Environ Med. 2004;75(Supplement 1):A37–A43.
12. Turek F. Introduction: master circadian clock and master circadian rhythm. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine.
13. Peter-Derex L, Magnin M, Bastuji HJN. Heterogeneity of arousals in human sleep: a stereo-electroencephalographic study. NeuroImage. 2015;123:229–244. doi:10.1016/j.neuroimage.2015.07.057
14. Vyazovskiy VV, Cui N, Rodriguez AV, Funk C, Cirelli C, Tononi G. The dynamics of cortical neuronal activity in the first minutes after spontaneous awakening in rats and mice. Sleep. 2014;37(8):1337–1347. doi:10.5665/sleep.3926
15. Dijk D-J, Czeisler CA. Paradoxical timing of the circadian rhythm of sleep propensity serves to consolidate sleep and wakefulness in humans. Neurosci Lett. 1994;166(1):63–68. doi:10.1016/0304-3940(94)90841-9
16. Ferrara M, Curcio G, Fratello F, et al. The electroencephalographic substratum of the awakening. Behav Brain Res. 2006;167(2):237–244. doi:10.1016/j.bbr.2005.09.012
17. Marzano C, Ferrara M, Moroni F, De Gennaro L. Electroencephalographic sleep inertia of the awakening brain. Neuroscience. 2011;176:308–317. doi:10.1016/j.neuroscience.2010.12.014
18. Gorgoni M, Ferrara M, D’Atri A, et al. EEG topography during sleep inertia upon awakening after a period of increased homeostatic sleep pressure. Sleep Med. 2015;16(7):883–890. doi:10.1016/j.sleep.2015.03.009
19. Vallat R, Meunier D, Nicolas A, Ruby P. Hard to wake up? The cerebral correlates of sleep inertia assessed using combined behavioral, EEG and fMRI measures. NeuroImage. 2019;184:266–278. doi:10.1016/j.neuroimage.2018.09.033
20. Rechtschaffen A, Kales A. A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. Los Angeles: Brain Information Service/Brain Research Institute, University of California; 1968.
21. Picchioni D, Duyn JH, Horovitz SG. Sleep and the functional connectome. NeuroImage. 2013;80:387–396. doi:10.1016/j.neuroimage.2013.05.067
22. Hajak G, Klingelhofer J, Schulz-Varszegi M, et al. Relationship between cerebral blood flow velocities and cerebral electrical activity in sleep. Sleep. 1994;17(1):11–19. doi:10.1093/sleep/17.1.11
23. Balkin TJ, Braun AR, Wesensten NJ, et al. The process of awakening: a PET study of regional brain activity patterns mediating the re‐establishment of alertness and consciousness. Brain. 2002;125(10):2308–2319. doi:10.1093/brain/awf228
24. Kuboyama T, Hori A, Sato T, Mikami T, Yamaki T, Ueda S. Changes in cerebral blood flow velocity in healthy young men during overnight sleep and while awake. Electroencephalogr Clin Neurophysiol. 1997;102(2):125–131. doi:10.1016/s0921-884x(96)95054-7
25. Sakai F, Meyer JS, Karacan I, Derman S, Yamamoto M. Normal human sleep: Regional cerebral hemodynamics. Ann Neurol. 1980;7(5):471–478. doi:10.1002/ana.410070514
26. Van Dongen HPA, Price NJ, Mullington JM, Szuba MP, Kapoor SC, Dinges DF. Caffeine eliminates psychomotor vigilance deficits from sleep inertia. Sleep. 2001;24(7):813–819. doi:10.1093/sleep/24.7.813
27. Tassi P, Bonnefond A, Engasser O, Hoeft A, Eschenlauer R, Muzet A. EEG spectral power and cognitive performance during sleep inertia: the effect of normal sleep duration and partial sleep deprivation. Physiol Behav. 2006;87(1):177–184. doi:10.1016/j.physbeh.2005.09.017
28. Miccoli L, Versace F, Koterle S, Cavallero C. Comparing sleep-loss sleepiness and sleep inertia: lapses make the difference. Chronobiol Int. 2008;25(5):725–744. doi:10.1080/07420520802397228
29. Rosa RR, Bonnet MH, Warm JS. Recovery of performance during sleep following sleep deprivation. Psychophysiology. 1983;20(2):152–159.
30. Dinges D, Orne M, Orne E. Assessing performance upon abrupt awakening from naps during quasi-continuous operations. Behav Res Methods. 1985;17(1):37–45. doi:10.3758/BF03200895
31. Balkin TJ, Badia P. Relationship between sleep inertia and sleepiness: cumulative effects of four nights of sleep disruption/restriction on performance following abrupt nocturnal awakenings. Biol Psychol. 1988;27(3):245–258. doi:10.1016/0301-0511(88)90034-8
32. McHill AW, Hull JT, Cohen DA, Wang W, Czeisler CA, Klerman EB. Chronic sleep restriction greatly magnifies performance decrements immediately after awakening. Sleep. 2019;42. doi:10.1093/sleep/zsz032
33. Scheer FA, Shea TJ, Hilton MF, Shea SA. An endogenous circadian rhythm in sleep inertia results in greatest cognitive impairment upon awakening during the biological night. J Biol Rhythms. 2008;23(4):353–361. doi:10.1177/0748730408318081
34. Silva EJ, Duffy JF. Sleep inertia varies with circadian phase and sleep stage in older adults. Behav Neurosci. 2008;122(4):928–935. doi:10.1037/0735-7044.122.4.928
35. Hilditch CJ, Short M, Van Dongen HP, et al. Sleep inertia during a simulated 6-h on/6-h off fixed split duty schedule. Chronobiol Int. 2016;33(6):685–696. doi:10.3109/07420528.2016.1167724
36. Tietzel AJ, Lack LC. The short-term benefits of brief and long naps following nocturnal sleep restriction. Sleep. 2001;24(3):293–300. doi:10.1093/sleep/24.3.293
37. Brooks A, Lack L. A brief afternoon nap following nocturnal sleep restriction: which nap duration is most recuperative? Sleep. 2006;29(6):831–840. doi:10.1093/sleep/29.6.831
38. Hilditch CJ, Centofanti SA, Dorrian J, Banks S. A 30-minute, but not a 10-minute nighttime nap is associated with sleep inertia. Sleep. 2016;39(3):675–685. (in press). doi:10.5665/sleep.5550
39. Gillberg M, Åkerstedt T. The dynamics of the first sleep cycle. Sleep. 1991;14(2):147–154.
40. Iber C, Ancoli-Israel S, Chesson AJ, Quan S; for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Westchester, IL: American Academy of Sleep Medicine (AASM); 2007.
41. Stampi C. The effects of polyphasic and ultrashort sleep schedules. In: Stampi C, editor. Why We Nap: Evolution, Chronobiology and Functions of Polyphasic and Ultrashort Sleep. Boston: Birkhäuser; 1992:137–179.
42. Bruck D, Pisani DL. The effects of sleep inertia on decision-making performance. J Sleep Res. 1999;8(2):95–103.
43. Ferrara M, De Gennaro L, Bertini M. The effects of slow-wave sleep (SWS) deprivation and time of night on behavioral performance upon awakening. Physiol Behav. 1999;68(1–2):55–61. doi:10.1016/s0031-9384(99)00150-x
44. Achermann P, Werth E, Dijk D-J, Borbély AA. Time course of sleep inertia after nighttime and daytime sleep episodes. Arch Ital Biol. 1995;134(1):109–119.
45. Signal TL, van den Berg MJ, Mulrine HM, Gander PH. Duration of sleep inertia after napping during simulated night work and in extended operations. Chronobiol Int. 2012;29(6):769–779. doi:10.3109/07420528.2012.686547
46. Salame P, Otzenberger H, Ehrhart J, et al. Effects of sleep inertia on cognitive performance following a 1-hour nap. Work Stress. 1995;9(4):528–539. doi:10.1080/02678379508256898
47. Hilditch CJ, Dorrian J, Banks S. A review of short naps and sleep inertia: do naps of 30 min or less really avoid sleep inertia and slow-wave sleep? Sleep Med Rev. 2017;32:176–190. doi:10.1016/j.sleep.2016.12.016
48. Lovato N, Lack L, Ferguson S, Tremaine R. The effects of a 30-min nap during night shift following a prophylactic sleep in the afternoon. Sleep Biol Rhythms. 2009;7(1):34–42. doi:10.1111/j.1479-8425.2009.00382.x
49. Kubo T, Takahashi M, Takeyama H, et al. How do the timing and length of a night-shift nap affect sleep inertia? Chronobiol Int. 2010;27(5):1031–1044. doi:10.3109/07420528.2010.489502
50. Hilditch CJ, Dorrian J, Centofanti SA, Van Dongen HP, Banks S. Sleep inertia associated with a 10-min nap before the commute home following a night shift: a laboratory simulation study. Accid Anal Prev. 2017;99:411–415. doi:10.1016/j.aap.2015.11.010
51. Jewett ME, Wyatt JK, Ritz-De Cecco A, Khalsa SB, Dijk D-J, Czeisler CA. Time course of sleep inertia dissipation in human performance and alertness. J Sleep Res. 1999;8(1):1–8.
52. Ikeda H, Hayashi M. The effect of self-awakening from nocturnal sleep on sleep inertia. Biol Psychol. 2010;83(1):15–19. doi:10.1016/j.biopsycho.2009.09.008
53. Centofanti SA, Hilditch CJ, Dorrian J, Banks S. The impact of short night-time naps on performance, sleepiness and mood during a simulated night shift. Chronobiol Int. 2016;33(6):706–715. doi:10.3109/07420528.2016.1167722
54. Wertz AT, Ronda JM, Czeisler CA, Wright KP
55. Hofer-Tinguely G, Achermann P, Landolt HP, et al. Sleep inertia: performance changes after sleep, rest and active waking. Brain Res Cogn Brain Res. 2005;22(3):323–331. doi:10.1016/j.cogbrainres.2004.09.013
56. Tremaine R, Dorrian J, Lack L, et al. The relationship between subjective and objective sleepiness and performance during a simulated night-shift with a nap countermeasure. Appl Ergon. 2010;42(1):52–61. doi:10.1016/j.apergo.2010.04.005
57. Kaida K, Nittono H, Hayashi M, Hori T. Effects of self-awakening on sleep structure of a daytime short nap and on subsequent arousal levels. Percept Mot Skills. 2003;97(3 Pt 2):1073–1084. doi:10.2466/pms.2003.97.3f.1073
58. Biggs SN, Smith A, Dorrian J, et al. Perception of simulated driving performance after sleep restriction and caffeine. J Psychosom Res. 2007;63(6):573–577. doi:10.1016/j.jpsychores.2007.06.017
59. Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi:10.1093/sleep/26.2.117
60. Ritchie HK, Burke TM, Dear TB, McHill AW, Axelsson J, Wright KP
61. Naitoh P, Kelly T, Babkoff H. Sleep inertia: best time not to wake up? Chronobiol Int. 1993;10(2):109–118.
62. Santhi N, Groeger JA, Archer SN, Giménez M, Schlangen LJM, Dijk D-J. Morning sleep inertia in alertness and performance: effect of cognitive domain and white light conditions. PloS One. 2013;8(11):e79688. doi:10.1371/journal.pone.0079688
63. Ferrara M, De Gennaro L, Casagrande M, Bertini M. Selective slow-wave sleep deprivation and time-of-night effects on cognitive performance upon awakening. Psychophysiology. 2000;37(4):440–446.
64. Muzet A, Nicolas A, Tassi P, Dewasmes G, Bonneau A. Implementation of napping in industry and the problem of sleep inertia. J Sleep Res. 1995;4(S2):67–69.
65. Burke TM, Scheer FA, Ronda JM, Czeisler CA, Wright KP. Sleep inertia, sleep homeostatic and circadian influences on higher-order cognitive functions. J Sleep Res. 2015;24(4):364–371. doi:10.1111/jsr.12291
66. Horne J, Moseley R. Sudden early-morning awakening impairs immediate tactical planning in a changing ‘emergency’ scenario. J Sleep Res. 2011;20(2):275–278. doi:10.1111/j.1365-2869.2010.00904.x
67. Rosekind MR, Smith RM, Miller DL, et al. Alertness management: strategic naps in operational settings. J Sleep Res. 1995;4(S2):62–66.
68. Ferrara M, De Gennaro L. The sleep inertia phenomenon during the sleep-wake transition: theoretical and operational issues. Aviat Space Environ Med. 2000;71(8):843–848.
69. Caldwell JA, Prazinko BF, Caldwell JL Fatigue in Aviation Sustained Operations, the Utility of Napping, and the Problem of Sleep Inertia. Report No. RTO-EN-016. Neuilly-sur-Seine Cedex: North Atlantic Treaty Organisation (NATO); 2002.
70. Fallis WM, McMillan DE, Edwards MP. Napping during night shift: practices, preferences, and perceptions of critical care and emergency department nurses. Crit Care Nurse. 2011;31(2):e1–e11. doi:10.4037/ccn2011710
71. Gregory KB, Winn W, Johnson K, Rosekind MR. Pilot fatigue survey: exploring fatigue factors in air medical operations. Air Med J. 2010;29(6):309–319. doi:10.1016/j.amj.2010.07.002
72. Ribak J, Ashkenazi IE, Klepfish A, et al. Diurnal rhythmicity and air force flight accidents due to pilot error. Aviat Space Environ Med. 1983;54(12 Pt 1):1096–1099.
73. Marine Accident Investigation Branch. Heavy Contact by Skandi Foula with OMS Resolution, Aberdeen Harbour 29 May 2010. Accident Report No. 15/2011. London: UK Department for Transport: UK Department for Transport; 2011.
74. Armentrout JJ, Holland DA, O’Toole KJ, Ercoline WR. Fatigue and related human factors in the near crash of a large military aircraft. Aviat Space Environ Med. 2006;77(9):963–970.
75. Transportation Safety Board of Canada. Pitch Excursion: Air Canada, Boeing 767-333, C-GHLQ, North Atlantic Ocean, 55°00ʹN 029°00ʹW, 14 January 2011. Aviation Investigation Report No. A11F0012. Gatineau: Government of Canada; 2011:A11F0012.
76. Government of India Ministry of Civil Aviation. Report on Accident to Air India Express Boeing 737-800 Aircraft VT-AXV on 22nd May 2010 at Mangalore. New Delhi: Government of India; 2010.
77. Gray DM, Banks S, Dorrian J, Munro E, Nielsen J, Centofanti S. Combining caffeine and a nap to improve alertness during a simulated nightshift. Sleep. 2019;42(Supplement 1):A78–A78. doi:10.1093/sleep/zsz067.190
78. Hilditch CJ, Dorrian J, Banks S. Time to wake up: reactive countermeasures to sleep inertia. Ind Health. 2016;54:2015–2236.
79. Newman RA, Kamimori GH, Wesensten NJ, Picchioni D, Balkin TJ. Caffeine gum minimizes sleep inertia. Percept Mot Skills. 2013;116(1):280–293. doi:10.2466/29.22.25.PMS.116.1.280-293
80. McHill AW, Smith BJ, Wright KP. Effects of caffeine on skin and core temperatures, alertness, and recovery sleep during circadian misalignment. J Biol Rhythms. 2014;29(2):131–143. doi:10.1177/0748730414523078
81. Hayashi M, Masuda A, Hori T. The alerting effects of caffeine, bright light and face washing after a short daytime nap. Clin Neurophysiol. 2003;114(12):2268–2278.
82. Santhi N, Groeger JA, Archer SN, Giménez M, Schlangen LJ, Dijk DJ. Morning sleep inertia in alertness and performance: effect of cognitive domain and white light conditions. PloS One. 2013;8(11):e79688. doi:10.1371/journal.pone.0079688
83. Tassi P, Nicolas A, Dewasmes G, et al. Effects of noise on sleep inertia as a function of circadian placement of a one-hour nap. Percept Mot Skills. 1992;75(1):291–302. doi:10.2466/pms.1992.75.1.291
84. Hayashi M, Uchida C, Shoji T, Hori T. The effects of the preference for music on sleep inertia after a short daytime nap. Sleep Biol Rhythms. 2004;2(3):184–191. doi:10.1111/j.1479-8425.2004.00142.x
85. Kräuchi K, Cajochen C, Wirz-Justice A. Waking up properly: is there a role of thermoregulation in sleep inertia? J Sleep Res. 2004;13(2):121–127. doi:10.1111/j.1365-2869.2004.00398.x
86. Kräuchi K, Knoblauch V, Wirz-Justice A, Cajochen C. Challenging the sleep homeostat does not influence the thermoregulatory system in men: evidence from a nap vs. sleep-deprivation study. Am J Physiol Regul Integr Comp Physiol. 2006;290(4):R1052–R1061. doi:10.1152/ajpregu.00381.2005
87. Cajochen C. Alerting effects of light. Sleep Med Rev. 2007;11(6):453–464. doi:10.1016/j.smrv.2007.07.009
88. Wilkinson RT. Interaction of noise with knowledge of results and sleep deprivation. J Exp Psychol. 1963;66(4):332–337.
89. Poulton EC. Arousing environmental stresses can improve performance, whatever people say. Aviat Space Environ Med. 1976;47(11):1193–1204.
90. Reyner LA, Horne JA. Evaluation of “in-car” countermeasures to sleepiness: cold air and radio. Sleep. 1998;21(1):46–50.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
