Back to Journals » Drug, Healthcare and Patient Safety » Volume 13
Self-Medication Practice and Associated Factors Among Health Care Professionals at Debre Markos Comprehensive Specialized Hospital, Northwest Ethiopia
Authors Mohammed SA , Tsega G, Hailu AD
Received 9 November 2020
Accepted for publication 3 February 2021
Published 11 February 2021 Volume 2021:13 Pages 19—28
DOI https://doi.org/10.2147/DHPS.S290662
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Siew Siang Chua
Solomon Ahmed Mohammed,1 Gashaw Tsega,2 Abel Demerew Hailu3
1Department of Pharmacy, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia; 2Department of Pharmacy, Finote Selam General Hospital, Finote Selam, Ethiopia; 3Department of Pharmacy, Dessie Health Science College, Dessie, Ethiopia
Correspondence: Solomon Ahmed Mohammed Tel +251910504378
Email [email protected]
Introduction: Despite self-medication empowers patients in making decisions about the management of minor illnesses independently, the prevalence among health care professionals has sharply increased throughout the world. Self-medication has negative consequences on both the health care professionals themselves and health care delivery. Hence, this study assessed self-medication practices and associated factors among health care professionals at Debre Markos Comprehensive Specialized Hospital.
Methods: A facility-based cross-sectional study was conducted using a structured questionnaire among health care professionals working at Debre Markos Comprehensive Specialized Hospital from October 10 to 25, 2020. A systematic random sampling technique was employed to select 227 study participants. Multivariate logistic regression was computed using the statistical package for social sciences version 20 and variables with a p-value less than 0.05 were taken as statistically significant. Results were presented in the form of tables and graphs.
Results: Among 227 health professional, 164 (72.2%; 95% CI: 66.0%, 77.7%) practiced self-medication. Of these, 107 (65.2%; 95% CI: 57.3%, 71.8%) stated the negative consequence of self-medication. Drug resistance 96 (89.7%) and adverse drug reaction 95 (88.8%) were reported as a consequence. The predictor of self-medication among health professionals was the pharmacy profession (AOR: 11.88, 95% CI (1.38– 102.38)). The most common disease conditions for practicing self-medication were headache 153 (93.3%), respiratory tract infection 116 (70.7%) and gastrointestinal symptoms 103 (62.8%). Pain killers 154 (93.9%), antibiotics 122 (74.4%), and antacid 101 (61.6%) were frequently used for self-medication and health professionals got the medicines from drug retail shops 130 (79.3%) and workplace 104 (63.4%). Mild disease condition 128 (78%), time-saving 124 (75.6%), and accessibility 97 (59.1%) were the reasons for self-medication.
Conclusion: More than two-thirds of health professionals practiced self-medication and reported the negative consequence of self-medication. The predictor of self-medication was the pharmacy profession. The provision of appropriate health education was recommended for promoting rational medication use.
Keywords: self-medication, health professionals, Ethiopia
Introduction
World Health Organization defines self-medication as the treatment of self-diagnosed disorders or symptoms by the use of medicines with the intention that they will be used by consumers on their initiatives and responsibilities.1 It is one of the basic components of self-care, characterized by the use of the drugs by the patient initiative without consulting a medical practitioner.2
Self-medication empowers patients by offering independence in making decisions about the management of minor illnesses.3 Self-medication enables patients in making decisions about the management of their minor illnesses and reduced the pressure on medical services.4 However, illegal providers of drugs along with some practitioners use the practice for the further source of irrational and potentially dangerous drug use.3,5
Self-medication is one component of health care in both developed and developing countries to treat minor ailments that do not require medical consultation.4 Self-medication is an important component of health care,5 and the prevalence has sharply increased throughout the world.6 Now a day, there has been an increasing trend in self-medication with non-prescription drugs.7 For example, in economically deprived countries, like Ethiopia, drugs are dispensed over the counter, and nearly 60–80% of health-related problems are treated through self-medication as a lower-cost alternative.8,9
Self-medication is an essential part of daily self-care and is affected by various factors such as socioeconomic factors, lifestyle, access to drugs, availability of medicinal products,8,10,11 time, and perception of risk of self-medication.12,13 The type and extent of self-medication and the reasons vary from country to country.14,15 In developing countries, self-medication is widely practiced due to poor professional control of pharmaceutical products.16 Health professionals’ knowledge about drugs, diseases, and their health problem was the reasons for self-medication.17 Increase promotion of self-medication products and patient awareness of the availability of products has enhanced self-medication.18
Even if self-medication with non-prescription drugs is universally accepted as an important strategy to alleviate minor ailments, it has negative impacts. The impact of the problem of self-medication practices worsens among health care professionals as it is highly prone to inappropriate use.7,15 Incorrect dosage, prolonged duration of use, wastage of resources, increased resistance to pathogens,18 adverse reactions, incorrect self-diagnosis, delays in seeking appropriate care, drug interactions, risk of dependence, drug abuse,8 and drug toxicity12 were associated with self-medication. A worldwide concern, the emergence of antibiotic-resistant strains of micro-organisms might have been highly augmented by self-medication.19
In Ethiopia, a systematic review and meth analysis revealed that the prevalence of self-medication varied from 12.8% to 77.1%.8 Despite self-medication facilitates better use of clinical skills increases access to medication, and reducing prescribed drug costs associated with publicly funded health programs,3 it has negative consequences on both the health care professionals themselves and the health care delivery.18 In the meantime, the inappropriate practice of self-medication will result in the irrational use of drugs.9 Thus, evaluating and knowing the magnitude and drugs that are consumed is crucial.20 This study assessed self-medication practices and associated factors among health care professionals at Debre Markos Comprehensive Specialized Hospital.
Methods
Study Area and Period
The study was conducted at Debre Markos Comprehensive Specialized Hospital, Debre Markos, Northwest Ethiopia, from October 10 to October 25, 2020. Debre Markos is in the Amhara region, located at a distance of 303 kilometers away from Addis Ababa. The hospital is one of the public hospitals in the region and serves as a referral center for the population of Debre Markos and the adjacent Zones. Currently, the hospital has 465 staff (55 doctors. 232 nurses, 41 pharmacy professionals, 33 laboratory professionals, 44 midwives, 8 radiographers, 8 anesthetists, and 44 other health care professionals).
Study Design
A facility-based cross-sectional study was employed to assess self-medication among health care professionals working at Debre Markos Comprehensive Specialized Hospital.
Population
The source populations were all health professionals working at different units in Debre Markos Comprehensive Specialized Hospital. All health professionals working at Debre Markos Comprehensive Specialized Hospital during the study period and who fulfill the inclusion criteria were considered as the study population.
Inclusion and Exclusion Criteria
All health professionals who were willing to provide consent were included in the study. Health professionals who were not available at the working place during the data collection period due to annual leave, sick leave, and no willingness to give consent were excluded from the study.
Sample Size Determination and Sampling Technique
The sample size was estimated by using a single population proportion formula using 42.4% self-medication prevalence in Dessie referral hospital,21 95% confidence level, and 5% tolerable sampling error. The minimum sample size was 226, and by adding a 10% none response rate, the final sample size was 249.
The sample was taken proportionally from all types of health professions of Debre Markos Comprehensive Specialized Hospital. Then, systematic random sampling (Individuals are taken at regular intervals down the list of health professionals as their list is available at human resource department) was used to select study participants (27 doctors. 113 nurses, 20 pharmacy professionals, 16 laboratory professionals, 21 midwives, 4 radiographers, 4 anesthetists, and 22 other health care professionals) from an eligible list of health professions.
Study Variables
The dependent variable of the study was the prevalence of self-medication, while the independent variables were socio-demographic characteristics of health professionals.
Data Collection Procedure and Quality Assurance
The data were collected using a structured self-administered questionnaire15 after pretested in five percent of the sample size at the Finote Selam general hospital. Then, a small amendment was made based on the results of the pretest. After recruiting and half-day training, data were collected by two druggists who had no working relation to the hospital with the supervision of the principal investigators. Health professional asked their opinion regarding the negative effects of self-medication. After and during data collection, data were checked for completeness, accuracy, and consistency and appropriately arranged and kept in a secured place for compilation and analysis. Cronbach’s alpha test was employed to test the reliability of the questionnaire that assessed types of complaint(s), medications, reason(s) of self-medication and sources of drugs for self-medication and a value of 81.9% was obtained.
Data Processing and Analysis
Data entry and analysis were performed using the Statistical Package for Social Sciences version 20. Each variable was entered into the model one by one and the level of association was checked. Then, variables with a p-value of less than 0.25 in bivariate logistic regression analyses were fitted for multivariate logistic regression. All variables were also entered back into the final model. Crude odds ratios (COR) and adjusted odds ratios (AOR) (95% confidence interval (CI)) were calculated and those variables with a p-value less than 0.05 were taken as statistically significant. The final model fitness was checked to ensure that the model is good. Descriptive data were presented in frequencies, percentages, means, and standard deviation with tables and graphs.
Operational Definition
Self-medication: is the use of medicines without consulting a doctor by one’s initiative or on the advice of another person in the last two months.22
Results
The present study has a 91.1% response rate. Of 227 health professionals, 106 (46.7%) were below 30 years. The mean age was 30.4 with a standard deviation (SD) of 4.3. The minimum and maximum experience ranged from 1 month to 27 years with a mean of 6.6±4.0 years. Nearly one third (36.1%) of health professional had an experience of fewer than 5 years. The majority (60.4%) of health professionals were degree holders. Moreover, 113 (49.7%) of the health professionals were nurses (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Health Care Professionals at Debre Markos Comprehensive Specialized Hospital, 2020 (N=227) |
Health professionals have different patterns of the resort. When they got sick, 54 (23.7%) and 9(4.1%) of health professionals immediately consulted the doctor and traditional healers, respectively, while 164 (72.2%; 95% confidence interval (CI): 66.0%, 77.7%) self-medicated themselves.
When a health professional got sick, they practiced self-medication. The most common disease conditions for practicing self-medication were headache 153 (93.3%), followed by a respiratory tract infection 116 (70.7%), and gastrointestinal symptoms 103 (62.8%). The least self-medication practice was reported for skin (22.6%) and eye diseases (22.6%) (Figure 1).
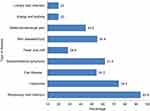 |
Figure 1 Self-medicated disease conditions among health professionals at Debre Markos Comprehensive Specialized Hospital (N=164). |
Of 164 health professionals who practiced self-medication, 154 (93.9%) used pain killers. Antibiotics and antacid were used for self-medication by 122 (74.4%) and 101 (61.6%) health professionals, respectively. Moreover, nearly 55% of health professionals reported the use of medicines for treating cough and parasites (Figure 2).
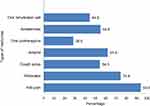 |
Figure 2 Type of medicines used among health professionals at Debre Markos Comprehensive Specialized Hospital, 2020 (N=164). |
The most common reason for practicing self-medication was the disease was mild 128 (78%), followed by time-saving 124 (75.6%) and accessibility 97 (59.1%). Emergency use 90 (54.9%), less expensive 74 (45.1%), and prior experience with the medicine 89 (54.3%) were also the stated reasons for self-medication (Table 2).
 |
Table 2 Reasons for Self-Medication Among Health Professionals at Debre Markos Comprehensive Specialized Hospital (N=164) |
One hundred thirty (79.3%) of the health professionals got the medicines for self-medication from drug retail shops followed by workplace 104 (63.4%), friends 22 (13.4%) and traditional healers 22 (13.4%) respectively. The negative effects of self-medication were based on health professionals’ opinion. Among health professionals (72.2%) who practiced self-medication 107 (65.2%; 95% CI: 57.3%, 71.8%) reported that self-medication has negative consequence. Of these, 88 (82.2%) stated drug dependency as a consequence of health care professionals (Table 3).
 |
Table 3 Consequences of Self-Medication Among Health Professionals at Debre Markos Comprehensive Specialized Hospital (N=107) |
In the bivariate logistic regression analysis, all socio-demographic variables had a p-value of less than 0.25 and were not fitted to multivariate logistics regression analysis. Multivariate logistic regression analysis showed that the only profession of health professionals was significantly associated with self-medication. Pharmacy professionals were nearly 12 folds to practice self-medication than other health professionals like medical laboratory, radiography, anesthesia, environmental health, and health officer (AOR: 11.88, 95% CI (1.38–102.38)) (Table 4).
 |
Table 4 Factors Associated with Self-Medication Among Health Care Professionals at Debre Markos Comprehensive Specialized Hospital |
Discussion
When health professionals got sick, 164 (72.2%; 95% CI: 66.0%, 77.7%) of them practiced self-medication. The finding was consistent with a study conducted in selected hospitals in Ethiopia where 73.4% of health professionals self-medicated themselves.15 The result of the current study was higher than studies conducted in Gonder (54.6%),23 and in line with Nekemte (67.5%),24 but lower as compared to the study done in Addis Abeba 90%,25 Pune 87.5%,17 Nigeria 81.8%26 and Eritrea 93.7%.27 This might be attributed to lower attitude and practice of health professionals on self-medication. The differences could also be due to the country’s drug laws or the electiveness of the drug regulating agencies among countries. A systematic review and meta-analysis of the population-based analysis indicated that healthcare professionals were the main practitioners of self-medication.28 In India, the prevalence of self-medication was highly prevalent (100%) in the healthcare workers, which can influence the other populations to practice self-medication.29
In this study, health professionals most commonly practiced self-medication for headache, respiratory tract infection, and gastrointestinal symptoms. This disease condition was reported by various studies5,23,25 as the main reason for self-medication. The reason was due to higher prevalence of headache, respiratory tract infection, and gastrointestinal symptoms associated with their work and lifestyle. Mild disease condition, time-saving, accessibility, emergency use, less expensive, and prior experience with medicine were a common reason for practicing self-medication by health professionals. These reasons were identified by previous studies.15,25,30 When health professionals got sick, they believed that the illness was mild. On this occasion they trade-off various patterns of resort and demand a time-saving health service. A high patient load in seeking health heath will let health professionals to go to community pharmacy to purchase and use medicines. Most of the community pharmacies are profit oriented and offer the service without requesting prescription and medical diagnosis. This implied that health professionals had imposed their subjective judgment in determining both their diagnosis and treatment.31 Moreover, financial constraints, knowledge of diagnosis, convenience, and non-availability of doctors were the mentioned reasons to self-medicate with modern medicines.8,23,28,32
In the present study, pain killers, antibiotics, antacid, cough, and parasites medications were the most commonly used self-medicated categories of the drug. Health professionals usage of this group of medicines were reported by previous studies.8,15,23,24,28,30,32 This was due to the higher prevalence of disease condition requiring the specified medicines. Because of the lack of knowledge and information, many people take their medication inappropriately which leads to loss of efficacy and inefficient use scares resources.33 Besides, we found that self-medication with antimicrobials was alarmingly high (74.4%). This might be attributed to the usage of antibiotics for every illness and low attitude to antibiotic resistance. The availability of antibiotics without prescription was also high as most of the community pharmacies are striving to incur more profit. The community pharmacies usually offer antibiotics without requesting prescription with a simple verbal request. The use antibiotics as over the counter drug are being promoted because of the poor practice of regulatory agencies and heavy practice of black market.34 Despite health professionals aware of bacterial resistance and the concept of rational drug use, they had used antibiotics without consultation.32,35 Since there is a positive relationship between antibiotic consumption and resistance,36 the implementation of an educational intervention to all health professionals is needed to address self-medication.3,37
Health professionals got their medicines for self-medication from drug retail shops, workplaces, friends, and traditional healers. This is due to the fact that drug retail shops often concerned with client attraction to promote and improve their market value, and continuity of care. Mainly, these drugs were obtained from drug-retail outlets32,35 and the use of self-medication was commonly suggested by pharmacy professionals and friends/relatives.8 There is an increasing trend in self-medication with non-prescription drugs.7 An ethnographic study in India revealed that profit motives of different players located on the drug sales continuum foster medicine sales. Thus, there is a need to be more closely scrutinized for advocating rational drug use.38
Improper use of self-medication has negative consequences on both health care professionals and patients.18 The present study revealed that 65.2% of health professionals aware of the negative consequence of self-medication. Drug dependency, resistance, adverse drug reaction, and worsening of disease condition were the stated consequence. This was attributed to poor attitude of health professionals on their role in rational drug use. Health professionals who practiced self-medication are vulnerable to inappropriate use and resulting in wastage of resources, adverse reactions, delay in seeking appropriate care, drug interactions, incorrect dosage,4 and drug toxicity.6 Inappropriate drug use in self-medication leads to the emergence of antibiotic resistant strains of micro-organisms39 which might have been highly augmented by self-medication.19 Moreover, health professional self-medication enhances patient awareness of the availability of products through the promotion of self-medication products.18 As a result, the impact of the problem of self-medication among the health care profession is severe.7,15
In the present study, only profession was significantly associated with self-medication and pharmacy professionals were nearly 12 folds to practice self-medication than other health professionals (AOR: 11.88). This was attributed to poor attitude, a better access to pharmaceuticals and loose regulatory system. This was in line with Balbisi and Ambiza finding where pharmacists have the greatest access to medications and having an impressive knowledge of prescription drugs and their use in the treatment of various drug therapies increases the potential of self-medication.40 The reason for this wide confidence interval is due to small sample size. The practice of self-medication was also reported to be more prevalent among medical professionals followed by pharmacy and dentistry.7,35 Pharmacy professionals suggested self-medication without formal prescriptions.8 Female sex, age 20–29 years, work experience of <5 years,15 and worked less than 3 years23 were significantly associated with self-medication in previous studies. The difference might be due to differences in socio-demographic characteristics of health professionals, and study design utilized.
Knowing the magnitude and possible reasons responsible for the practice of self-medication among health professionals will help policymakers and implementers to design intervention that focuses on promoting rational drug use. This study has limitations. A causal relationship between the independent and dependent variables cannot be established due to the cross-sectional nature of the study. The study was conducted in a specific context (health professionals working in the public health facilities only), and small sample size. Hence, more studies in different contexts with larger numbers would be helpful to validate the findings. And also the findings in this study may be subjected to recall bias as 2 months recall period was used to collect information. The analyses were also based on self-report (socially acceptable responses by the study participants) of health professional resulting with the possibility of over and under-reporting.
Conclusion
More than two-thirds of health professionals practiced self-medication and stated that self-medication has a negative consequence. The most common disease conditions for practicing self-medication were headache, respiratory tract infection, and gastrointestinal symptoms. Pain killers, antibiotics, and antacids were frequently used for self-medication and health professionals got medicines from drug retail shops, workplaces, friends, and traditional healers. Mild disease condition, time-saving, accessibility, emergency use, less expensive, and prior experience with the medicine were the reasons for self-medication. The predictor of self-medication among health professionals was the pharmacy profession. For promoting rational medication use, awareness creation was recommended for the safe and effective use of medicines.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; SD, standard deviation.
Data Sharing Statement
The datasets are available from the corresponding author upon reasonable request.
Ethical Consideration
Ethical approval was obtained from Ethics Review Committee of the Department of Pharmacy, College of Medicine and Health Sciences, Wollo University (WU Phar/037/13). Then, permission was requested and obtained from Debre Markos Comprehensive Specialized Hospital. Moreover, information concerning the purpose, sampling and importance of the provided and verbal informed consent was obtained from study participants. In this study, verbal informed consent was approved by the ethics review committee and the study was conducted in accordance with the Declaration of Helsinki. Confidentiality of study participants data was maintained throughout the study.
Acknowledgment
The authors would like to acknowledge Mrs Mulu Wondimu for her contribution in manuscript edition.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no potential competing interests in this work.
References
1. WHO. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. World Health Organization; 2000.
2. Jambo A, Mengistu G, Sisay M, Amare F, Edessa D. Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of Harar town, Ethiopia. Front Pharmacol. 2018;9:1063. doi:10.3389/fphar.2018.01063
3. Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Saf. 2001;24(14):1027–1037. doi:10.2165/00002018-200124140-00002
4. Jember E, Feleke A, Debie A, Asrade G. Self-medication practices and associated factors among households at Gondar town, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):1–7. doi:10.1186/s13104-019-4195-2
5. Angamo MT, Wabe NT. Knowledge, attitude and practice of self medication in Southwest Ethiopia. Int J Pharm Sci Res. 2012;3(4):1005.
6. Shafie M, Eyasu M, Muzeyin K, Worku Y, Martin-Aragon S. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One. 2018;13(3):e0194122. doi:10.1371/journal.pone.0194122
7. Ali A, Kion J, Keat C, Dhanaraj S. Self-medication practices among health care professionals in a private university, Malaysia. Int J Curr Pharm. 2012;1(302–310):302–310. doi:10.3329/icpj.v1i10.11846
8. Ayalew MB. Self-medication practice in Ethiopia: a systematic review. Patient Prefer Adherence. 2017;11:401. doi:10.2147/PPA.S131496
9. Befekadu A, Dhekama NH, Mohammed MA. Self-medication and contributing factors among pregnant women attending antenatal care in Ethiopia: the case of Jimma University specialized hospital. Med Sci. 2014;3(1):969–981. doi:10.5455/medscience.2013.02.8098
10. Hailemichael W, Sisay M, Mengistu G. Assessment of knowledge, attitude, and practice of self-medication among Harar health sciences college students, Harar, Eastern Ethiopia. J Drug Deliv Ther. 2016;6(5):31–36. doi:10.22270/jddt.v6i5.1329
11. Abay S, Amelo W. Assessment of self-medication practices among medical, pharmacy, health science students in Gondar University, Ethiopia. J Young Pharm. 2010;2(3):306–310. doi:10.4103/0975-1483.66798
12. Mekuria AB, Erku DA, Gebresillassie BM, Birru EM, Tizazu B, Ahmedin A. Prevalence and associated factors of herbal medicine use among pregnant women on antenatal care follow-up at university of gondar referral and teaching hospital, Ethiopia: a cross-sectional study. BMC Complement Altern Med. 2017;17(1):86. doi:10.1186/s12906-017-1608-4
13. Afshary P, Mohammadi S, Najar S, Pajohideh Z, Tabesh H. Prevalence and causes of self-medication in pregnant women referring to health centers in southern of Iran. Int J Pharm Sci Res. 2015;6(2):612. doi:10.13040/IJPSR.0975-8232.6(10).4103-12
14. Abula T, Worku A. Self-medication in three towns of north west Ethiopia. Ethiop J Health Dev. 2001;15(1).
15. Fekadu G, Dugassa D, Negera GZ, et al. Self-medication practices and associated factors among health-care professionals in selected hospitals of western Ethiopia. Patient Prefer Adherence. 2020;14:353. doi:10.2147/PPA.S244163
16. Abasiubong F, Bassey EA, Udobang JA, Akinbami OS, Udoh SB, Idung AU. Self-medication: potential risks and hazards among pregnant women in Uyo, Nigeria. Pan Afr Med J. 2012;13(1).
17. Sajith M, Suresh SM, Roy NT, Pawar D. Self-medication practices among health care professional students in a tertiary care hospital, Pune. Open Public Health J. 2017;10(1):63–68. doi:10.2174/1874944501710010063
18. Kumar V, Mangal A, Yadav G, Raut D, Singh S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J DY Patil Univ. 2015;8(1):16. doi:10.4103/0975-2870.148828
19. Gutema GB, Gadisa DA, Kidanemariam ZA, et al. Self-medication practices among health sciences students: the case of Mekelle University. J Appl Pharm Sci. 2011;1(10):183.
20. Banzal N, Saxena K, Dalal M. Research publications. Int J Basic Clin Pharmacol. 2017;6(4):924–927. doi:10.18203/2319-2003.ijbcp20171105
21. Baye A, Sada O. Self-medication practice in community pharmacies: the case of Dessie town, Northeast Ethiopia. Adv Pharmacoepidemiol Drug Saf. 2018;7(1):1–3.
22. Hernandez-Juyol M, Job-Quesada J. Dentistry and self-medication: a current challenge. Med Oral. 2002;7(5):344.
23. Simegn W, Dagnew B, Dagne H. Self-medication practice and associated factors among health professionals at the university of gondar comprehensive specialized hospital: a cross-sectional study. Infect Drug Resist. 2020;13:2539. doi:10.2147/IDR.S257667
24. Sado E, Kassahun E, Bayisa G, Gebre M, Tadesse A, Mosisa B. Epidemiology of self-medication with modern medicines among health care professionals in Nekemte town, western Ethiopia. BMC Res Notes. 2017;10(1):533. doi:10.1186/s13104-017-2865-5
25. Belete T, Berhanu Z. Self-medication practice among health care professionals and its effect on patients or clients at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia; 2017. Available from: http://213.55.95.56/bitstream/handle/123456789/2716/Tigist%20Belete.pdf?sequence=1&isAllowed=y.
26. Esan DT, Fasoro AA, Odesanya OE, Esan TO, Ojo EF, Faeji CO. Assessment of self-medication practices and its associated factors among undergraduates of a private University in Nigeria. J Environ Public Health. 2018;2018:1–7. doi:10.1155/2018/5439079
27. Tesfamariam S, Anand IS, Kaleab G, et al. Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health. 2019;19(1):159. doi:10.1186/s12889-019-6470-5
28. Sisay M, Mengistu G, Edessa D. Epidemiology of self-medication in Ethiopia: a systematic review and meta-analysis of observational studies. BMC Pharmacol Toxicol. 2018;19(1):56. doi:10.1186/s40360-018-0248-8
29. Hanumaiah V, Manjunath H. Study of knowledge, attitude and practice of self medication among health care workers at MC gann teaching district hospital of Shivamogga, India. Int J Basic Clin Pharmacol. 2018;7(6):1174–1181. doi:10.18203/2319-2003.ijbcp20182102
30. Shaghaghi A, Asadi M, Allahverdipour H. Predictors of self-medication behavior: a systematic review. Iran J Public Health. 2014;43(2):136.
31. Dabney DA, Hollinger RC. Illicit prescription drug use among pharmacists: evidence of a paradox of familiarity. Work Occup. 1999;26(1):77–106. doi:10.1177/0730888499026001005
32. Babatunde OA, Fadare JO, Ojo OJ, et al. Self-medication among health workers in a tertiary institution in South-West Nigeria. Pan Afr Med J. 2016;24.
33. Atsbeha BW, Suleyman SA. Medication knowledge, attitude and practice (kap) among university of gondar freshman students, north western ethiopia. Pharmacologyonline. 2008;1:4–12.
34. Haque M, Rahman NAA, McKimm J, et al. Self-medication of antibiotics: investigating practice among university students at the Malaysian National Defence University. Infect Drug Resist. 2019;12:1333–1351. doi:10.2147/IDR.S203364
35. Sharif SI, Bugaighis LM, Sharif RS. Self-medication practice among pharmacists in UAE. Pharm Pharmacol. 2015;6(09):428. doi:10.4236/pp.2015.69044
36. Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14(1):13. doi:10.1186/1471-2334-14-13
37. Awad A, Ball D, Eltayeb I. Improving rational drug use in Africa: the example of Sudan. East Mediterr Health J. 2007;13(5):1202–1211. doi:10.26719/2007.13.5.1202
38. Kamat VR, Nichter M. Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Soc Sci Med. 1998;47(6):779–794. doi:10.1016/S0277-9536(98)00134-8
39. Worku S. Practice of self-medication in Jimma Town. Ethiop J Health Dev. 2003;17(2):111–116.
40. Balbisi EA, Ambizas EM. Self-prescribing of noncontrolled substances among pharmacists. Am J Health Syst Pharm. 2005;62(23):2508–2511. doi:10.2146/ajhp050007
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
