Back to Journals » International Medical Case Reports Journal » Volume 15
Ruptured Middle Colic Artery Aneurysm Presenting with Symptoms of Acute Cholecystitis: A Case Report and Literature Review
Authors Johnson GGRJ , Dhaliwal S, Launcelott S, Hyun E, Helewa R , Shariff F, Hochman D
Received 26 April 2022
Accepted for publication 29 October 2022
Published 28 December 2022 Volume 2022:15 Pages 761—768
DOI https://doi.org/10.2147/IMCRJ.S372294
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ronald Prineas
Garrett GRJ Johnson,1,2 Surinder Dhaliwal,3 Sebastian Launcelott,4 Eric Hyun,1 Ramzi Helewa,1 Farhana Shariff,1 David Hochman1
1Department of Surgery, Section of General Surgery, University of Manitoba, Winnipeg, Manitoba, Canada; 2Clinician Investigator Program, University of Manitoba, Winnipeg, Manitoba, Canada; 3Department of Radiology, University of Manitoba, Winnipeg, Manitoba, Canada; 4Department of Surgery, Section of Vascular Surgery, University of Manitoba, Winnipeg, Manitoba, Canada
Correspondence: David Hochman, Department of Surgery, Section of General Surgery, University of Manitoba, 343 Tache Avenue, Winnipeg, Manitoba, R2H 2A5, Canada, Tel +1 204-925-9592, Fax +1 204-231-2283, Email [email protected]
Background: Ruptured middle colic artery aneurysm is extremely uncommon. Diagnosis can be challenging, as symptomatology can be attributed to more common abdominal pathologies. Due to the rarity of this condition, only case reports are available to inform management.
Case Presentation: We present the case of a 72-year-old woman with a ruptured middle colic artery aneurysm presenting with signs and symptoms more suggestive of acute calculous cholecystitis. Her co-existing bleed was confirmed on CT angiogram. Coil embolization was initially attempted unsuccessfully. She underwent laparotomy, a middle colic artery ligation, and extended right hemicolectomy with intra-aortic balloon placement for emergency proximal vascular control. Post-operatively, she had a re-bleed that was successfully managed with covered stent placement in the proximal superior mesenteric artery after an unsuccessful re-attempt at coil embolization. Her apparent associated cholecystitis was managed with antibiotics and resolved uneventfully.
Conclusion: A middle colic artery aneurysm can be challenging to diagnose and treat. Management options include endovascular techniques, open surgery, or a combination approach. Intra-aortic balloon placement for emergency vascular control is a novel approach that could avoid hemorrhage when intra-abdominal vascular access is challenging.
Keywords: middle colic artery, mesenteric aneurysm, endovascular therapy, coil embolization, intra-aortic balloon placement
Introduction
Aneurysms of the vasculature supplying the intra-abdominal viscera are collectively very uncommon.1 Ruptured middle colic artery (MCA) aneurysms are exceedingly rare and represent one of the least common sites of occurrence. Fewer than 30 cases of ruptured MCA aneurysms have been reported in the literature, all with a variety of symptomatology and management strategies employed.2 Classically, emergency laparotomy was performed with arterial ligation and resection of the affected colon. However, as familiarity with minimally invasive transcatheter interventional strategies increases, these present a compelling management option for patients stable enough for management in the interventional radiology suite.3 However, due to the rarity of this condition and the varied case presentations and associated symptoms, accurate diagnosis can be a challenge before effective management can be initiated. We report the case of a 72-year-old woman with a ruptured MCA aneurysm, presenting first with signs, symptoms, and ultrasound findings of acute calculous cholecystitis. The purpose of this case report is to highlight how a rare visceral artery aneurysm can be mistaken for a more common abdominal pathology, and to review the management of this rare condition.
Case Presentation
A 72-year-old woman presented to the emergency department with constant and gradually increasing epigastric abdominal pain for the past 10 days. The pain worsened following meals and was associated with nausea and retching. Within the past 24 hours, she had become unable to tolerate significant oral intake, and the pain had migrated to the right upper quadrant of her abdomen. Her medical history is significant for secondary progressive multiple sclerosis (MS) for the past 27 years, treated unsuccessfully at another institution with an experimental bilateral percutaneous transluminal jugular venoplasty 11 years prior. She also has hypertension treated with hydrochlorothiazide, and depression treated with citalopram, but no history of trauma, abdominal surgeries, or cardiovascular disease.
Upon presentation to the emergency department, she appeared quite uncomfortable, although her vital signs were within normal limits with a temperature of 36.5°C, a heart rate of 68 beats/min, blood pressure of 123/71 mm Hg, and an oxygen saturation of 92% on room air. Her abdomen was tender in the right upper quadrant with a positive Murphy’s sign. No abdominal masses were appreciated, and she had no peritoneal signs. She underwent laboratory testing, which demonstrated a leukocyte count of 12,000/μL with 84% neutrophils and a hemoglobin of 10.7 g/dL. Her serum liver enzymes, lipase, and liver function tests were all within normal limits. She underwent abdominal ultrasound, which demonstrated a positive sonographic Murphy’s sign, a 5 mm thickened gallbladder wall, and stones in the gallbladder lumen, but with no pericholecystic fluid or gallbladder distension. She had an incidental note of a complex cystic lesion seen in the left upper quadrant felt to be dilated bowel; however, bowel gasses obscured the pancreas and aorta (Figure 1). She was initially diagnosed with acute calculous cholecystitis, but an abdominal computed tomography (CT) was requested, given the unexpected finding in her left upper quadrant. The CT scan revealed a large hematoma (20 cm diameter) in the mid-abdomen adjacent to the pancreas and transverse colon mesentery, associated with a small 1.1×0.6 cm aneurysm of the MCA (Figure 2). No extravasation of contrast was seen and there were no signs of colonic ischemia. Given her clinical stability at this point, an angiogram with embolization of the mesenteric aneurysm was initially attempted through the superior mesenteric artery (SMA). The exact site of the aneurysm could not be reached due to acute angle of the culprit branch. Only proximal coils into small vessels potentially supplying the area were placed (Figure 3).
 |
Figure 1 Sonographic images demonstrating (A) acute calculous cholecystitis with stone visible and (B) a complex cystic structure in the left upper quadrant. |
 |
Figure 2 CT angiogram arterial phase axial view demonstrating a 1.1×0.6cm aneurysm adjacent to the pancreas. |
This was considered an incomplete embolization and as expected, the bleeding continued.
The patient was subsequently taken for urgent laparotomy. Given the size of the hematoma and its status overlying the superior mesenteric artery and supraceliac aorta, an aortic CODA balloon catheter (Cook Incorporated, Bloomington, IN) was positioned (but not deployed) within the distal descending thoracic aorta prior to performing the laparotomy. This was performed as a safeguard in case emergent proximal aortic control was required and to minimize the extent of hemorrhage in the event of exsanguination. Within her upper abdomen, a large, contained hematoma was identified at the root of the transverse colonic mesentery. The left and right colon were fully mobilized, and the transverse colon was divided to facilitate access to the aneurysm. The haematoma cavity was entered, the clot was evacuated, and the bleeding MCA was identified and ligated. No further bleeding was identified, and the endovascular balloon was never inflated. At this point, a large section of the transverse and distal ascending colon appeared ischemic, requiring extended right hemicolectomy, leaving the descending and sigmoid colon intact. Throughout the operation, the patient remained hemodynamically stable, so a stapled ileocolic anastomosis was performed without fecal diversion. Of note, there were some adhesions to the gallbladder, however the gallbladder itself appeared grossly normal, and was left in situ.
Post-operatively, 24 hours after her operation, the patient had a sudden rise in her heart rate to 100 beats/min and a drop in her hemoglobin to 6.0 g/dL. She was emergently resuscitated with blood products, and underwent a repeat CT angiogram, which demonstrated the persistence of her MCA aneurysm, just proximal to the site of ligation during her operation (Figure 4). She underwent repeat angiography through the SMA, which demonstrated two remaining branches of the MCA, one supplying the bleeding aneurysm, which had been ligated distally during the preceding laparotomy. Due to their tortuosity, these branches were difficult to cannulate and the bleeding vessel could not be selectively embolized. Upon discussion with the teams involved, there were limited operative options. As a result, a plan was made to place a covered stent in the SMA across the ostia of the inflow of the MCA. This effectively stopped the bleeding, and the remainder of the SMA remained patent (Figure 5). For the rest of her hospital stay, she had no further bleeding episodes. Her hospital course was complicated by a prolonged post-operative ileus for 14 days requiring total parenteral nutrition supplementation. She also developed a deep vein thrombosis in her right brachial vein on a post-operative day seven, requiring anticoagulation. Her presumed cholecystitis was mild, likely secondary to her large bleed, and was managed with parenteral antibiotics for 14 days. She made a full recovery and was discharged home 21 days after her index operation. At her 6-month follow-up visit, she continued to do well without any symptoms of biliary colic.
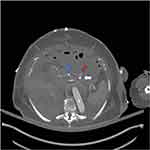 |
Figure 4 CT angiogram arterial phase axial view demonstrating ongoing bleeding from middle colic artery branch (red arrow). Prior coils (blue arrow) and surgical clips at outflow (white arrow) shown. |
Discussion
MCA aneurysm is an extremely rare occurrence, with unknown incidence. The etiology of MCA aneurysm is poorly understood. Similar to other aneurysms, their development has been associated with connective tissue disorders such as Marfan syndrome or Ehlers-Danlos, or medical conditions such as vasculitis or pregnancy. Conversely, visceral artery pseudoaneurysms result from a tear in the vessel wall due to trauma or instrumentation.4 Owing to its rarity, a typical disease presentation of MCA aneurysm does not appear to exist. On review of the literature, many patients present with hemodynamic instability and hemoperitoneum, similar to a ruptured abdominal aortic aneurysm (AAA).2,5,6 However, prolonged vague gastrointestinal symptoms7,8 or even asymptomatic detection leading to outpatient elective referral have also been described.9 Symptomatology could easily be attributed to other more common abdominal pathology such as pancreatitis, peptic ulcer disease, or biliary colic.2,9 In the present case, our patient initially had clinical, laboratory, and radiologic findings most suggestive of acute calculous cholecystitis. Her more pressing and life-threatening issue, the ruptured MCA aneurysm, was identified incidentally. To our knowledge, this is the first case in the literature where a patient presented with both acute calculous cholecystitis, and ruptured MCA aneurysm simultaneously.
The co-existence of two seemingly unrelated pathologies defies medical axioms where a single unifying diagnosis to explain symptomatology is preferred over multiple co-occurring phenomena.10 Therefore, one might dispute the etiology of her cholecystitis, and whether this was truly caused by her gallstones. Despite her suggestive symptomatology and ultrasound findings, her gallbladder appeared grossly normal when examined intra-operatively. Furthermore, there was a large hematoma immediately adjacent to this area, and some surrounding inflammatory adhesions. As blood products are highly irritating, inflammation is likely from the adjacent hemorrhage rather than originating from gallstone disease. Conversely, gallstone-related pathology is extremely common, and by chance alone it is possible the MCA aneurysm and cholecystitis could have occurred simultaneously without a causal link.11
The second unique aspect of this case is the manner of vascular control. Previous studies showed that stable bleeding from ruptured MCA aneurysms could be controlled through endovascular intervention or open surgery.2,12 A combined approach in one patient with chronic aortic occlusion has also been described.13 However, the present case is the first where an intra-aortic balloon catheter has been placed for a ruptured MCA aneurysm, in case of a need for emergency vascular control. Management of severe exsanguinating hemorrhage from abdominal vasculature is not a new subject and is well represented in the trauma literature. Methods for emergency hemostatic control range from direct manual supracelliac aorta compression to emergent thoracotomy and aortic clamp.14 Recently, an endovascular approach called resuscitative endovascular balloon occlusion of the aorta (REBOA) has increased in popularity and presents a compelling option obviating the need for resuscitative thoracotomy in peri-arrest situations due to bleeding.15 In the present case, the large hematoma overlying the aorta precluded safe access prior to entering the hematoma cavity and potentially exposing the patient to the risk of brisk life-threatening hemorrhage. We elected to place an aortic balloon catheter in a site proximal to the SMA so that it could be inflated for immediate hemostatic control if necessary. Fortunately, bleeding from the MCA was relatively minor intraoperatively and we were able to control it locally without the need to inflate the aortic balloon. Rarely, REBOA, which is typically administered in the emergency department in a significant trauma setting or ruptured AAA, has been associated with significant complications such as dissection, ischemia, and death.16 Such risks were likely much lower in our patient, where the balloon was positioned in the operating room under fluoroscopic guidance.
Another option, which was initially attempted in the present case, is endovascular occlusion via coil embolization. However, as reviewed by Huo et al, many previous case reports have had failed endovascular attempts and led to more traditional laparotomy.2 Challenges with the endovascular approach include difficult access due to tortuous, small vasculature, and often unstable patients who cannot be managed safely in an interventional radiology suite. Risks related to an endovascular approach also include bowel ischemia, although this has been rarely reported after MCA aneurysm embolization.3
A final consideration in the present case is the question as to the optimal management of this patient’s gallbladder. Typically, acute calculous cholecystitis is managed with urgent cholecystectomy.17 Given the patient’s ruptured aneurysm, managing the more dangerous issue took precedence. As the gallbladder had a grossly normal appearance at laparotomy, the gallbladder was left in situ so as not to risk possible additional complications from a potentially unnecessary procedure. While complications following open cholecystectomy are rare, major vasculobiliary injuries can occur.18 The possibility of these issues may have complicated the post-operative monitoring of this patient, who eventually presented with a repeat bleed. However, given the presence of gallstones on preoperative ultrasound, cholecystectomy at the index laparotomy could have been a reasonable option. The risk of recurrent gallstone-related disease, even in elderly patients with significant comorbidities, is important,19 and cholecystectomy is typically recommended for symptomatic patients who can tolerate the procedure.20 Furthermore, an interval cholecystectomy, if necessary, would likely be very challenging in this patient due to the resultant adhesions from her adjacent intra-abdominal hemorrhage and prior laparotomy.
Conclusion
Middle colic artery aneurysm can be a challenging condition to diagnose and treat. Optimal management requires a team approach between vascular surgery, general surgery, and interventional radiology. Previously, management options included endovascular embolization, open surgery, or a combination of approaches. Intra-aortic balloon placement for emergency vascular control, as described in trauma literature, is a novel addition to MCA aneurysm rupture management when intra-abdominal vascular access is challenging.
Abbreviations
AAA, abdominal aortic aneurysm; CT, computed tomography; MCA, middle colic aneurysm; MS, multiple sclerosis; REBOA, resuscitative endovascular balloon occlusion of the aorta; SMA, superior mesenteric artery.
Ethics Approval and Informed Consent for Publication
Informed consent for publication of the patient’s medical details and photographs was obtained from the patient prior to publication. Institutional approval was obtained from the University of Manitoba’s Health Research Ethics Board.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There was no specific funding for this research.
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Juntermanns B, Bernheim J, Karaindros K, Walensi M, Hoffmann JN. Visceral artery aneurysms. Gefasschirurgie. 2018;23(Suppl 1):19–22. doi:10.1007/s00772-018-0384-x
2. Huo CW. Middle colic artery aneurysm: a case report and review of the literature. Ann Vasc Surg. 2012;26(4):571.e1–6. doi:10.1016/j.avsg.2011.07.023
3. Kim SH, Lee MS, Han HY, Lee HM. Endovascular management of ruptured middle colic artery aneurysm and review of the literature. Ann Vasc Surg. 2019;59:310.e13–310.e16. doi:10.1016/j.avsg.2018.12.099
4. Ibrahim F, Dunn J, Rundback J, Pellerito J, Galmer A. Visceral artery aneurysms: diagnosis, surveillance, and treatment. Curr Treat Options Cardio Med. 2018;20(12):97. doi:10.1007/s11936-018-0696-x
5. Srinivasan R, Parvin SD, Lambert D. Spontaneously ruptured middle colic artery aneurysm in a patient with Marfan’s syndrome. Eur J Vasc Surg. 1990;4(3):317–318. doi:10.1016/S0950-821X(05)80215-4
6. den Butter G, van Bockel JH, Aarts JC. Arterial fibrodysplasia: rapid progression complicated by rupture of a visceral aneurysm into the gastrointestinal tract. J Vasc Surg. 1988;7(3):449–453. doi:10.1016/0741-5214(88)90445-4
7. Verma BS, Bose AK, Bhatia HC, Katoch R. Superior mesenteric artery branch aneurysm diagnosed by ultrasound. Br J Radiol. 1991;64(758):169–171. doi:10.1259/0007-1285-64-758-169
8. Kataoka M, Naruse M, Watarai N, et al. Retroperitoneal bleeding due to a ruptured aneurysm of the middle colic artery. Jpn J Surg. 1984;14(2):150–154. doi:10.1007/BF02469808
9. Nishimura K, Hamasaki T, Ota R, et al. Elective treatment of middle colic artery aneurysm. Ann Vasc Dis. 2014;7(3):328–330. doi:10.3400/avd.cr.14-00058
10. Wardrop D. Ockham’s Razor: sharpen or re-sheathe? J R Soc Med. 2008;101(2):50–51. doi:10.1258/jrsm.2007.070416
11. Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172–187. doi:10.5009/gnl.2012.6.2.172
12. Hirokawa T, Sawai H, Yamada K, et al. Middle-colic artery aneurysm associated with segmental arterial mediolysis, successfully managed by transcatheter arterial embolization: report of a case. Surg Today. 2009;39(2):144–147. doi:10.1007/s00595-008-3811-x
13. Hanada K, Takayama T, Sasaki T, Taniguchi R, Hoshina K. A hybrid procedure for middle colic artery aneurysm complicated by chronic juxtarenal segmental aortic occlusion. J Vasc Surg Cases Innov Tech. 2019;5(3):327–331. doi:10.1016/j.jvscit.2019.03.011
14. Kobayashi LM, Costantini TW, Hamel MG, Dierksheide JE, Coimbra R. Abdominal vascular trauma. Trauma Surg Acute Care Open. 2016;1(1):e000015. doi:10.1136/tsaco-2016-000015
15. van Dongen TTCF, Morrison JJ, Hedeman JPPA, et al. A systematic review and meta-analysis of the use of resuscitative endovascular balloon occlusion of the aorta in the management of major exsanguination. Eur J Trauma Emerg Surg. 2018;44(4):535–550. doi:10.1007/s00068-018-0959-y
16. Ribeiro Junior MAF, Feng CYD, Nguyen ATM, et al. The complications associated with Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). World J Emerg Surg. 2018;13(1):20. doi:10.1186/s13017-018-0181-6
17. Yokoe M, Hata J, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):41–54. doi:10.1002/jhbp.515
18. Visser BC, Parks RW, Garden OJ. Open cholecystectomy in the laparoendoscopic era. Am J Surg. 2008;195(1):108–114. doi:10.1016/j.amjsurg.2007.04.008
19. Edwards K, Johnson G, Bednarz J, Hardy K, McKay A, Vergis A. Long-term outcomes of elderly patients managed without early cholecystectomy after endoscopic retrograde cholangiopancreatography and sphincterotomy for choledocholithiasis. Cureus. 2021;13(10):e19074. doi:10.7759/cureus.19074
20. Rao A, Polanco A, Qiu S, et al. Safety of outpatient laparoscopic cholecystectomy in the elderly: analysis of 15,248 patients using the NSQIP database. J Am Coll Surg. 2013;217(6):1038–1043. doi:10.1016/j.jamcollsurg.2013.08.001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


