Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Robotic single-site surgery for mature cyst teratoma cystectomy: an initial case series study in a single medical center in China
Authors Liu Z, Tian S, Yan Z, Yu X, Li X, Tao Y
Received 11 June 2018
Accepted for publication 29 December 2018
Published 24 January 2019 Volume 2019:15 Pages 179—185
DOI https://doi.org/10.2147/TCRM.S176852
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Zhongyu Liu,1 Shuang Tian,1 Zhifeng Yan,1 Xiurong Yu,2 Xiuli Li,1,3 Ye Tao4
1Department of Obstetrics and Gynecology, PLA General Hospital, Beijing 100853, PR China; 2Department of Anesthesia Surgery Center, Hainan Branch of PLA General Hospital, Sanya 572013, PR China; 3Department of Obstetrics and Gynecology, Hainan Branch of PLA General Hospital, Sanya 572013, PR China; 4Department of Ophthalmology, PLA General Hospital, Beijing 100853, PR China
Objective: To report the first case series of robotic single-site (RSS) surgery via the da Vinci Si Surgical System for mature cyst teratoma cystectomy in China.
Materials and methods: The study was devised as a retrospective study in a single medical center. Five patients with mature cyst teratomas requested a minimally invasive surgical treatment. These patients were treated with RSS surgery for mature cyst teratoma between January 2014 and January 2015. RSS mature cyst teratoma cystectomies were performed with the da Vinci single-site platform in the Hainan branch of PLA General Hospital. Data regarding patient characteristics, surgical approach, and perioperative clinical outcomes were collected and analyzed in a retrospective study.
Results: All RSS procedures were completed successfully in the five patients. No instrument failure was noted during the procedures. The median operating time was 65 minutes (range 45–100 minutes). The median docking time was 20 minutes (range 18–28 minutes). No instrument failure was noted during any surgical procedures. The median blood loss was 30 mL (range 10–70 mL). No patient had massive intraoperative bleeding nor required a transfusion. No extra trocar was placed during the surgery. None of the patients had bladder or rectal injury. The median length of stay in hospital was 2.8 days. All patients were followed up until 6 months postoperatively, and no surgical complication occurred.
Conclusion: RSS mature cyst teratoma cystectomy using the wristed semirigid instrumentation is feasible. Randomized controlled trials with a larger number of patients and longer postoperative follow-up should be conducted to further evaluate the effect of this therapeutic strategy.
Keywords: da Vinci robotic single-site platform, robotic single-site surgery, mature cyst teratoma, laparoscopic single-site surgery
Introduction
Conventional laparoscopy is the recommended surgical approach for mature cyst teratoma cystectomy. The surgery via the laparoscopic approach could improve quality of life with satisfactory surgical outcomes under various gynecologic conditions.1–3 Despite the excellent outcomes of laparoscopic gynecologic surgery, possible risks might accompany this therapeutic approach, especially with multiport laparoscopy. The laparoscopic gynecologic surgery procedures require 3–5 trocar incisions, including muscle-splitting incisions. In the last decade, laparoscopic single-site surgery (LESS) has emerged as a potentially minimally invasive therapeutic strategy. The feasibility of LESS for adnexal surgery and myomectomy has been reported by several studies.4–6 This innovative laparoscopic surgical approach presents some unique challenges, such as avoiding instrument crowding, manipulating a flexible camera, and coordinating all the surgical instruments through a small umbilical incision.7 Thus, LESS requires more advanced laparoscopic surgery skills than the conventional laparoscopic surgery.8,9 In addition, the learning curves and the expense associated with LESS may be factors deterring the universal adoption of LESS.10,11
Robotic surgery has vastly improved surgical precision, visualization, surgeon dexterity, and ergonomics. Robotic surgical platforms had shorter learning curve compared to traditional laparoscopy for select surgeons.12 When considering technical challenges, introducing the robotic system into single-site surgery has several advantages over LESS or conventional robotic surgery, and it may also overcome some of the technical limitations of LESS. The robotic single-site (RSS) surgical platforms have been developed recently.13 The feasibility and safety of RSS surgery have been demonstrated in gynecologic surgery.14–19 However, this novel surgical technology still requires critical evaluation in several aspects, including the assessment of comparative advantages, quality, clinical efficacy, and patient satisfaction.
Mature cyst teratoma is a common disease in females. To date, no study has assessed the clinical outcomes of RSS in mature cyst teratoma cystectomy. In this context, we explored the perioperative outcomes of RSS mature cyst teratoma cystectomy. The first purpose of this study is to determine the feasibility and safety of RSS for the surgical treatment of mature cyst teratomas. The second purpose is to describe techniques for the successful platform setup and the performance of mature cyst teratoma cystectomy procedures through a novel RSS platform. To our knowledge, this is the first gynecologic RSS surgery research study in China.
Materials and methods
The protocol of this retrospective study was approved by the Institutional Review Board of the PLA General Hospital Institutional Review Board. The study has been reported in line with the PROCESS criteria.20 All patients provided written informed consent for the procedure and for their data to be used for future research. Five cases were enrolled in the present study. All the patients undergoing adnexal surgery for mature cyst teratoma were offered RSS surgery during the study period from January 2014 to January 2015. While getting written informed consent, patients were counseled regarding the following: the RSS platform would be a novel therapeutic strategy for mature cyst teratomas, and all the RSS surgeons were well trained and experienced with traditional robotic gynecologic surgery and conventional LESS. All patients gave written consent for surgery.
The inclusion criteria were as follows: 1) patients with mature cyst teratoma; 2) patients 18 years or more of age; 3) the tumor marker CA125 was l<40 U/mL; 4) the lesion was presumed to be benign based on the clinical evaluation and preoperative imaging; 5) there was no contraindication for robotic surgery; 6) patients had no pelvic surgery history. All included cases underwent quick frozen pathology during the surgery. The exclusion criteria included the following: 1) the pathology examination showed no mature cyst teratoma; 2) the patient had a contraindication for robotic surgery; 3) the patient was <18 years of age; 4) the patient had pelvic surgery history; 5) the CA125 level was >40 U/mL.
Data for age, body mass index (BMI, calculated as kg/m2), pelvic surgery history, and CA125 level were obtained before surgery. For each patient, the operative time, length of hospital stay, blood loss, and intraoperative or postoperative complications were analyzed. The operative time was the interval between the incision start and closure. Specifically, the operative time included the umbilical incision time, single-port placement time, robotic docking time, and surgeon console time. The intraoperative complications included blood loss >500 mL, blood transfusion, extra trocars placed, conversion to open surgical procedure, and bladder or rectal injury. The postoperative complications included postoperative bleeding, wound infection, and trocar-site hernia.
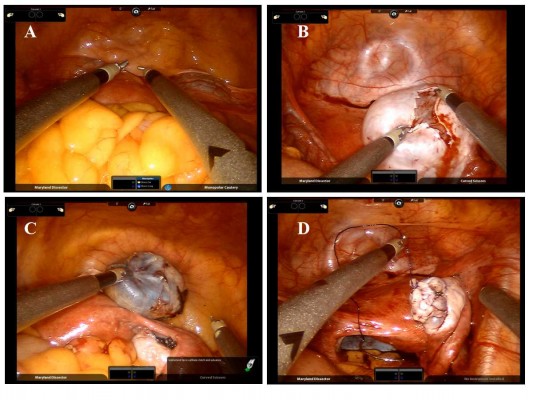
All patients underwent RSS mature cyst teratoma cystectomy. The RSS mature cyst teratoma cystectomy techniques were readily incorporated into the conventional LESS and performed by a team of surgeons. The participating physicians had extensive experience in robotic gynecologic surgery. These physicians had used the da Vinci robotic surgery system in gynecologic surgery for early ovarian cancer, cervical cancer, endometrial carcinoma, uterine prolapse, and manual vaginal construction.21–23 In this study, all the surgical procedures were performed via the da Vinci Surgical System (Intuitive Surgical System, Sunnyvale, CA, USA) with a novel set of single-site instruments and accessories. The accessories included a multichannel access port with room for four cannulae and an insufflation valve (Figure 1A). Two curved cannulae, one camera cannula, and one assistant cannula were used as robotically controlled instruments (Figure 1B). Except that the entire length of the instruments is semirigid of the da Vinci single-site instruments, which were similar to the da Vinci Si EndoWrist. The semirigid instruments allowed to be inserted through the curved cannulae and triangulation of the anatomy (Figure 1C). In contrast to standard robotic instrumentation, these instruments did not have the wrist at the tip of the single-site instrument. They were rigid enough to grasp and retract the tissue. The instruments available for this platform included needle-drivers, a suction irrigation device, a hook with cautery, and a Maryland dissector. A single 2.5 cm incision was made through the midpoint of the umbilicus. The da Vinci single-site port was positioned at the incision (Figure 2A). The abdomen was insufflated to 14 mmHg through the CO2 tubing that was attached to the insufflation adapter (Figure 2B). A 0°, 8.5 mm robotic endoscope was inserted through the trocar (Figure 2C). Docked to the camera port when the robot was positioned appropriately, a 5 mm accessory trocar was placed, and the curved cannulae were inserted through the marked lumens on the single-site port under direct visualization. The external view of the da Vinci system when connected to the trocar is shown in Figure 2C. After the instrumentation was positioned and the robot was fully docked, the da Vinci system software automatically detected and reassociated the surgical hands with the instrument tips (Figure 2D). The assistant surgeon using a standard 5 mm endograsper helped to retract the bowel or the other tissues, and use a bipolar grasper to coagulate the vessels through the assistant channel.
  | Figure 1 (A) Multichannel port; (B) the endoscope cannula, assistant cannula, and two curved cannulae; (C) the 5 mm semirigid instruments. |
The state of two semirigid robotic instruments in the pelvic cavity is shown in Figure 3A. An incision was made in the cyst wall using a hook monopolar cautery (Figure 3B). The assistant surgeon with a laparoscopic grasper grasped the cyst to increase the distance from the robotic arms and to fix the cyst. A robotic suction irrigation device and a grasper robotic were used to remove the capsule (Figure 3C). During cystectomy, the assistant surgeon used a laparoscopic bipolar grasper for hemostasis. Subsequently, the 4-0 absorbable suture was used to seam the surgical incision in the ovary to normal appearance (Figure 3D). The storage bag was placed in the pelvic cavity to collect the ovarian cyst (Figure 4A). The cyst wall was removed via the umbilical incision (Figure 4B). The 4-0 absorbable suture was used to seam the surgical incision in the abdomen (Figure 4C). The peritoneum, muscle scabbard film, subcutaneous fat, and skin were sewed to prevent the hemorrhage and incisional hernia (Figure 4C). The overall effect of the umbilical incision after suture is shown in Figure 4D.
All patients were followed up for 6 weeks at the outpatient clinic after hospital discharge. The patients were regularly followed up if their symptoms were absent. All symptomatic patients underwent radiologic imaging in case of any persisting symptoms. Patients were contacted two times by telephone during the 6 months post operation to score the presence of trocar-site herniation. The statistics were primarily descriptive. The median and range were used for continuous data. Categorical data were presented as the number of patients and a percentage.
Results
Six patients underwent mature cyst teratoma cystectomy using the da Vinci Si Surgical System from January 2014 to January 2015. All included patients had neither history of pelvic surgery, nor any contraindication for robotic surgery. One patient was excluded from the study because the frozen pathology examination suggested nonmature teratoma. The other five patients were included in the present study. The characteristics of the five RSS cases are presented in Table 1. All five cases were completed in a minimally invasive approach, and none of them was converted to laparotomy. The median patient age was 39 years (range 20–45 years), and the median BMI was 23.5 kg/m2 (range 19.5–33 kg/m2). The five patients accepted pelvic ultrasound examination and tumor marker detection preoperatively. The pelvic ultrasound examination suggested that all patients had mature cyst teratoma, and their tumor marker CA125 was <40 U/mL. The clinical evaluation and preoperative imaging examinations suggested that these included patients had benign conditions.
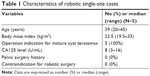  | Table 1 Characteristics of robotic single-site cases |
The surgical outcomes of the included patients are described in Table 2. The median operative time was 65 minutes (range 45–100 minutes). The median docking time was 20 minutes (range 18–28 minutes). No instrument failure was noted during any surgical procedures. The median blood loss was 30 mL (range 10–70 mL). No patient had massive intraoperative bleeding nor required a transfusion. No extra trocar was placed during the surgical procedure. None of the patients had bladder or rectal injury. The length of hospital stay ranged from 2 to 4 days, and the median length of hospital stay was 2.8 days. All the patients had exhaust within 24 hours post operation. All patients were followed up until 6 months postoperatively, and no surgical complication occurred. No patient had postoperative bleeding. No patient underwent wound infection or trocar-site hernia. In this study, no one patient underwent cyst rupture in the surgery. All the patients had successful wound healing based on a postoperative visual examination. The intraoperative and postoperative results are shown in Table 2.
  | Table 2 Intraoperative and postoperative results |
Discussion
In the past decade, several studies have demonstrated that laparoscopic surgery is a feasible surgical method for various gynecologic diseases. This therapeutic strategy could result in shorter hospital stay, improved quality of life, and comparable surgical outcomes to those of traditional laparotomy.24,25 However, several critical technical obstacles would keep this therapeutic procedure from full integration into usual practice of conventional laparoscopy. Robotic surgery could afford several advantages, such as three-dimensional visualization, tremor control, a stable camera platform, scaling of movement, and range of motion, which are superior to those of conventional laparoscopy. Moreover, the operative complications related to trocar insertion, such as vessel injury, the troca wound infection, and hematoma formation, might be avoided by reducing the number of ancillary troca penetrating the napes. Therefore, RSS surgery has several advantages compared to LESS or conventional robotic surgery. RSS surgery has been applied to colectomy, cholecystectomy, hernia, appendectomy, and bariatric surgical procedures. Among these procedures, RSS cholecystectomy is currently the most widely used application within general surgery.26 Escobar et al reported the first experience with RSS gynecologic surgery using the da Vinci Si platform on a porcine model.27 Nam et al reported a retrospective series study, using a home-made surgical glove port system put into practice in seven women who underwent robotic single-port total hysterectomy.28
Ovarian cystectomy surgery is usually performed successfully with conventional laparoscopy. However, this procedure damages more normal ovarian tissue and has the potential to decrease the ovarian reserve, which may be an important issue, especially in reproductive-age and infertile women. In this regard, RSS surgery may be advantageous, because it has the superiority of magnified three-dimensional view, more precise operation dissection, and improved hemostasis. Admittedly, the cost is one of the main shortcomings of the robotic device. The surgery complications related to trocar insertion, such as vessel injury, troca insert wound infection, and hematoma formation, might be avoided by reducing the number of ancillary ports penetrating the abdominal wall. Moreover, the umbilical incision is larger than the traditional robotic or laparoscopic port site. For this reason, RSS surgery may be of remarkable benefit in outlet for tissue extraction, and it avoids extending a muscle-splitting port incision to accommodate the tissue mass.
The present study demonstrates that RSS mature cyst teratoma cystectomy could act as a feasible therapeutic strategy for mature cyst teratomas. Due to the inadequate length of the instruments and the lack of tactile, EndoWrist, and/or force feedback, the surgical procedure can be technically challenging. Compared with conventional laparoscopic surgery, the RSS could afford some benefits, such as the improved three-dimensional view, more dexterity, and more stable camera.29 The LESS restricts the ability of maneuvering the instruments’ work due to a parallel position. RSS gains access to a greater range of motion of instrument because it allows the surgical instruments to cross. The crossing instruments are difficult to manipulate in conventional surgery since left is right and vice versa.30 Admittedly, a high amount of cystic ruptures occurred in RSS because of the lack of force feedback. In conventional laparoscopic and LESS, the surgeon could feel the tractive power on the cyst. In contrast, due to the lack of force feedback limits of robotic surgery system, the surgeon reduces the tractive power when needed. On the other hand, due to the flexible instruments without EndoWrist and without the adjusting ability, RSS surgery system might result in higher force needed to retract organs. Some technical improvements on the instruments and platform are still needed. Whether this platform would be superior in terms of performance and surgical outcomes to conventional single-site laparoscopy remains to be explored by further clinical trials. To this point, there are only a few published data for the RSS surgery in gynecology. In clinical practice, we have used the RSS techniques in gynecologic operations for ovarian cysts and leiomyomas. Admittedly, our experience in ovarian cysts is limited up to now, as only five ovarian cystectomy surgeries have been performed with this technique. It is noteworthy that the strengths of this study reside in the methodology, which could be adopted by a prospective study for clinical results.
Conclusion
The present study demonstrates the safety and feasibility of RSS for mature cyst teratoma cystectomy. The unique advantages of the RSS platform may improve cosmesis, postoperative pain, and recovery time. This novel technology may be the further development of minimally invasive gynecologic surgery. Randomized controlled trials with an increased number of patients and long-term postoperative follow-up should be conducted to further evaluate the effect of this therapeutic strategy.
Acknowledgment
The study was sponsored by a grant from the Hainan Province Emphasized Promotion Program (ZDXM2015090).
Author contributions
Zhongyu Liu, Shuang Tian, Zhifeng Yan and Xiurong Yu contributed equally for this article. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;(3):CD003677. | ||
Fanfani F, Fagotti A, Ercoli A, et al. A prospective randomized study of laparoscopy and minilaparotomy in the management of benign adnexal masses. Hum Reprod. 2004;19(10):2367–2371. | ||
Galaal K, Bryant A, Fisher AD, et al. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev. 2012;12(9):CD006655. | ||
Jung YW, Kim YT, Lee DW, et al. The feasibility of scarless single-port transumbilical total laparoscopic hysterectomy: initial clinical experience. Surg Endosc. 2010;24(7):1686–1692. | ||
Kim YW, Park BJ, Ro DY, Kim TE, Dy R. Single-port laparoscopic myomectomy using a new single-port transumbilical morcellation system: initial clinical study. J Minim Invasive Gynecol. 2010;17(5):587–592. | ||
Kim TJ, Lee YY, Kim MJ, et al. Single port access laparoscopic adnexal surgery. J Minim Invasive Gynecol. 2009;16(5):612–615. | ||
Uppal S, Frumovitz M, Escobar P, Ramirez PT. Laparoendoscopic single-site surgery in gynecology: review of literature and available technology. J Minim Invasive Gynecol. 2011;18(1):12–23. | ||
Fader AN, Cohen S, Escobar PF, Gunderson C. Laparoendoscopic single-site surgery in gynecology. Curr Opin Obstet Gynecol. 2010;22(4):331–338. | ||
Murji A, Patel VI, Leyland N, Choi M. Single-incision laparoscopy in gynecologic surgery: a systematic review and meta-analysis. Obstet Gynecol. 2013;121(4):819–828. | ||
Fanfani F, Rossitto C, Gagliardi ML, et al. Total laparoendoscopic single-site surgery (less) hysterectomy in low-risk early endometrial cancer: a pilot study. Surg Endosc. 2012;26(1):41–46. | ||
Fagotti A, Boruta DM, Scambia G, Fanfani F, Paglia A, Escobar PF. First 100 early endometrial cancer cases treated with laparoendoscopic single-site surgery: a multicentric retrospective study. Am J Obstet Gynecol. 2012;206(4):353.e1–353.e6. | ||
Spinoglio G, Lenti LM, Maglione V, et al. Single-site robotic cholecystectomy (SSRC) versus single-incision laparoscopic cholecystectomy (SILC): comparison of learning curves. First European experience. Surg Endosc. 2012;26(6):1648–1655. | ||
Scheib SA, Fader AN. Gynecologic robotic laparoendoscopic single-site surgery: prospective analysis of feasibility, safety, and technique. Am J Obstet Gynecol. 2015;212(2):179.e1–179.e8. | ||
Nam EJ, Kim SW, Lee M, et al. Robotic single-port transumbilical total hysterectomy: a pilot study. J Gynecol Oncol. 2011;22(2):120–126. | ||
Cela V, Freschi L, Simi G, Ruggiero M, Tana R, Pluchino N. Robotic single-site hysterectomy: feasibility, learning curve and surgical outcome. Surg Endosc. 2013;27(7):2638–2643. | ||
Sendag F, Akdemir A, Zeybek B, Ozdemir A, Gunusen I, Oztekin MK. Single-site robotic total hysterectomy: standardization of technique and surgical outcomes. J Minim Invasive Gynecol. 2014;21(4):689–694. | ||
Iavazzo C, Gkegkes ID. Single-site port robotic-assisted hysterectomy: a systematic review. Arch Gynecol Obstet. 2014;289(4):725–731. | ||
Vizza E, Corrado G, Mancini E, et al. Robotic single-site hysterectomy in low risk endometrial cancer: a pilot study. Ann Surg Oncol. 2013;20(8):2759–2764. | ||
Mereu L, Carri G, Khalifa H. Robotic single port total laparoscopic hysterectomy for endometrial cancer patients. Gynecol Oncol. 2012;127(3):644. | ||
Agha RA, Fowler AJ, Rajmohan S, et al. Preferred reporting of case series in surgery; the process guidelines. Int J Sur. 2016;36:319–323. | ||
Liu Z, Li X, Li W, Yang Y, Tao Y, Yao Y. Robotic nerve-sparing radical hysterectomy for locally advanced cervical cancer after neoadjuvant chemotherapy. Int J Gynaecol Obstet. 2015;131(2):152–155. | ||
Li XL, Liu ZY, Zhou N, Zhu T, Yang YZ, Yao YQ. Long-term results of robotic sacral hysteropexy for pelvic organ prolapse in China single medical center. Int J Surg. 2016;27:128–132. | ||
Liu Z, Li X, Tian S, Zhu T, Yao Y, Tao Y. Superiority of robotic surgery for cervical cancer in comparison with traditional approaches: a systematic review and meta-analysis. Int J Surg. 2017;40:145–154. | ||
Johnson N, Barlow D, Lethaby A. Surgical approach to hysterectomy for benign gynecological disease. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD003677. | ||
Eltabbakh GH, Shamonki MI, Moody JM, Garafano LL. Hysterectomy for obese women with endometrial cancer: laparoscopy or laparotomy? Gynecol Oncol. 2000;78(3 Pt 1):329–335. | ||
Konstantinidis KM, Hirides P, Hirides S, Chrysocheris P, Georgiou M. Cholecystectomy using a novel single-site robotic platform: early experience from 45 consecutive cases. Surg Endosc. 2012;26(9):2687–2694. | ||
Escobar PF, Fader AN, Paraiso MF, Kaouk JH, Falcone T. Robotic-assisted laparoendoscopic single-site surgery in gynecology: initial report and technique. J Minim Invasive Gynecol. 2009;16(5):589–591. | ||
Nam EJ, Kim SW, Lee M, et al. Robotic single-port transumbilical total hysterectomy: a pilot study. J Gynecol Oncol. 2011;22(2):120–126. | ||
Heemskerk J, Zandbergen HR, Keet SW, et al. Relax, it’s just laparoscopy! A prospective randomized trial on heart rate variability of the surgeon in robot-assisted versus conventional laparoscopic cholecystectomy. Dig Surg. 2014;31(3):225–232. | ||
van der Linden YT, Brenkman HJ, van der Horst S, van Grevenstein WM, van Hillegersberg R, Ruurda JP. Robotic single-port laparoscopic cholecystectomy is safe but faces technical challenges. J Laparoendosc Adv Surg Tech A. 2016;26(11):857–861. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



