Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Risk of cancer after lung transplantation for COPD
Authors Ekström M , Riise GC, Tanash HA
Received 23 July 2017
Accepted for publication 29 August 2017
Published 3 October 2017 Volume 2017:12 Pages 2841—2847
DOI https://doi.org/10.2147/COPD.S147065
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Magnus Ekström,1 Gerdt C Riise,2 Hanan A Tanash3
1Department of Clinical Sciences, Division of Respiratory Medicine & Allergology, Lund University, Lund, Sweden; 2Department of Respiratory Medicine, Sahlgrenska University Hospital, Gothenburg, Sweden; 3Department of Respiratory Medicine, Skåne University Hospital, Lund University, Malmö, Sweden
Background: The risk of cancer is increased and affects survival after lung transplantation (LTx), but has not been well characterized in COPD. We aimed to evaluate the incidence and prognosis of cancer following LTx for COPD.
Methods: A prospective, population-based study of patients undergoing LTx for end-stage COPD at the two transplantation centers in Sweden between 1990-2013, with follow-up for incident cancer and death, using national registers. The excess risk of cancer was calculated as standardized incidence ratios compared with the general population matched for age, sex, and calendar year. Risk factors for cancer were analyzed using Fine-Gray regression, and survival after cancer diagnosis with Kaplan–Meier.
Results: In total, 331 patients (mean age 55.4 years; 64% women; 97% former smokers) were included. At a median follow-up of 2.8 years, 35% of patients had developed cancer and the risk was increased more than 10-fold ([95% CI] 8.1-11.8). The highest excess risks were for non-Hodgkin lymphoma (20.8-66.7), skin cancer (20.3-35.2), lung (11.7-31.2), liver (3.6-51.6), and colorectal cancer (6.1-19.5). Median survival was longer for skin cancer (8 years; 95% CI, 3-15) compared with non-skin cancer (4 years; 95% CI, 2.8-4.8; p<0.001).
Conclusion: The cancer risk is markedly increased after LTx for COPD. It could not be predicted by the factors evaluated, but contributed significantly to a negative prognosis.
Keywords: cancer, COPD, lung transplantation, severe alpha-1-antitrypsin deficiency, survival
Introduction
Lung transplantation (LTx) improves the survival time in selected patients with end-stage lung disease.1 With improved immunosuppression and surgical methods, survival after LTx has increased over the past 10 years. Major causes of mortality after LTx include chronic rejection and incident malignancy.1 In Sweden, the median survival time after LTx for end-stage COPD is 9 years.2 Longer survival, through longer exposure to immunosuppressive treatment, may increase the risk of developing morbidities after LTx, including an increased risk of cancer.
After solid organ transplantation, the cancer risk is elevated 2–4-fold compared with population controls.3 Factors associated with the increased cancer incidence include higher age of donor and recipient, type of LTx (single or bilateral), and type of immunosuppressive therapy.3–5 After transplantation, risks are especially high for cancers associated with viral infections, including Mb, Hodgkin and non-Hodgkin lymphoma (NHL) (caused by Epstein Barr virus [EBV]), anogenital cancer (human papillomavirus), and liver cancer (hepatitis C and B virus),6 but also for other malignancies such as lung, kidney, skin, and thyroid cancer.3 Compared with other cancers, cutaneous squamous cell carcinoma (SCC) has a particularly increased incidence but a better prognosis.7
Knowledge of the incidence and risk factors of cancer after LTx for COPD is limited. Earlier studies include a large range of solid organ transplantations or populations across different end-stage respiratory diseases.3,7,8 Patients with different respiratory conditions such as cystic fibrosis, COPD, and idiopathic pulmonary fibrosis often differ in preoperative risk factors for developing cancer. To date, no studies have specifically evaluated the risk of cancer after LTx for COPD. This knowledge is important as most patients with COPD undergoing LTx are former smokers, and COPD patients have an increased risk of cancers including lung and colon cancer.9 Furthermore, patients with COPD due to severe alpha-1-antitrypsin deficiency (AATD) have an increased risk of liver cancer.10
Sweden offers a unique opportunity to study the risk of incident cancer and mortality after LTx by cross-linkage between the two national transplantation centers in Lund and Gothenburg, together with the national registers on cancer and vital status which give a nearly complete coverage and follow-up.
The aim of this study was to estimate the risk of cancer by site, with a focus on non-skin cancer, among LTx patients with COPD in Sweden.
Methods
Study design and population
This was a prospective cohort study of all patients who underwent LTx for end-stage COPD at the two national LTx centers in Sweden, located at the university hospitals in Lund and Gothenburg. The study design has been detailed earlier.2 Patients were included between the start of the transplantation program in 1990 up until January 2013, and were prospectively followed-up for the primary endpoints, namely, a diagnosis of cancer or death, as recorded in national registers. Criteria for LTx in COPD patients and the diagnosis of COPD were in line with international recommendations.11
Assessments
LTx
Patients were assessed according to standardized protocols at the transplantation centers. Patients with a history of active cancer in the 5-year period prior to operation were not accepted for LTx in line with international guidelines.11 Medical records from the transplantation units were reviewed for all patients, including the pre-transplant investigation protocol, the operation protocol, discharge summaries after the operation, and the record of the final follow-up visit at the transplantation center. The following preoperative variables were obtained: smoking status and pack-years, medical history including previous cancer(s), spirometry, diffusing lung capacity for carbon monoxide, and body mass index (BMI), previous thoracic surgery, long-term oxygen therapy (LTOT) before LTx, type of LTx (single or bilateral), perioperative total allograft ischemic time, and cytomegalovirus (CMV) status of donor and recipient. Severe AATD was defined as the presence of the Pi-phenotype (PiZZ) which was confirmed by isoelectric focusing at the Department of Clinical Chemistry, Skåne University Hospital, Malmö, Sweden.
Follow-up
Cancer diagnoses were assessed using the Swedish Patient Register and Cancer Register.12–14 In Sweden, reporting diagnosed cancers to the Cancer Register is mandatory for both the diagnosing clinician and the pathologist, resulting in nearly complete data on diagnosed cancers nationally. Cancers were categorized according to the ICD-7 codes: oral cavity (140–148), digestive organs (150–159), respiratory organs (160–165), reproductive and genitourinary organs (170–181), hematological and lymphoproliferative (200–207), and skin (190–199).
Cancers were divided into: 1) skin cancers, which included SCC, basal cell carcinoma (BCC), and malignant melanoma; and 2) non-skin cancers, which included the digestive organs-, respiratory organs-, reproductive organs-, genitourinary organs-, lymphatic and hematological cancers.
Vital status was obtained from the Swedish Causes of Death Register. Individual participant data were cross-linked between registers using each patient’s specific Swedish social security number.
Ethical considerations
The study was conducted in accordance with the amended Helsinki Declaration, and was approved by the Regional Ethical Review Board in Lund (DNr: 2010/338 and 2015/186), which did not require individual patient consent as a high proportion of patients were deceased, and due to the registry-based design.
Statistical analyses
Patient characteristics were tabulated using descriptive statistics. The relative (excess) risk of cancer in transplanted patients compared to the general population was expressed as standardized incidence ratio (SIR), ie, the ratio of the observed to the expected numbers matched for age, sex, and calendar year. The expected number was calculated by multiplying the calendar period-, age- and sex-specific follow-up time in the cohort with the corresponding incidence in the general population. The follow-up time for cancer was from the date of transplantation and until the date of death, date of incident cancer (first cancer diagnosis), or study end (January 1, 2013), whichever came first. Estimates were presented with 95% CIs computed using the Poisson distribution. SIRs were calculated for all types of cancer, for the first cancer diagnosis, by anatomical site, and histopathological sub-classification. The estimated rate of developing cancer was calculated using survival tables.
Risk factors of incident cancer after LTx were analyzed using Fine-Gray regression, which accounts for the competing event of death.15 Factors evaluated were the recipient’s age, sex, AATD status (yes/no), BMI, pack-years of smoking, use of LTOT, days on waiting list, age of donor, CMV-mismatch between donor and recipient, type of LTx (single vs bilateral) and allograft ischemic time, all variables at the time of LTx (baseline).
Survival after first cancer diagnosis was analyzed using Kaplan–Meier. Differences in survival between patients with skin cancers and patients with non-skin cancers were calculated using the log-rank test. Follow-up time for survival was from the date of first cancer diagnosis to the date of death or study end. Statistical significance was defined as a two-sided p<0.05. Statistical analyses were performed with the Stata version 14.2 (StataCorp LP, College Station, TX, USA).
Results
Study population
A total of 331 patients received a lung transplant due to end-stage COPD between 1990 and January 2013 and were included in the analysis. The patients had a mean age of 55 (SD, 7) years, 64% were women, 38% had severe AATD, and 71% received a single lung transplant (Table 1). Only nine patients (3%) were never-smokers. The patients with a smoking history (97%) had smoked a mean of 25 (SD, 12) pack-years.
Immunosuppressive regimens were induction therapy with antithymocyte globulin and steroids, then prednisone, calcineurin inhibitors and azathioprine up until 2002, and thereafter prednisone, calcineurin inhibitors and mycophenolate mofetil. Twelve patients had a previous cancer diagnosis before LTx; eleven patients with previous cervix cancer, and one patient with lung cancer who was treated with pneumonectomy 10 years before LTx.
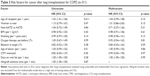
Incidence and excess risk of cancer
The median follow-up time from LTx to first cancer diagnosis, death or study end was 2.8 (interquartile range [IQR], 5.0) years, generating a total of 1,360 person-years at risk of cancer. During this time, 118 (35%) patients developed cancer; 54 (16%) developed skin cancer, and 64 (19%) developed non-skin cancer, SIR for all cancers was 10.0 (95% CI 8.1-11.8). The most common non-skin cancers were lung cancer (n=18), colorectal cancer (n=13), and NHL (n=13), Table 2.
Skin cancer
Skin cancer occurred in 54 patients, giving an excess risk by the SIR of 27.0 (95% CI, 20.3-35.2) compared with the general population matched for age, sex, and calendar year (Table 2). Of these, two patients developed malignant melanoma, SIR 3.7 (95% CI, 0.4-13.2), and 52 patients developed SCC and BCC, SIR 118.2 (88.3-155.0).
Non-skin cancers
The risk of non-skin cancers in LTx patients was increased more than 5-fold, SIR 5.6 (95% CI, 4.3-7.2). The highest excess risks were seen for NHL (SIR 39.0; 95% CI, 20.8-66.7), lung cancer (SIR 19.8; 95% CI, 11.7-31.2), liver cancer (SIR 17.7; 95% CI, 3.6-51.6), and colorectal cancer (SIR 11.4; 95% CI, 6.1-19.5). Cancers of the stomach, prostate, breast or urinary bladder were not significantly increased. The estimated risk of developing non-skin cancer was 2% (95% CI 1%−4%) at 1 year, 6% (95% CI, 3%−9%) at 3 years, 13% (95% CI, 9%−18%) at 5 years, and 31% (95% CI, 23%−39%) at 10 years.
The excess cancer risk was similar between patients who had undergone single LTx (SIR 5.1; 95% CI, 3.7-6.7) and those who had undergone bilateral LTx (SIR 6.4; 95% CI, 3.6-10.6).
Of the patients with severe AATD, 28 (22%) developed non-skin cancer, SIR 6.4 (95% CI, 4.2-9.2) which was comparable to the excess risk in the patients without AATD, SIR 4.7 (95% CI, 3.3-6.5), p=0.25. The SIR of colorectal, liver, and lung cancer was 12.0 (95% CI 4.0-28.0), 30.0 (95% CI 3.7-109.0), and 15.5 (95% CI 5.0-36.0) in the patients with AATD and 11.0 (95% CI 4.7-21.7), 9.5 (95% CI 0.24-53.0), and 24.0 (95% CI 13.0-40.0) in the patients without AATD, with no significant difference between the groups (p>0.10 for all comparisons).
Lung cancer occurred in 18 patients, SIR 19.8 (95% CI, 11.7-31.2). The median time from LTx to diagnosis of lung cancer was 2.6 (IQR, 3.7) years with 6/18 diagnoses within the first year post-transplantation. Most lung cancers (14/18; 78%) occurred in patients who had received a single lung transplant, and among these, 11/14 (79%) occurred in the native lung. There was no difference in the incidence of lung cancer between patients who had undergone single LTx (SIR 19.0; 95% CI, 10.3-31.6) and those who had undergone bilateral LTx (SIR 24.1; 95% CI, 6.6-61.7), p=0.68.
Risk factors for developing cancer
In univariate analyses, the only factor associated with increased risk of cancer after transplantation was a higher age of the recipient (Table 3). However, in multivariate analysis, no factor predicted the risk of cancer, including age, sex, AATD status, BMI, pack-years of smoking, LTOT, type of LTx (single/bilateral), donor age, CMV mismatch, or waiting time for the transplantation (Table 3). The cancer risk was not associated with year of LTx and thus did not change over the study period. Findings were similar for skin cancers and non-skin cancers.
Survival after cancer diagnosis
There were 43 (67%) deaths among the 64 patients who developed non-skin cancer, compared with 22 (41%) deaths in patients who developed skin cancer. Overall, the estimated median survival time after cancer diagnosis was 6 years (95% CI, 4-8), with longer median survival after the diagnosis of skin cancer (8 years; 95% CI, 3-15) compared with non-skin cancer (4 years; 95% CI, 2.8-4.8), p<0.001 (Figure 1). Cancer was the main cause of death in 70% of patients with non-skin cancer; NHL (n=12), lung cancer (n=9), colorectal (n=3), liver (n=3), and urogenital cancer (n=3), whereas cancer was the cause of death in only two patients (4%) with skin cancer.
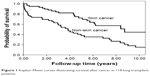  | Figure 1 Kaplan–Meier curves illustrating survival after cancer in 118 lung transplant patients. |
Discussion
Main findings
This study is the first to examine the risk of cancer after LTx, specifically in patients with COPD. The main finding is that the risk of cancers other than skin cancer was increased more than 5-fold compared with the general population. The highest excess risk was seen for NHL, lung, colorectal, and liver cancer.
Relation to previous findings
We found a high risk for NHL, possibly as a result of the intensity of immunosuppression or the large amount of lymphoid tissue conveyed within the lung graft.5 These results are in agreement with previously published studies. Engels et al have found that NHL is the most common malignancy in US transplant recipients.3 Previous studies have also shown that the most common NHL subtype among transplant recipients is diffuse large B-cell lymphoma, with most cases being EBV-positive.8,16 The risk of NHL is most pronounced among younger transplant recipients, who are more susceptible to a primary EBV infection following transplantation.6
The incidence of lung cancer was high in our study population (SIR 19.8). Patients underwent regular and intensive follow-up with chest X-ray, every 3 months during the first year and every 6 months thereafter. Heavy smoking exposure and immune suppression make the LTx recipients susceptible to lung cancer. The present findings are consistent with reports of increased lung cancer risk in smokers with COPD.17–19 Smokers with mild and moderate COPD have a 3-fold increased risk of developing lung cancer within 10 years, which increases to a 10-fold risk when severe COPD is developed, compared with smokers with normal lung function.18,19 We found that in patients who received single-lung transplants (71%), the majority of lung cancers developed in the remaining native lung, with 33% of cancers observed during the first year after transplantation. These results are in line with those of previous studies.4,20 There was no difference in the incidence of lung cancer between patients who had undergone single LTx and those who had undergone bilateral LTx, but this analysis could be affected by the low number of cases (n=4 in the double LTx group).
Risk of stomach, prostate, breast, and urinary bladder cancers compared with the general population was not significantly increased.
Consistent with previous studies of lung transplant recipients, our study showed an increased risk of non-melanoma skin cancer, which increased 118-fold. A population-based study from Sweden demonstrated a 198-fold increased risk of SCC in a mixed population of patients after heart and/or LTx compared with the general population.7 In another population-based study from Denmark, the SIR was 65 for skin cancer including SCC, BCC, and malignant melanoma among LTx patients.21 SCC is widely considered a benign disease with a good prognosis. In line with this, the patients with skin cancer in our study had significantly better survival than those with non-skin cancer. An increased risk of malignant melanoma compared with the general population was not observed in this study, which can be explained by the small number of patients. However, previously published studies have shown a moderate increase in risk (2.2-fold) of malignant melanoma.3,7,21,22 It was speculated that the development of melanoma is mainly linked to exposure to UV light and is not affected by immunosuppression therapy and/or viral carcinogenesis.7
The excess risk of non-skin cancer in patients with severe AATD after LTx was comparable to the excess risk in patients without AATD and the risk of cancer did not differ by AATD status in multivariate analysis. We did not find an increased risk of liver cancer in patients with severe AATD compared with patients without AATD. To our knowledge, no previous study has examined the risk of cancer after LTx, specifically in patients with COPD and severe AATD.
Mechanisms
The increased risk of cancer after LTx for COPD may be explained by several factors. The majority (97%) of the patients had smoked, with a mean exposure of more than 20 pack-years. Smoking is the single most important risk factor for several cancers, especially lung cancer. Immunosuppressive treatment is likely to contribute to the increased cancer risk.23 Lung transplant recipients tend to receive more intensive immune suppression than other solid organ transplant recipients. The role of immunosuppressive therapy in the development of cancer in organ transplant recipients is a matter of debate. In the present study, similar protocols for immunosuppression were used in patients who developed cancers and those who did not, which shows the importance of additional factors apart from immunosuppression in the development of cancer.
COPD is a complex disease associated with systemic consequences, including increased risk of both pulmonary and extra-pulmonary cancer.24,25 The improved treatment and survival time following LTx seen in recent decades are likely to increase the risk of developing cancer since these patients are exposed to immunosuppression for a longer time period. Another possible reason for the higher cancer risk in the present study compared with previous studies in solid organ transplantations is that the majority (64%) of the patients undergoing LTx for COPD in our study were women. It has been reported that comorbidities, such as cardiorespiratory disorders and cancer, including lung cancer, are more common among women with COPD compared with men.9,26 Women with severe COPD have been shown to have an almost 1.5-fold higher mortality risk of all types of cancer, and a 2.7-fold increased risk of lung cancer compared with men.9,26 The present study also extends our knowledge that the evaluated patient demographics and peri-operative characteristics cannot predict which patients will develop cancer.
Strengths and limitations
The strengths of the study are that it included a well-characterized, representative, national cohort of patients undergoing LTx for COPD at both transplantation units in Sweden. Patients were followed prospectively with outcomes assessed using population-based registers with practically complete coverage and follow-up.
The limitations include that we lacked data on potentially important risk factors for cancer, including hereditary history and genetic analyses. The impact of different immunosuppressive therapies could not be assessed as data on immunosuppression, including the dosage used, were not available. However, the risk of cancer, adjusted for confounders, did not change in the present analysis over the study period 1990–2013. Data on smoking exposure and morbidity for the Swedish control population were not available, and the excess cancer risk compared with non-smoking, healthy controls is probably even higher.
Conclusion
These results contribute new knowledge about the risk of cancer in COPD patients after LTx. Our study shows the importance of regular follow-up after LTx for the early diagnosis of malignancy; clinical follow-up and regular examination with chest X-ray, at a minimum every 3 to 4 months and regular skin screening. As 61% of lung cancer occurred in the native lung, bilateral LTx may be a better option for patients with a history of smoking, ie, COPD. This is also in line with what is now common procedure in the LTx field where over 66% of LTx are double LTx.
Acknowledgments
The authors wish to thank Isabella Björk for secretarial assistance and Jan-Åke Nilsson for statistical advice. We thank transplant nurse Marie Stiernspetz, transplant coordinator Katarina Karlsson, and Linda Persson for their help in collecting the data on the transplant patients.
Disclosure
ME was supported by unrestricted grants from the Swedish Society of Medicine and the Swedish Heart-Lung Foundation. HAT was supported by unrestricted grants from the Swedish Society of Medicine, Skåne University Hospital, and the Swedish Heart-Lung Foundation. The authors report no other conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
Yusen RD, Edwards LB, Dipchand AI, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-third Adult Lung and Heart-Lung Transplant Report-2016; Focus Theme: Primary Diagnostic Indications for Transplant. J Heart Lung Transplant. 2016;35(10):1170–1184. | ||
Tanash HA, Riise GC, Ekström MP, Hansson L, Piitulainen E. Survival benefit of lung transplantation for chronic obstructive pulmonary disease in Sweden. Ann Thorac Surg. 2014;98(6):1930–1935. | ||
Engels EA, Pfeiffer RM, Fraumeni JF Jr, et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011;306(17):1891–1901. | ||
Dickson RP, Davis RD, Rea JB, Palmer SM. High frequency of bronchogenic carcinoma after single-lung transplantation. J Heart Lung Transplant. 2006;25(11):1297–1301. | ||
Opelz G, Döhler B. Lymphomas after solid organ transplantation: a collaborative transplant study report. Am J Transplant. 2004;4(2):222–230. | ||
Cockfield SM. Identifying the patient at risk for post-transplant lymphoproliferative disorder. Transpl Infect Dis. 2001;3(2):70–78. | ||
Krynitz B, Edgren G, Lindelöf B, et al. Risk of skin cancer and other malignancies in kidney, liver, heart and lung transplant recipients 1970 to 2008 – a Swedish population-based study. Int J Cancer. 2013;132(6):1429–1438. | ||
Magruder JT, Crawford TC, Grimm JC, et al. Risk factors for de novo malignancy following lung transplantation. Am J Transplant. 2017;17(1):227–238. | ||
Ekstrom M, Franklin KA, Strom KE. Increased relative mortality in women with severe oxygen-dependent COPD. Chest. 2010;137(1):31–36. | ||
Tanash HA, Ekström M, Wagner P, Piitulainen E. Cause-specific mortality in individuals with severe alpha 1-antitrypsin deficiency in comparison with the general population in Sweden. Int J Chron Obstruct Pulmon Dis. 2016;26:1663–1669. | ||
Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates: 2014 – an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015;34(1):1–15. | ||
Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. | ||
National Board of Health and Welfare CfE. Cancerincidens i Sverige 2013 [Cancer Incidence Sweden 2013]. Available from: https://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19613/2014-12-10.pdf. Accessed December 10, 2014. Swedish. | ||
Barlow L, Westergren K, Holmberg L, Talbäck M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48(1):27–33. | ||
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. | ||
van Leeuwen MT, Grulich AE, Webster AC, et al. Immunosuppression and other risk factors for early and late non-Hodgkin lymphoma after kidney transplantation. Blood. 2009;114(3):630–637. | ||
El-Zein RA, Young RP, Hopkins RJ, Etzel CJ. Genetic predisposition to chronic obstructive pulmonary disease and/or lung cancer: important considerations when evaluating risk. Cancer Prev Res (Phila). 2012;5(4):522–527. | ||
Mannino DM, Aguayo SM, Petty TL, Redd SC. Low lung function and incident lung cancer in the United States: Data from the first National Health and Nutrition Examination Survey follow-up. Arch Intern Med. 2003;163(12):1475–1480. | ||
Young R, Hopkins R. Lung function predicts lung cancer. Eur Respir J. 2010;35(6):1421–1422. | ||
Minai OA, Shah S, Mazzone P, et al. Bronchogenic carcinoma after lung transplantation: characteristics and outcomes. J Thorac Oncol. 2008;3(12):1404–1409. | ||
Jensen AO, Svaerke C, Farkas D, Pedersen L, Kragballe K, Sørensen HT. Skin cancer risk among solid organ recipients: a nationwide cohort study in Denmark. Acta Derm Venereol. 2010;90(5):474–479. | ||
Dinh QQ, Chong AH. Melanoma in organ transplant recipients: the old enemy finds a new battleground. Australas J Dermatol. 2007;48(4):199–207. | ||
Kotloff RM, Ahya VN. Medical complications of lung transplantation. Eur Respir J. 2004;23(2):334–342. | ||
Kornum JB, Sværke C, Thomsen RW, Lange P, Sørensen HT. Chronic obstructive pulmonary disease and cancer risk: a Danish nationwide cohort study. Respir Med. 2012;106(6):845–852. | ||
Durham AL, Adcock IM. The relationship between COPD and lung cancer. Lung Cancer. 2015;90(2):121–127. | ||
Ekberg-Aronsson M, Nilsson PM, Nilsson JA, Löfdahl CG, Löfdahl K. Mortality risks among heavy-smokers with special reference to women: a long-term follow-up of an urban population. Eur J Epidemiol. 2007;22(5):301–309. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.