Back to Journals » Clinical Ophthalmology » Volume 15
Retrospective Comparison of Intraoperative Parameters, Efficacy and Safety in Cataract Surgery Between Halogen and Light-Emitting Diode (LED) Illuminated Surgical Microscope
Authors Tangjanyatam S
Received 8 July 2021
Accepted for publication 25 August 2021
Published 2 September 2021 Volume 2021:15 Pages 3721—3726
DOI https://doi.org/10.2147/OPTH.S328450
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sagol Tangjanyatam
Department of Ophthalmology, Hua Hin Hospital, Prachuap Khiri Khan, Thailand
Correspondence: Sagol Tangjanyatam Email [email protected]
Purpose: The objective was to compare the operative time, ultrasound time, efficacy and safety of phacoemulsification with IOL insertion between using halogen and light-emitting diode (LED) illuminated microscope.
Patients and Methods: Two hundred and twenty-seven surgical charts of cataract patients who underwent phacoemulsification with IOL insertion between June 2018 and October 2020 were reviewed. There were 113 cases operated on under halogen-illuminated microscope (Carl Zeiss OPMI LUMERA S7®) and 114 cases operated on under light-emitting diode (LED)-illuminated microscope (Leica PROVEO 8®). All cases were operated on by the same surgeon (S.T.). The difference in operative time and ultrasound time between two groups was compared by independent samples t-test. The proportion of cases with 3-months BCVA that was better than 20/30 and the proportion of cases with intraoperative complications from the operation between two groups were compared by Pearson’s Chi-squared test.
Results: The mean ultrasound time was 121.29± 53.60 seconds in halogen group and 123.98± 61.53 seconds in LED group. The mean difference was − 2.69± 8.44 seconds which was not statistically significant (95% CI, − 19.35 to 13.97; p=0.573). The mean operative time was 19.83± 4.77 minutes in the halogen group and 17.20± 3.02 minutes in the LED group. The mean difference was 2.63± 0.53 minutes (95% CI, 1.59 to 3.67; p < 0.001). The cases with BCVA better than 20/30 was 93.69% in halogen group and 95.49% in LED group. The proportion of cases with intraoperative complications was 3.53% in halogen group and 2.63% in LED group. The difference of both proportions was not statistically significant (p=0.553 and p=0.692, respectively).
Conclusion: This study shows statistically significant operative time reduction with LED microscope. This evidence could be used for making the decision to switch from halogen microscope to LED microscope. Upgrading to LED-illuminated microscope might be beneficial for productivity improvement if there were at least six to seven cases operated on per day. The ultrasound time, efficacy, and safety showed no significant difference.
Keywords: operative time, ultrasound time, light source, operative microscope
Introduction
Cataract surgery is the most common procedure performed by ophthalmic surgeons and phacoemulsification with IOL insertion is the preferred technique worldwide.1,2,10,11 The clinical outcome of cataract surgery depends on not only the surgeon’s techniques and skills but also the operative machine and instruments.3,4 The ophthalmic operating microscope is one of the most important instruments for modern cataract surgery.
One of the main differences between ophthalmic operating microscopes is the source of illumination. The two main sources of illumination are traditional halogen bulb and the newer light-emitted diode (LED) bulb. The LED bulbs produce brighter light using less power and emitting less heat compared to halogen light bulb. In addition, the LED bulbs are unlikely to burn out and degrade in light quality over time, which is one of the downsides of halogen bulbs.5
The manufacturers continue to upgrade their product lines and offer LED-illuminated ophthalmic operating microscopes on the market which are relatively more expensive than the halogen-illuminated models.
A previous study compared the effects of halogen- and LED-illuminated dental operating microscopes on asthenopia of the operators using accommodative function test and subjective symptoms questionnaire before and after the procedure. The result showed no significant change in degree of asthenopia before and after the procedure with either light source.6 Another previous study compared the effects of operating microscope with halogen and LED light source on rabbit eyes using in vivo confocal microscopy. This study demonstrated that both halogen and LED operating microscope has no sustained adverse effect on the cornea and the retina of a rabbit.7
There has been no previous study that compared halogen- and LED-illuminated ophthalmic operating microscope in clinical aspects of cataract surgery, and there is no clinical evidence demonstrating that the more expensive LED-illuminated microscope is superior to the traditional halogen-illuminated microscope.
The purpose of this study was to compare two intraoperative parameters which are operative time and ultrasound time of phacoemulsification with IOL insertion between using halogen- and LED-illuminated ophthalmic operating microscope. The efficacy and safety will also be compared between the two operating microscopes. The hypothesis is that the LED-illuminated microscope could provide better visualization and would result in less operative time and better efficacy and safety than the halogen-illuminated microscope.
Patients and Methods
Study Design
This study was a retrospective comparative study and took place at Hua Hin hospital, Prachuap Khiri Khan province, Thailand. The surgical charts of cataract cases that underwent phacoemulsification with IOL insertion under retrobulbar anesthesia operated on by a single surgeon (Sagol Tangjanyatam M.D.) between June 1st, 2018 to October 30th, 2020 were reviewed. Patients with conditions associated with longer operative time were excluded including patients with complicated cataract (posterior polar cataract, membranous cataract, pseudoexfoliation syndrome, traumatic cataract and phacodonesis), Toric IOL insertion, small pupil who were operated on with iris retractor insertion and patients who underwent combined surgery during the same operation such as pterygium excision. Patients with underlying disease that could affect best corrected visual acuity were also excluded including patients with advanced glaucoma, retinal and macular disease. The patients who underwent cataract surgery between June 1st, 2018 to August 21st, 2019 were operated on under OPMI LUMERA S7® halogen-illuminated operating microscope (Carl Zeiss, California, USA) and the patients who underwent cataract surgery between August 22nd, 2019 to October 30th, 2020 were operated on under PROVEO 8® LED-illuminated operating microscope (Leica, Wetzlar, Germany).
Surgical Technique
The operations were done by a single surgeon (Sagol Tangjanyatam, MD) with the same surgical technique using CENTURION® Phacoemulsification machine (Alcon, Geneva, Switzerland). The continuous mode was used with maximum power between 20 to 60% depending on the hardness of nucleus. The flow rate was set at 35 cm3/min. The vacuum was set at 100 mmHg for Sculpt mode, 300 mmHg for Chop mode, 280 mmHg for Quadrant removal mode, 330 mmHg for Epinuclear mode, 500 mmHg for Cortex mode, 8 mmHg for Polish mode, 650 mmHg for Viscoelastic removal mode. The small clear cornea incision was temporally created and the side port was created inferiorly for left eye, superiorly for right eye with 15 degree stab knife. Anterior lens capsule was stained by injection of 0.2 mL of 0.1% Trypan blue dye into anterior chamber via cannula. The dye remained in anterior chamber for 40 seconds, then Balanced Salt Solution (BSS®) was injected to clear anterior chamber. Viscoelastic material (1.8% Sodium Hyaluronate, IAL-F) was injected into anterior chamber. The continuous curvilinear capsulorhexis was made using a manually-bent 26-gauge disposable needle as a capsulorhexis cystotome. The main port of 2.4 millimeter clear cornea incision was created temporally by single bevel slit knife. The hydro-dissection and hydro-delineation were done using a 27-gauge hydrodissection cannula. The phacoemulsification was done using a 45-degree, 0.9 millimeter Kelman® Tapered ABS® MicrotipTM with a bevel-up tip, divide and conquer technique. The nuclear groove was made with Sculpt mode, then the nucleus was divided. The nucleus was chopped with Chop mode and was removed with Quadrant removal mode. After the nucleus was completely removed, the epinucleus was removed with Epinuclear mode. The tip was changed to 0.3 millimeter straight Irrigation/Aspiration (I/A) tip to remove the cortex with Cortex mode. The capsule was polished with Polish mode. The viscoelastic material was injected into anterior chamber and lens capsule. The intraocular lens was inserted into lens capsule followed by viscoelastic removal. The clear cornea incision was closed by stromal hydration technique.
Study Outcomes and Statistical Analysis
The preoperative, intraoperative, and postoperative data including surgical microscope, date of operation, gender, age, underlying disease, eye side, severity of nucleus cataract graded by Lens Opacities Classification System II (LOCS II),8 preoperative visual acuity, 3 months postoperative best corrected visual acuity (BCVA) assessed by Snellen chart with corrective lens, operation start and finish time, ultrasound time, total case time, intraocular lens (IOL) inserted, and intraoperative complications were collected by case record form.
This study selected 3-months postoperative BCVA data as efficacy of the operation to avoid temporary effect of postoperative corneal edema and to minimize effect of surgically induced astigmatism (SIA) as much as possible.
Dense nuclear cataract was a risk factor of transient worsening of visual acuity from immediate postoperative corneal edema.12–14 Surgically induced astigmatism was one factor that temporarily affected early postoperative visual acuity and gradually decreased with time. There were previous studies that demonstrated that SIA at 1 month postoperative was greater than at 3 months postoperative cataract surgery.15–19
The data were recorded and analyzed by IBM SPSS statistics 23®(SPSS Inc., Chicago, IL, USA). The statistical significance was set at P<0.05.
The distribution of operative time and ultrasound time data from each group was tested with Q-Q plot. The difference in operative time and ultrasound time between Halogen and LED group was compared by independent samples t-test. The efficacy and safety of the operation, which were the proportion of cases with 3-months BCVA that was better than 20/30 tested from the Snellen Chart and the proportion of cases with intraoperative complications respectively, between Halogen and LED group were compared by Pearson’s Chi-squared test.
Privacy and Ethical Consideration
This study was approved by the constituted Ethics Committee from Hua Hin Hospital, and it conforms to provisions of the Declaration of Helsinki. The patient consent requirement was waived by the constituted Ethics Committee from Hua Hin Hospital due to the retrospective nature of the review. The subjects were identified on case record forms by subject number. The data were stored in a locked and secure area in the study investigator’s office. The data were assessed and analyzed by a single investigator. Data that could possibly identify patients were not disclosed.
Results
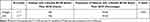
Two hundred and thirty-four surgical charts were enrolled in this study. Seven charts were excluded due to one case of posterior polar cataract, one case with iris retractor insertion, one case with retinitis pigmentosa, and four cases with advanced glaucoma. 227 charts were analyzed which were divided into Halogen group: 113 charts and LED group: 114 charts. Clinical characteristics of patients between each group were summarized in Table 1.
 |
Table 1 Clinical Characteristics of Cataract Patients Between Halogen-Illuminated Microscope Group and LED-Illuminated Microscope Group, N(%) |
This study included 54 patients who were operated on after March 11th, 2021 which was the day that the World Health Organization declared a pandemic of COVID-19.9 All fifty-four patients were operated on under LED microscope. Elective ophthalmic surgery in Hua Hin Hospital continued after the onset of the pandemic under COVID-19 guidelines. Every patient needed to have a “not detected” result from nasopharyngeal swab for COVID-19 by real-time PCR (polymerase chain reaction) within 72 hours before surgery. The surgical technique was the same.
Perusal of the Q-Q plot suggested that the operative time and ultrasound time data did not substantially depart from normality.
The mean ultrasound time was 121.29±53.60 seconds in halogen group and 123.98±61.53 seconds in LED group. The mean difference was −2.69±8.44 seconds which was not statistically significant (95% CI, −19.35 to 13.97; p=0.573). There were forty-one cases for which ultrasound time data were not applicable due to incomplete or incorrect records, so 186 cases were analyzed as shown in Table 2. The mean operative time was 19.83±4.77 minutes in the halogen group and 17.20±3.02 minutes in the LED group. The mean difference was 2.63±0.53 minutes which was statistically significant (95% CI, 1.59 to 3.67; p < 0.001) as shown in Table 3. The percentage of cases with 3-months BCVA better than 20/30 was 93.69% in halogen group and 95.49% in LED group with insignificant difference by Pearson’s Chi-squared test (p=0.553). There were five cases for which 3-months BCVA data were not applicable due to the patients being lost to follow-up, so only 222 cases were analyzed as shown in Table 4. The percentage of cases with intraoperative complications was 3.53% in halogen group and 2.63% in LED group. The difference was not significant as tested by Pearson’s Chi-squared test (p=0.692) as shown in Table 5.
 |
Table 2 Comparison of Ultrasound Time Between Halogen-Illuminated Microscope Group and LED-Illuminated Microscope Group |
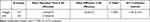 |
Table 3 Comparison of Operative Time Between Halogen-Illuminated Microscope Group and LED-Illuminated Microscope Group |
 |
Table 5 Comparison of Proportion of Cases with Intraoperative Complications Between Halogen-Illuminated Microscope Group and LED-Illuminated Microscope Group |
Discussion
Ophthalmic microscope is one of the most important instruments for cataract surgeons. The main technological advantages of LED-illuminated microscope over the halogen-illuminated microscope include greater luminous flux production capacity, lower energy consumption, lower heat production, longer lifetime, and less likely to burn out resulting in better visualization and more stable light quality.20,21 However, the price of LED-illuminated microscope is relatively higher.
In terms of safety, McDonald and Irvine first reported retinal toxicity associated with ophthalmic microscope in cataract surgery.22 There were publications demonstrating retinal toxicity secondary to conventional light source (tungsten or halogen) operating microscope. The incidence of toxicity related to duration of surgery, light intensity and exposure of certain wavelength of light, was related to retinal toxicity.23,24 In 2019, Taha et al evaluated possible toxic effect of different light sources on cultured human retinal pigment epithelium (RPE). The RPE cell cultures were exposed to halogen, xenon, and LED light sources at a distance of 1.5 centimeters for 30 and 60 minutes with equal lumen output levels. Only the halogen light showed significantly more DNA damage and lower viable cell counts at 30 and 60 minutes compared to the control group. However the distance between light source and RPE in cataract surgery is much longer than 1.5 centimeters demonstrated in this study.25
Without any clinical evidence to support clinical benefit, it is more difficult to make the decision to upgrade the light source especially for hospitals in low-income and middle-income countries which have a tight budget.
This study tried to compare halogen- and LED-illuminated microscopes in terms of clinical aspects. The results showed statistically significant operative time reduction of phacoemulsification with IOL insertion with LED-illuminated microscope. The mean operative time in LED group was 17.20±3.02 minutes with 2.63±0.53 minutes less than Halogen group, suggesting that upgrading to LED-illuminated microscope would be beneficial for productivity improvement if there were at least six to seven phacoemulsification with IOL insertion operations per day.
There were no statistically significant difference in ultrasound time between LED and halogen groups. The explanation might be that the ultrasound time depended on the hardness of nucleus without any benefit from better visualization. However, there was considerable data loss due to incomplete or incorrect records of ultrasound time data in this study resulting in an inadequate sample size.
The difference in percentage of patients with 3-months BCVA better than 20/30 and patients with intraoperative complications between halogen and LED groups was not statistically significant. This result suggested that the traditional halogen-illuminated microscope could provide comparable efficacy and safety to LED-illuminated microscope.
There were some limitations of this study. First, this study was a retrospective chart review, thus, there was some incomplete data records due to human errors, as shown in ultrasound time data. Second, this study had no intraoperative cumulative dissipated energy (CDE) data which could provide better information than ultrasound time data alone. Third, the halogen-illuminated and LED-illuminated microscopes in this study were produced by different manufacturers, so the different technology inside operating microscopes other than the light source could have been a confounding factor. Finally, in real practice, most phacoemulsification with IOL insertion operations are performed under topical anesthesia, however only the operations performed under retrobulbar anesthesia were included in this study, aiming at preventing confounding factor of intraoperative patient cooperation. This could have resulted in limitation of generalization.
Future studies should be conducted to compare luminance and heating under microscope, glare during surgery, intraoperative patient comfort, and postoperative phototoxicity between both light sources.
Conclusion
This study showed that phacoemulsification with IOL insertion performed under LED-illuminated microscope had the benefit of operative time reduction, so a productivity improvement could be expected when switching from the conventional halogen microscope to the more expensive LED microscope. From the results of this study, upgrading to LED-illuminated microscope might be beneficial for productivity improvement if there were at least six to seven cases operated on per day. The ultrasound time, efficacy and safety between both microscopes showed no significant difference. Both halogen- and LED-illuminated microscopes provided comparable efficacy and safety when operated by experienced surgeons. However, more extensive ocular safety like phototoxicity should be investigated in future studies for more accurate safety comparisons.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Blindness C. Vision 2020: the cataract challenge. Community Eye Health Int Cent Eye Health. 2000;13(34):17–19.
2. Bushra U, Iftikhar M, Latif A, et al. Epidemiology of primary ophthalmic procedures performed in the United States. Can J Ophthalmo. 2019;54(6):727–734. doi:10.1016/j.jcjo.2019.03.006
3. Park J, Yum HR, Kim MS, Harrison AR, Kim EC. Comparison of phaco-chop, divide-and-conquer, and stop-and-chop phaco techniques in microincision coaxial cataract surgery. J Cataract Refract Surg. 2013;39(10):1463–1469. doi:10.1016/j.jcrs.2013.04.033
4. Christakis PG, Braga-Mele RM. Intraoperative performance and postoperative outcome comparison of longitudinal, torsional, and transversal phacoemulsification machines. J Cataract Refract Surg. 2012;38(2):234–241. doi:10.1016/j.jcrs.2011.08.035
5. Lubeck DM. Red reflex stability improves illumination. Ocul Surg News. 2013;8–9. www.arboreyecare.com/wp-content/uploads/Red-reflex-stability.pdf
6. Kengo N, Mutoh N, Fuchida S, et al. Effects of different light sources used for dental operating microscope illumination on the visual function of operators. J Oral Biosci. 2020;62(4):363–371. doi:10.1016/j.job.2020.10.003
7. Bahri A. Comparison of the effects of operating microscopes with light emitting diode and halogen light source on the eye: a rabbit study. Cutan Ocul Toxico. 2021;6:1–7.
8. Chylack LT
9. Jin Y, Yang H, Ji W, et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12(4):372. doi:10.3390/v12040372
10. Thomson J, Lakhani N. Cataracts. Prim Care. 2015;42(3):409–423. doi:10.1016/j.pop.2015.05.012
11. Tabin G, Chen M, Espandar L. Cataract surgery for the developing world. Curr Opin Ophthalmo. 2008;19(1):55–59. doi:10.1097/ICU.0b013e3282f154bd
12. Sharma N, Singhal D. Corneal edema after phacoemulsification. Indian J Ophthalmol. 2017;65(12):1381–1389. doi:10.4103/ijo.IJO_871_17
13. Kausar A, Farooq S. Transient corneal edema after phacoemulsification. J Coll Physicians Surg Pak. 2015;25(7):505–509.
14. Yu-Chieh K, Liu CJ-L, Lau L-I, et al. Factors related to corneal endothelial damage after phacoemulsification in eyes with occludable angles. J Cataract Refract Surg. 2008;34(1):46–51. doi:10.1016/j.jcrs.2007.07.057
15. Jin C, Chen X. Different‐sized incisions for phacoemulsification in age‐related cataract. Cochrane Database Syst Rev. 2017;2017(9):CD010510.
16. Liang JL, Xing XL. Clinical comparison analysis in surgically induced astigmatism of the total, anterior and posterior cornea after 2.2-mm versus 3.0-mm clear corneal incision cataract surgery. Zhonghua Yan Ke Za Zhi. 2019;55(7):495–501.
17. Wang J, Zhang EK. The effect of micro-incision and small-incision coaxial phaco-emulsification on corneal astigmatism. Clin Exp Ophthalmol. 2009;37(7):664–669.
18. Borasio E, Mehta JS, Maurino V. Surgically induced astigmatism after phacoemulsification in eyes with mild to moderate corneal astigmatism: temporal versus on-axis clear corneal incisions. J Cataract Refract Surg. 2006;32(4):565–572. doi:10.1016/j.jcrs.2005.12.104
19. Nikose AS, Saha D, Laddha P, et al. Surgically induced astigmatism after phacoemulsification by temporal clear corneal and superior clear corneal approach: a comparison. Clin Ophthalmol. 2018;3(12):65–70. doi:10.2147/OPTH.S149709
20. Dithmar S, Hoeh AE, Amberger R, et al. Light-emitting diode technology in vitreoretinal surgery. Retina. 2011;31:924–927. doi:10.1097/IAE.0b013e3181f44269
21. Behar-Cohen F, Martinsons C, Vienot F, et al. Light-emitting diodes (LED) for domestic lighting: any risks for the eye? Prog Retin EyeRes. 2011;30:239–257. doi:10.1016/j.preteyeres.2011.04.002
22. McDonald HR, Irvine AR. Light-induced maculopathy from the operating microscope in extracapsular cataract extraction and intraocular lens implantation. Ophthalmology. 1983;90:945–951. doi:10.1016/S0161-6420(83)80022-0
23. Kleinmann G, Hoffman P, Schechtman E, et al. Microscope-induced retinal phototoxicity in cataract surgery of short duration. Ophthalmology. 2002;109:334–338. doi:10.1016/S0161-6420(01)00924-1
24. Michels M, Sternberg P
25. Taha S, Altinisik M, Guler EM, et al. Evaluation of xenon, light-emitting diode (LED) and halogen light toxicity on cultured retinal pigment epithelial cells. Cutan Ocul Toxico. 2019;38(2):125–130. doi:10.1080/15569527.2018.1539008
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.