Back to Journals » Open Access Emergency Medicine » Volume 14
Retrospective Analysis of Left Ventricular Thrombus Among Heart Failure Patients with Reduced Ejection Fraction at a Single Tertiary Care Hospital in Somalia
Authors Abdi IA , Karataş M, Öcal L, Elmi Abdi A, Farah Yusuf Mohamud M
Received 6 August 2022
Accepted for publication 20 October 2022
Published 1 November 2022 Volume 2022:14 Pages 591—597
DOI https://doi.org/10.2147/OAEM.S384109
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Ishak Ahmed Abdi,1 Mesut Karataş,1 Lütfi Öcal,1 Ahmed Elmi Abdi,1 Mohamed Farah Yusuf Mohamud2
1Department of Cardiology, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 2Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Mohamed Farah Yusuf Mohamud, Mogadishu Somali-Turkish Training and Research Hospital, 30 Street, Alikamin, Wartanabada District, Mogadishu, Somalia, Tel +252615591689, Email [email protected]
Introduction: Left ventricular thrombus (LVT) is a common complication in patients with systolic heart failure and can cause thromboembolic consequences including stroke. In order to determine the characteristics of LV thrombus among heart failure patients with reduced ejection fraction (HFrEF), the present study was undertaken.
Methods and Materials: This was retrospective cross-sectional study conducted from referral tertiary hospital in a year period. A total of 810 transthoracic echocardiograms were carried out in our center from January 2021 to December 2021. Forty participants had met the inclusion criteria of the study.
Results: About 75% of the population was male and the mean age at diagnosis was 51 years (SD: 15). Ischemic cardiomyopathy and dilated cardiomyopathy (DCMP) found to be the most underlying cause of LVT represented (57.5% and 42.5% respectively). Hypertension, hypothyroidism, and atrial fibrillation were found to be the commonest associated risk factors of LVT, 45%, 12.5%, and 30% respectively. Simpson’s Biplane’s approach yielded a mean LVEF of 25.25 ± 6.97. 60% of the patients had a LVEF of ≤ 25%. The mean LV end-diastolic and end-systolic diameters were 59.2 ± 9.4 mm and 51 ± 8.3mm respectively. Warfarin was administered to 19 (47.5), Rivaroxaban to 8 (20), and Dabigatran to 10 (25). The most prevalent anticoagulant among the individuals in our study was warfarin. A stroke complication was found in 8 patients (20%), two of them were hemorrhagic stroke and they were on dabigatran. A Peripheral Arterial Disease (PAD) affected 6 of the patients (15%). One of those with PAD had also ischemic stroke.
Conclusion: This study determines that Ischemic and Dilated cardiomyopathy were the most common cause of left ventricular thrombosis among HFrEF patients in Somalia.
Keywords: left ventricular thrombus, transthoracic echocardiography, cardiomyopathy, heart failure
Introduction
Left ventricle thrombus (LVT) is a common consequence seen in patients with systolic heart failure and those who have had an acute myocardial infarction (AMI).1,2 Even though the precise mechanism by which the LV thrombus forms is unknown, several hypotheses such as blood stasis, hypercoagulable state, and myocardial injury may partially explain the process.3 The heart is a major source of systemic emboli, with atrial fibrillation (AF), LV thrombus, and prosthetic valves being the most common cardiogenic sources.4 A hypercoagulable state is observed in HF with reduced ejection fraction (HFrEF), with an increased incidence of LV thrombus and a higher risk of thromboembolism.5 Transthoracic echocardiography (TTE) remains the most used imaging modality for diagnosing LVT Because it`s most generally available and comparably less expensive than other imaging modalities such as cardiac CT scan and MRI.6,7
In developed countries, the incidence of LVT has been decreasing.8 Cardiovascular epidemiology on the Africa continent is undergoing a transformation, which is aggravated by a lack of expertise and poor healthcare infrastructures.9,10 Ischemic heart disease and acute coronary syndromes are becoming more common on the continent.11 Unfortunately, delayed presentation and missed MI are prevalent issues, and primary PCI is still unavailable to the great majority of the population.12
In Somalia, the extant of heart failure and left ventricular thrombus have yet to be investigated. The purpose of this study is to determine the frequency, characteristics, etiology, and outcomes of HFrEF patients with LVT who attended Cardiology department of a Tertiary Hospital in Somalia.
Method
This is a cross-sectional retrospective study conducted at Mogadishu Somali Turkish Training and Research hospital between 2021January to December 2021. Medical records of all adults with echocardiographic diagnosis of LVT were retrieved and the patients who were confirmed to have LVT with eligible criteria were included in the study. Eligible Patients were those with LVT, heart failure LVEF < 40% and above 18 years old (Figure 1). Both ambulatory and inpatient patients with LVT were included to the study. Patient`s characteristics, demographics, risk factors, echocardiographic findings and outcomes were assessed. 2D Transthoracic Echocardiography with the standard views were carried out using Toshiba Aplio™ ultrasound system (TUS-A500, Shimo ishigami, Japan) by a senior cardiologist.
 |
Figure 1 Summarized the inclusion and exclusion criteria. |
The presence of thrombus in the left atrium (LA) or right cardiac cavity, Rheumatic Heart disease (RHD), prosthetic valves, infective endocarditis, or cardiac tumors were all considered as exclusion criteria.
On echocardiographic examinations, LV thrombus was defined as a discrete mass in the left ventricle, distinct from the LV endocardium, in a location with corresponding to LV regional or global wall motion abnormality.13 Dilated cardiomyopathy was diagnosed by the presence of global Left ventricle dilatation with LVDd > 56mm and EF < 40%.14
The leading edge to leading edge approach was used to measure the size of the left ventricle.15,16 Hypertensive heart disease (HHD) was diagnosed in hypertensive patients with a history of concentric or eccentric LV hypertrophy or concentric LV remodeling, left atrial dilatation, and/or systolic and/or diastolic dysfunction.17
Prior to the start of data collection, the ethical approval of the institution was acquired with a reference number of MSTH/10261. Patients’ names and other identifiers were not integrated in the research data; instead, a unique code was used to provide a new identification for the subject’s identity. This study was carried out in accordance to the Helsinki Declaration contents.
The data were collected and entered in MS Excel 10. The patient’s codes, age, sex, Echo parameters, comorbidities and medication were all listed in the excel. For statistical analysis, and the data were entered by letter in to the statistical package for social sciences (SPSS) software version 23. Continuous data with a normal distribution is represented by the mean and Standard deviation. Frequencies and percentages are used to present categorical data.
Results
A total of 810 transthoracic echocardiograms were carried out in our center from January 2021 to December 2021. Five hundred seventy individuals were disqualified due to incomplete data, EF > 40, and pediatric populations. Among the remaining HFrEF patients, forty participants had left ventricular thrombus as shown in Table 1.
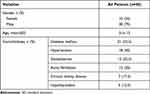 |
Table 1 Demographics and Comorbidities of the Study Patients |
Seventy-five of the population was male and the mean age at diagnosis was 51 years (SD: 15). Twenty-one patients (52.5%) had diabetes, 18 (45%) had hypertension, five (12.5%) had hypothyroidism, seven (17%) patients with chronic renal disease, thirteen (32.5%) had dyslipidemia, and twelve (30%) had atrial fibrillation. The study participants’ demographics and comorbidities are summarized in Table 1.
Simpson’s Biplane’s approach yielded a mean LVEF of 25.25 ± 6.97. Twenty-four (60) of the patients had a LVEF of ≤25%. The mean LV end-diastolic and end-systolic diameters were 59.2 ± 9.4 mm and 51 ± 8.3mm respectively.
The underlying cause of LV dysfunction in the participants was ischemic cardiomyopathy 23 (57.5%), followed by non-ischemic cardiomyopathy 17 (42.5%).
Twenty-one (52.5%) thrombi were located in the apex, 11 (27.5%) along the inferior wall, and 8 (20%) along the anterior wall. In the ischemic patients with LV thrombus, LV aneurysm complicated in 15 (37.5) of our participants. Table 2 summarizes the echocardiographic findings of the study precipitants.
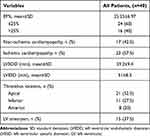 |
Table 2 Echocardiography Findings of the Study Patients (EF<40%) |
Thirty-seven of the 40 patients with an LVT diagnosis were treated with long-term anticoagulation. Due to a concordance of bleeding diathesis, one patient did not get an anticoagulant, and the other two patients passed away in the hospital before receiving oral anticoagulation.
As shown in Table 3, Warfarin was administered to 19 (47.5), Rivaroxaban to 8 (20), and Dabigatran to 10 (25). The most prevalent anticoagulant among the individuals in our study was warfarin.
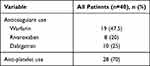 |
Table 3 The Detailed Treatments of the Patients |
A reevaluation in 28 patients (about 70%), echo was performed. Seventeen (42.5%) of the patients experienced complete LVT resolution, whereas 11 individuals continued to experience it (27.5%). A decrease in thrombus size was seen in 4 (36% of the patients) with LVT persistence. In the first year following LVT diagnosis, 12 patients (30%) passed away.
As shown in Table 4, eight patients (20%) had a stroke complication. Six individuals experienced ischemic strokes; three of them were taking dabigatran, two were using warfarin, and one was getting rivaroxaban. Two patients who were on dabigatran were reported to have suffered hemorrhagic strokes. One of those with PAD had also ischemic stroke.
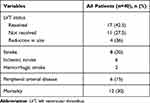 |
Table 4 Status of the Left Ventricular Thrombus and the Outcomes |
Discussion
This study was conducted over a year period at the Mogadishu Somalia Education and Research Specialist Hospital; we reported the prevalence rate for LVT among patients with low EF. The participants in our study had a mean age of 51 ± 15 years. Male patients made up most of the patients (75%). This age and gender distribution trend is consistent with a wide range of earlier studies.18 In this study we found LV thrombus in 16% of the patients. This frequency is higher than those reported by Aljaber et al19 and Talle et al,12 respectively, for Yemen (6.1%) and Nigeria (8.85%). To our knowledge, this is the first study on the prevalence of LVT among heart failure patients from Somalia.
In our study, 57% of participants were associated with ischemic heart disease (IHD). This result is consistent with that of Aljaber et al19 and Khaled et al,20 who discovered that the prevalence of IHD in people with left ventricle thrombus and HFrEF was 50% and 51%, respectively.
In our study, we discovered that the majority of thrombi (52.5%) were located in the apex, which is consistent with reports from Adar et al21 and Aljaber et al19 that LV thrombus frequently occurred in the LV apex. Benito discovered that the apex of the ventricle is the most prone to blood stasis, which explained why thrombi typically form there.22 More patients in our study (n = 18) had uncontrolled hypertension, which is a well-documented risk factor for heart failure and has also been suggested to play a significant role in the hypercoagulable state that affects all three factors of the Virchow triad and can be a prodrome for LV thrombus formation.23
Thromboembolic consequences from left ventricular thrombus affected 40% of patients in our study, which is much greater than the studies reported from Nigeria (8.85%) and Yemen (28.1%).12,20 This difference can be attributed to the fact that patients in our study did not adhere their medications, as well as to some risk factors were present in our study that were not taken into account in other studies, such as hypothyroidism and atrial fibrillation, which is thought to be a factor in the development of left ventricular thrombus.24,25
One of the major complications associated with left ventricle aneurysm is the development of thrombus, which can result in embolization to other organs like the brain.26 In the current study, 15 patients had left ventricle aneurysm which is also believed to play a significant role in the pathology of generation of thrombus.
This research will serve as a foundation for future research in the management of left ventricular thrombus in the African population. The article’s limitations include a small sample size, a retrospective single experience center, and technical deficiencies in echocardiography, such as the measurement of thrombus mass mobility by pulse wave Doppler, which is a prognostic indicator for hospitalized patients.27,28 Overall, these results cannot be generalized to the entire population due to these limitations. The epidemiological findings of LVT in heart failure at the continental and national levels should be supported by larger-scale studies in the future. Additionally, CMRI and contrast echo are more sensitive and specific than echocardiography for the identification of left thrombus.29
In conclusion, this study provides important insights into frequency, characteristics, and outcomes of left ventricular thrombus among heart failure patients with reduced ejection fraction in a single referral hospital in Somalia. Ischemic and Dilated cardiomyopathy were the most common cause of left ventricular thrombosis among heart failure patients with reduced ejection fraction in Somalia.
Regarding to the above obtained findings, the authors conclude that thrombus is present in considerable proportion among heart failure population and that there is emerging predisposing factors such hypothyroidism. However, additional researches are recommended.
Data Sharing Statement
The data is available from the corresponding author and can be accessed if requested.
Ethics Approval and Consent to Participate
This study was reviewed and approved by Mogadishu Somali Turkish Training and Research Hospital ethic committee (Ref. MSTH/10261), patient’s informed consent was waived by the Institutional Review Board because the data was acquired retrospectively from medical records and the patient’s data confidentiality was respected.
Consent for Publication
All authors gave their consent for this case study to be published.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
We declare that we have no funding source.
Disclosure
We declare that we have any no competing of interest.
References
1. Asinger RW, Mikell FL, Elsperger J, Hodges M. Incidence of left-ventricular thrombosis after acute transmural myocardial infarction: serial evaluation by two-dimensional echocardiography. N Engl J Med. 1981;305(6):297–302. doi:10.1056/NEJM198108063050601
2. Kalra A, Jang IK. Prevalence of early left ventricular thrombus after primary coronary intervention for acute myocardial infarction. J Thromb Thrombolysis. 2000;10(2):133–136. doi:10.1023/A:1018710425817
3. Delewi R, Zijlstra F, Piek JJ. Left ventricular thrombus formation after acute myocardial infarction. Heart. 2012;98(23):1743–1749. doi:10.1136/heartjnl-2012-301962
4. Celeste F, Muratori M, Mapelli M, Pepi M. The evolving role and use of echocardiography in the evaluation of cardiac source of embolism. J Cardiovasc Echogr. 2017;27(2):33. doi:10.4103/jcecho.jcecho_1_17
5. Lip GY, Gibbs CR. Does heart failure confer a hypercoagulable state? Virchow’s triad revisited. J Am Coll Cardiol. 1999;33(5):1424–1426. doi:10.1016/s0735-1097(99)00033-9
6. Visser CA, Kan G, David GK, Lie KI, Durrer D. Two dimensional echocardiography in the diagnosis of left ventricular thrombus: a prospective study of 67 patients with anatomic validation. Chest. 1983;83(2):228–232. doi:10.1378/chest.83.2.228
7. Cacciapuoti F, Varricchio M, D’Avino M, Gentile S, Lama D, Cotrufo M. Post-necrotic endoventricular thrombosis. Comparative evaluation of the diagnostic reliability of 2-dimensional echocardiography and cineventriculography. G Ital Cardiol. 1986;16(4):344–349.
8. McCarthy CP, Murphy S, Venkateswaran RV, et al. Left ventricular thrombus: contemporary etiologies, treatment strategies, and outcomes. J Am Coll Cardiol. 2019;73(15):2007–2009. doi:10.1016/j.jacc.2019.01.031
9. Mensah GA, Sampson UK, Roth GA. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015;26(2):S6. doi:10.5830/CVJA-2015-036
10. Varwani MH, Ngunga M, Jeilan M, Barasa A. Outcomes in patients with acute coronary syndrome in a referral hospital in sub-Saharan Africa. Cardiovasc J Afr. 2019;30(1):29–33. doi:10.5830/CVJA-2018-066
11. Lattuca B, Bouziri N, Kerneis M, et al. Antithrombotic therapy for patients with left ventricular mural thrombus. J Am Coll Cardiol. 2020;75(14):1676–1685. doi:10.1016/j.jacc.2020.01.057
12. Talle MA, Buba F, Anjorin CO. Prevalence and aetiology of left ventricular thrombus in patients undergoing transthoracic echocardiography at the University of Maiduguri Teaching Hospital. Adv Med. 2014;2014:1–8. doi:10.1155/2014/731936
13. Saric M, Armour AC, Arnaout MS, et al. Guidelines for the use of echocardiography in the evaluation of a cardiac source of embolism. J Am Soc Echocardiogr. 2016;29(1):1–42. doi:10.1016/j.echo.2015.09.011
14. Armstrong WF, Ryan T. Dilated Cardiomyopathy. In: Feigenbaum’s Echocardiography.
15. Billingsley IM, Leong-Poi H. Left ventricular thrombus: diagnosis, prevention and management. Cardiol Rounds. 2005;10(7):1–6.
16. Armstrong WF, Ryan T. Masses, tumors and source of embolism. In: Feigenbaum’s Echocardiography; 2010:711–740.
17. de Simone G, Daniels SR, Devereux RB, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20(5):1251–1260. doi:10.1016/0735-1097(92)90385-Z
18. Iqbal MW, Fayyaz A, Hanif A. Frequency of left ventricular thrombus after anterior wall ST-segment elevation acute Myocardial infarction. Ann King Edward Med Univ. 2014;20(1):68.
19. Aljaber NN, Mattash ZA, Alshoabi SA, Alhazmi FH. The prevalence of left ventricular thrombus among patients with low ejection fraction by trans-thoracic echocardiography. Pak J Med Sci. 2020;36(4):673. doi:10.12669/pjms.36.4.1972
20. Khaled A, Faiza A. The prevalence of left ventricular thrombus among heart failure patients admitted to Kuwait Teaching Hospital in Sanaa City between January 2014–2017. Nurs Health Care. 2019;4:29–34. doi:10.33805/2573-3877.134
21. Adar A, Onalan O, Cakan F. Newly developed left ventricular apical thrombus under dabigatran treatment. Blood Coagul Fibrinolysis. 2018;29(1):126–128. doi:10.1097/MBC.0000000000000671
22. Benito Y, Martinez-Legazpi P, Rossini L, et al. Age-dependence of flow homeostasis in the left ventricle. Front Physiol. 2019;10:485. doi:10.3389/fphys.2019.00485
23. Lip GY. Hypertension and the prothrombotic state. J Hum Hypertens. 2000;14(10):687–690. doi:10.1038/sj.jhh.1001051
24. Van Treeck BJ, Masoud AG. Hypothyroid cardiomyopathy complicated by a left ventricular laminar thrombus. Mo Med. 2014;111(5):444.
25. Bourezg A, Bochaton T, Mewton N, et al. Atrial fibrillation, intra-ventricular thrombus, and other anticoagulant indications relationship with adverse outcomes in acute anterior myocardial infarction patients. J Cardiol. 2018;72(4):277–283. doi:10.1016/j.jjcc.2018.03.008
26. Sattar Y, Alraies MC. Ventricular aneurysm. In: StatPearls [Internet]. StatPearls Publishing; 2021.
27. Sonaglioni A, Nicolosi GL, Lombardo M, Anzà C, Ambrosio G. Prognostic relevance of left ventricular thrombus motility: assessment by pulsed wave tissue Doppler imaging. Angiology. 2021;72(4):355–363. doi:10.1177/0003319720974882
28. Sonaglioni A, Albini A, Nicolosi GL, Rigamonti E, Noonan DM, Lombardo M. Case report: an unusual case of biventricular thrombosis in a COVID-19 patient with ischemic dilated cardiomyopathy: assessment of mass mobility and embolic risk by tissue Doppler imaging. Front Cardiovasc Med. 2021;8. doi:10.3389/fcvm.2021.694542
29. Varwani MH, Shah J, Ngunga M, Jeilan M. Treatment and outcomes in patients with left ventricular thrombus-experiences from the Aga Khan University Hospital, Nairobi-Kenya. Pan Afr Med J. 2021;39(1). doi:10.11604/pamj.2021.39.212.28585
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
