Back to Journals » International Medical Case Reports Journal » Volume 15
Retrograde CTO-PCI Using an Internal Thoracic Bypass Graft Segment in a Patient with Acute Inferior ST-Elevation Myocardial Infarction and Cardiogenic Shock
Authors Ungureanu C , Colletti G, Blaimont M, Avran A
Received 23 April 2022
Accepted for publication 17 August 2022
Published 15 September 2022 Volume 2022:15 Pages 499—505
DOI https://doi.org/10.2147/IMCRJ.S370231
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Claudiu Ungureanu,1 Giuseppe Colletti,1 Marc Blaimont,1 Alexandre Avran2
1Department of Cardiology, Jolimont Hospital, La Louvière, Belgium; 2Department of Cardiology, Clinique Pasteur Essey les Nancy, Nancy, France
Correspondence: Claudiu Ungureanu, Department of Cardiology, Jolimont Hospital, Rue, Ferrer, 159, La Louvière, Belgium, Tel +32495489442, Email [email protected]
Background: Percutaneous coronary intervention (PCI) of the “culprit” artery is the recommended mechanical reperfusion strategy in the setting of ST-segment elevation myocardial infarction (STEMI). As PCI of bypass grafts may be associated with higher risks and lower procedural success rates, in patients with a history of previous coronary artery surgery, PCI directed at revascularization of the native vessels should be considered, but this may be difficult in the setting of a chronically occluded artery.
Case Presentation: A patient with a history of multivessel coronary artery disease and a chronic total occlusion (CTO) of the right coronary artery (RCA) requiring arterial bypass surgery, presented with an acute inferior STEMI and cardiogenic shock. It was felt that shock was caused by the acute thrombotic occlusion of a right internal thoracic artery (RITA) bypass graft that had been sequentially anastomosed to the left circumflex (LCx) and right coronary arteries. Despite initiation of extracorporeal membrane oxygenation (ECMO), the patient remained in refractory shock and acute revascularization of the right coronary artery was performed through the RITA bypass segment using antegrade access to the graft through the LCx and then a retrograde approach to open a CTO of the RCA. After successful revascularization, the patient was successfully weaned from ECMO. Over 12 months of follow-up, the patient did well and was documented to have improved left ventricular systolic function.
Conclusion: This report is the first to document the successful use of a retrograde approach through an arterial graft segment to revascularize a chronic total occlusion in the setting of acute STEMI and cardiogenic shock.
Keywords: chronic total occlusion, STEMI, rotational atherectomy, coronary bypass
Introduction
Urgent percutaneous coronary revascularization is the standard care for patients presenting with acute myocardial infarction (STEMI) and associated cardiogenic shock.1 Clinical outcomes have dramatically improved after the increased use of revascularization by primary PCI.2,3 However, catheter-based revascularization may be difficult to perform in the setting of a chronically totally occluded vessel (CTO) and a culprit lesion in a coronary artery bypass graft (CABG).4,5 Technical success has been lower, and the incidence of adverse events has been documented to be higher among patients with prior CABG undergoing elective CTO PCI.6
Case Presentation
A 62-year-old male with a history of 3 vessel coronary disease and prior coronary artery surgery was admitted with an inferior STEMI and cardiogenic shock, 6 hours after the onset of symptoms. Twelve months earlier, the patient had undergone a failed attempt of anterograde CTO RCA PCI, followed by an arterial bypass graft placement using a LITA graft to the left anterior descending artery (LAD) and a RITA graft sequentially to the obtuse marginal branch of the left circumflex and the RCA arteries.
The patient was diagnosed with an acute thrombotic occlusion of the RITA graft at its ostium and a patent LITA to the LAD artery. The posterior-descending artery (PDA) was also occluded. The patient was in refractory cardiogenic shock and was placed on ECMO. Concerns were raised that antegrade interventions through the RITA graft could result in distal thrombus embolization and acute revascularization was attempted using an antegrade approach from the native LCx into the RITA graft segment to the PDA and then a retrograde approach through the native RCA CTO.
The procedure was successful after the retrograde crossing of the remaining RITA graft (between the obtuse marginal and the PDA), retrograde dissection re-entry technique, externalization, rotational atherectomy of the lesion, and implantation of 3 drug-eluting stents.
The clinical evolution of the patient was favorable after the intervention and at 12 months follow-up.
Past Medical History
The patient had a history of diabetes, dyslipidemia, mild renal insufficiency and left ventricular systolic dysfunction with a LVEF of 45%.
Acute Presentation
The patient presented to the emergency department in cardiogenic shock with a blood pressure of 77/50 mm Hg and a pulse rate of 102 beats per minute. The patient was in a poor overall condition, the skin was pale, cool and diaphoretic.
An initial electrocardiogram (ECG) revealed 2 mm ST elevations in the inferior leads and ST segment depression in leads V1-2 (Figure 1). These findings are consistent with inferior and posterior injury.
 |
Figure 1 ECG tracing recorded in the ambulance: 2mm ST elevation in inferior leads (see blue circles). |
An echocardiogram obtained on initial presentation documented severe left ventricular systolic dysfunction with limited basal inferior akinesia, severe hypokinesia in the anterior and inferolateral wall, and an LVEF of 20%. There was evidence of moderate mitral regurgitation, right ventricular dilatation, and systolic dysfunction.
Urgent coronary angiography was performed and the patient was started on ECMO immediately because of cardiogenic shock status despite pharmacological support. An intra-aortic balloon pump (IABP) was not preferred as a first choice regarding the stage D cardiogenic shock and the need for optimal perfusion in this acute coronary syndrome. A potential higher risk of mortality in acute settings could be related to the limited hemodynamic benefit of the IABP in comparison to other mechanical devices.7–9
The patient was documented to have a CTO of the RCA (Figure 2) and an occluded proximal LAD after the origin of the first diagonal branch. The LITA graft to the LAD was patent (Figure 3), and there was an acute ostial occlusion of the RITA graft. The ostial circumflex showed 80% lesion and the segment of the RITA graft between the left circumflex and the PDA artery was widely patent but with an occlusion in the native PDA vessel related probably to thrombotic embolization (Figure 4).
 |
Figure 2 Angiogram (projection LAO 30 °/ CRA 0°): chronic total occlusion of the mid RCA. Blunt and ambiguous proximal cap, length of 30mm, severely calcified (JCTO 4). |
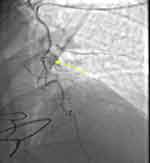 |
Figure 3 Angiogram (projection LAO 5°, CRA 0°): patent LITA to LAD. Ostial occlusion of RITA at the level of Y connection (see the yellow arrow). |
Management
Flow to the distal PDA and the posterolateral artery (PL) was absent and attempts were made to establish the reperfusion of these vessels.
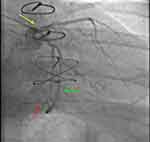
The RCA was chronically occluded and revascularization was attempted by bilateral sheathless distal radial artery access with 7Fr guiding catheters. Knowing that the anterograde true to true lumen approach had previously failed we performed an anterograde knuckle with Fielder XTR (Asahi Intecc, Japan) supported by 7Fr TrapLiner (Teleflex Medical Incorporated, US) and Corsair Pro 135cm (Asahi Intecc, Japan). The retrograde Sion (Asahi Intecc, Japan) wire supported by a Corsair Pro 150 cm microcatheter was able to pass through the remaining anastomosis between the RITA and the obtuse marginal to the distal anastomosis with the PDA (Figure 5). The guideliner reverse CART was successful after the retrograde Gaia 3 wire crossed and the externalization was made using an RG3 wire (Asahi Intecc, Japan).
Due to the severity and the extension of calcium the balloon failed to open and we performed a rotational atherectomy (Figure 6) after crossing the CTO with an anterograde microcatheter on the RG3 and exchanging it with an extra support Rota Wire.
 |
Figure 6 Rotational atherectomy. Angiogram (projection RAO 25°, CAUD 2°): rotational atherectomy using a 1.5 Burr (see the yellow arrow) through an extra support rota wire. |
The procedure was successful after implantation of 3 drug-eluting stents (Figure 7). The first stent was placed from the distal RCA to PDA using a provisional technique. The second stent was placed on the mid part of the RCA by overlapping with the first one and the third one on the proximal part of the RCA. The intervention was completed within 2 hours and 40 minutes.
 |
Figure 7 Angiogram (projection LAO 5°, CRA 0°): final angiographic result after 3 drug eluting stents’ implantation with TIMI 3 flow in the distal PAD et posterolateral artery. |
Follow-Up
After 12 months of clinical follow-up the patient had mild NYHA II (New York Heart Association) dyspnea without angina.
The echocardiography revealed an improvement of ventricular function (40% EF).
Discussion
This case represents a complex clinical situation with an acute STEMI and shock caused by a CTO of the RCA and an acute occlusion of a RITA graft to the RCA. The approach of using antegrade wiring of the bypass graft segment to enter the RCA and then performing a retrograde RCA CTO intervention has not been previously described in the setting of an acute infarction.
Total arterial revascularization (TAR) and the use of both arterial thoracic arteries have been shown to improve the short- and long-term mortality in patients undergoing CABG when compared to those undergoing revascularization with a single arterial graft and vein grafts.10 The early patency at 12 months is between 93–96% for internal thoracic artery grafts. In a previous study the rate of occlusion of the arterial grafts was significantly lower than for the venous grafts.11 Accordingly, the use of both LITA and RITA grafts for coronary revascularization has been increasing.12 There is limited data in the literature regarding the management of the acute closure of arterial grafts during a STEMI. In patients with acute coronary syndromes (ACS), revascularization of arterial grafts is more complex and is associated with higher rates of procedural failure and complications when compared with patients without prior surgery.5
CTO PCI for post-CABG patients is more difficult, even in elective cases, needing more contrast and higher doses of radiation, and is associated with a higher risk of adverse events at 12 months.13 The use of CTO PCI algorithms and techniques that are normally employed for elective cases could increase the rate of success of PCI in highly selected patients with acute myocardial infarction.14 In our case, we were not able to precisely detect the location of the anastomosis between the LITA and RITA arterial graft, therefore, any attempt to recanalize it seemed technically very challenging.
Given the patient’s presentation with an acute inferior infarction and cardiogenic shock, attempts were then directed at re-establishing blood flow to the inferolateral LV by opening a right CTO.
PCI CTO procedures are usually performed electively to allow adequate time for procedural planning and preparation,15 but in this particular setting of STEMI and refractory cardiogenic shock, an impromptu approach may be required.
A primary retrograde approach was performed in the presence of a complex CTO with a (Japan CTO score) J-CTO13 at 4 (proximal cap ambiguity, length of the occlusion, calcifications and retry). The retrograde crossing was easily achieved via the left system using the remaining arterial graft between the obtuse marginal and the PDA. In cases of retrograde approach, the easiest and safest collateral is the venous graft for post-CABG patients16 but in our case, the arterial graft was large and straight enough to allow crossing with a regular microcatheter.
Retrograde dissection and re-entry is the most commonly used retrograde crossing technique17,18 and was also preferred in our case. After externalization, the lesion was prepared by rotational atherectomy.
After PCI the ECG and hemodynamic status of the patient improved significantly. The patient was successfully weaned from ECMO only 6 hours after opening the RCA. The renal function recovered rapidly 24h after the procedure. The total amount of contrast was limited by the retrograde technic that allowed us the realization of almost all PCI steps without additional contrast administration. Acute kidney injury needs to be limited as much as possible knowing that it could negatively impact the prognosis of the patients.
Our case is unique in that it is the only case, to our knowledge, that describes the effective treatment of cardiogenic shock due to an acute inferior posterior STEMI in a patient with a history of RCA CTO using retrograde percutaneous interventions performed through an arterial graft segment from the left circumflex coronary artery to the distal RCA.
Conclusion
The use of arterial bypass grafts for coronary revascularization is increasing. Accordingly, in the future, there will likely be an increase in the number of patients with arterial bypass grafts who present with acute STEMIs requiring emergency percutaneous revascularization. This report documents the unique use of an approach for acute PCI using the native left circumflex artery and an arterial graft segment to provide access to the RCA to allow retrograde CTO interventions. Our patient presented with an acute inferior STEMI and cardiogenic shock but was stabilized after revascularization. While this case may be unusual, it demonstrates that alternative approaches of revascularization may be needed in patients with previously placed arterial coronary bypass grafts and acute myocardial infarctions.
Patient Consent
The patient provided informed consent for publication of their case details and any accompanying images, Institutional approval was not required to publish the case details.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eurointervention. 2019;14(14):1435–1534. doi:10.4244/EIJY19M01_01
2. Szummer K, Wallentin L, Lindhagen L, et al. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995–2014. Eur Heart J. 2017;38(41):3056–3065. doi:10.1093/eurheartj/ehx515
3. Labinaz Terri Swabey M, Watson R, Watson R, et al. Delivery of primary percutaneous coronary intervention for the management of acute ST segment elevation myocardial infarction: summary of the cardiac care network of ontario consensus report. Can J Cardiol. 2006;22(3):243–250. doi:10.1016/S0828-282X(06)70904-7
4. Blachutzik F, Achenbach S, Troebs M, et al. Angiographic findings and revascularization in patients with acute myocardial infarction and previous coronary bypass grafting. Am J Cardiol. 2016;118(4):473–476. doi:10.1016/j.amjcard.2016.05.040
5. Deharo P, Strange JW, Mozid A, et al. Primary percutaneous coronary intervention of native chronic total occlusions to treat ST elevation myocardial infarction secondary to acute vein graft occlusion. Catheter Cardiovasc Interv. 2013;90(2):251–256. doi:10.1002/ccd.26905
6. Nikolakopoulos I, Choi JW, Jaikirshan JK, et al. Follow-up outcomes of chronic total occlusion percutaneous coronary interventions in patients with and without prior coronary artery bypass graft surgery: insights from the Progress-CTO Registry. J Invasive Cardiol. 2020;32(8):315–320.
7. Baran DA, Long A, Badiye AP, Stelling K. Prospective validation of the SCAI shock classification: single center analysis. Catheter Cardiovasc Interv. 2020;96:1339–1347. doi:10.1002/ccd.29319
8. Thiele H, De waha-thiele S, Freund A, Zeymer U, Desch S, Fitzgerald S. Management of cardiogenic shock. EuroIntervention. 2021;17:451–465. doi:10.4244/EIJ-D-20-01296
9. Ilker Hayıroğlu M, Çanga Y, Yıldırımtürk Ö. Clinical characteristics and outcomes of acute coronary syndrome patients with intra-aortic balloon pump inserted in intensive cardiac care unit of a tertiary clinic. Turk Kardiyol Dern Ars. 2018;46(1):10–17. doi:10.5543/tkda.2017.11126
10. Buxton BF, Shi WY, Tatoulis J, Fuller JA, Rosalion A, Hayward PA. Total arterial revascularization with internal thoracic and radial artery grafts in triple-vessel coronary artery disease is associated with improved survival. J Thorac Cardiovasc Surg. 2014;148:1238–1244. doi:10.1016/j.jtcvs.2014.06.056
11. Goldman S, Zadina K, Moritz T, et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a department of veterans affairs cooperative Study. J Am Coll Cardiol. 2004;44:2149–2156. doi:10.1016/j.jacc.2004.08.064
12. Saran N, Locker C, Said SM, et al. Current trends in bilateral internal thoracic artery use for coronary revascularization: extending benefit to high-risk patients. J Thorac Cardiovasc Surg. 2018;155(6):2331–2343. doi:10.1016/j.jtcvs.2018.01.094
13. Dautov R, Nguyen CM, Altisent O, Gibrat C, Rinfret S. Recanalization of chronic total occlusions in patients with previous coronary bypass surgery and consideration of retrograde access via saphenous vein grafts. Circ Cardiovasc Interv. 2016;9:1–12. doi:10.1161/CIRCINTERVENTIONS.115.003515
14. Xenogiannis I, Nikolakopoulos I, Vemmou E, Brilakis ES. Chronic total occlusion recanalization for myocardial infarction. Catheter Cardiovasc Interv. 2020;95(6):1133–1135. doi:10.1002/ccd.28590
15. Brilakis ES, Mashayekhi K, Tsuchikane E, et al. Guiding principles for chronic Total occlusion percutaneous coronary intervention. Circulation. 2019;140:420–433. doi:10.1161/CIRCULATIONAHA.119.039797
16. Xenogiannis I, Gkargkoulas F, Karmpaliotis D. Retrograde chronic total occlusion percutaneous coronary intervention via saphenous vein graft. J Am Coll Cardio Intv. 2020;13:517–526. doi:10.1016/j.jcin.2019.10.028
17. Matsuno S, Tsuchikane E, Harding SA, et al. Overview and proposed terminology for the reverse controlled antegrade and retrograde tracking (reverse CART) techniques. Euro-Intervention. 2018;14(1):94–101. doi:10.4244/EIJ-D-17-00867
18. Hayıroğlu EB, Yıldırımtürk Ö, Ilker Tekkeşin A, Pehlivanoğlu S. Effect of acute kidney injury on long-term mortality in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock who underwent primary percutaneous coronary intervention in a high-volume tertiary center. Turkish Soc Cardiol. 2020;48:1–9.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.