Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Respiratory muscle strength effect on linear and nonlinear heart rate variability parameters in COPD patients
Authors Goulart CDL , CRISTIANO SIMON J, De Borba Schneiders P, Antunes San Martin E, Cabiddu R, BORGHI-SILVA A , TRIMER R, da Silva ALG
Received 20 March 2016
Accepted for publication 14 April 2016
Published 26 July 2016 Volume 2016:11(1) Pages 1671—1677
DOI https://doi.org/10.2147/COPD.S108860
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Cássia Da Luz Goulart,1 Julio Cristiano Simon,1 Paloma De Borba Schneiders,1 Elisabete Antunes San Martin,1 Ramona Cabiddu,2 Audrey Borghi-Silva,2 Renata Trimer,2 Andréa Lúcia Gonçalves da Silva1
1Course of Physiotherapy, Department of Health and Physical Education, University of Santa Cruz do Sul (UNISC), Santa Cruz do Sul, Rio Grande do Sul, Brazil; 2Cardiopulmonary Physiotherapy Laboratory, Nucleus of Research in Physical Exercise, Federal University of São Carlos (UFSCar), São Carlos, São Paulo, Brazil
Introduction: Chronic obstructive pulmonary disease (COPD) is recognized as a multisystemic inflammatory disease associated with extrapulmonary comorbidities, including respiratory muscle weakness and cardiovascular and cardiac autonomic regulation disorders. We investigated whether alterations in respiratory muscle strength (RMS) would affect cardiac autonomic modulation in COPD patients.
Methods: This study was a cross-sectional study done in ten COPD patients affected by moderate to very severe disease. The heart rate variability (HRV) signal was recorded using a Polar cardiofrequencimeter at rest in the sitting position (10 minutes) and during a respiratory sinus arrhythmia maneuver (RSA-M; 4 minutes). Linear analysis in the time and frequency domains and nonlinear analysis were performed on the recorded signals. RMS was assessed using a digital manometer, which provided the maximum inspiratory pressure (Pimax) and the maximum expiratory pressure (Pemax).
Results: During the RSA-M, patients presented an HRV power increase in the low-frequency band (LFnu) (46.9±23.7 vs 75.8±27.2; P=0.01) and a decrease in the high-frequency band (HFnu) (52.8±23.5 vs 24.0±27.0; P=0.01) when compared to the resting condition. Significant associations were found between RMS and HRV spectral indices: Pimax and LFnu (r=-0.74; P=0.01); Pimax and HFnu (r=0.74; P=0.01); Pemax and LFnu (r=-0.66; P=0.01); Pemax and HFnu (r=0.66; P=0.03); between Pemax and sample entropy (r=0.83; P<0.01) and between Pemax and approximate entropy (r=0.74; P=0.01). Using a linear regression model, we found that Pimax explained 44% of LFnu behavior during the RSA-M.
Conclusion: COPD patients with impaired RMS presented altered cardiac autonomic control, characterized by marked sympathetic modulation and a reduced parasympathetic response; reduced HRV complexity was observed during the RSA-M.
Keywords: COPD, heart rate, muscle strength, autonomic nervous system, sinus arrhythmia
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent and progressive airflow limitation resulting from abnormal inflammatory response of the airways and lungs to noxious particles inhalation.1 Apart from inducing lung damage, COPD is recognized as a multisystemic inflammatory disease associated with extrapulmonary comorbidities that can substantially affect the disease prognosis.1,2 The prevalence of comorbidities in COPD patients ranges between 65% and 81%,2 and they represent the primary causes of death in more than 60% of COPD patients.3 Specifically, the prevalence of cardiovascular disorders in COPD patients is ~40%;2 such disorders are directly associated with cardiac autonomic regulation.4,5
The integration of the cardiovascular, respiratory, and muscular systems constitutes a complex and sophisticated mechanism of energy generation6 in which the cardiovascular system activity, aiming at organic homeostasis preservation, is controlled by the autonomous nervous system (ANS).7 However, cardiorespiratory disorders, such as COPD, can induce changes in the sympathovagal balance, which can result in detrimental alterations in the ANS functioning of these patients.5 The heart rate variability (HRV) analysis is an important tool for the assessment of the ANS behavior,8 used to determine pathological conditions and investigate physiological modifications, which can be associated with physical exercise performance.6,8
Reduced HRV is associated with increased morbidity and mortality in COPD patients,4,5 and this has led various researchers to investigate the ANS behavior during respiratory maneuvers, position changes, and pharmacological blockade.9 It is widely known that in COPD patients the HRV is reduced, and postural adjustments, which induce a predominantly sympathetic stimulation, are also impaired. However, the number of studies that evaluated the parasympathetic component is scarce.10
The heart rate (HR) follows an oscillatory pattern synchronized with the respiratory cycle; this phenomenon is known as respiratory sinus arrhythmia (RSA). During inspiration, HR increases mainly due to the vagal withdrawal effect on the sinus node, while, during expiration, parasympathetic activity is regulated and HR decreases. RSA significantly decreases the sympathovagal balance, markedly increasing vagal modulation on the sinus node.11
Recent studies investigated the relationship between respiratory muscle strength (RMS) and HRV in COPD patients and showed that respiratory muscle weakness can modify the HRV. However, this alteration still needs to be quantified; this could lead to an improvement of therapeutic treatment in pulmonary rehabilitation programs.12,13 Starting from this evidence, we investigated if alterations in RMS may affect cardiac autonomic modulation in COPD patients. We hypothesized that respiratory muscle weakness negatively affects HRV at rest and during an RSA maneuver (RSA-M) in COPD patients.
Methods
Study design
We performed a cross-sectional case study on a convenience nonprobability sample; the study was conducted within Santa Cruz Hospital’s Pulmonary Rehabilitation Program (Santa Cruz do Sul, RS, Brazil). The study was approved by the Research Ethics Committee of the University of Santa Cruz do Sul, protocol number 1.100.926, and all volunteers signed an informed consent statement prior to participation.
Subjects
Ten patients with a clinical diagnosis of COPD, confirmed by pulmonary function test, participating in a pulmonary rehabilitation program and without disease exacerbation for at least 30 days were included in the study. Patients with complex cardiac arrhythmias, unstable angina, uncontrolled systemic arterial hypertension, or myocardial ischemia were excluded from the study.
Measurements
Patients were evaluated in a laboratory at a temperature of 22°C and relative humidity between 50% and 60%. They were instructed to avoid stimulants and alcoholic drinks and not to perform exhausting physical exercise the day before the test; they were also instructed not to smoke or use bronchodilators for 6 hours before the test. Baseline variables, including systolic arterial pressure, diastolic arterial pressure, HR, respiratory frequency, and peripheral oxygen saturation, were measured. Clinical data including sex, age, body mass index, ethnicity, COPD stage,3 and smoking status were also collected.
Pulmonary function
Pulmonary function was assessed using a digital spirometer (Microloop®, MK8, Care Fusion, Hoechberg, Germany), which provided measures of the slow vital capacity, the forced vital capacity (FVC), the forced expiratory volume in 1 second (FEV1), and the FEV1/FVC ratio. Spirometry was performed according to the recommendations of the American Thoracic Society,14 and the results were analyzed according to the values predicted by Pereira et al.15 The classification of severity of airflow limitation in COPD was performed according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations1 and patients were classified as moderate (GOLD II), severe (GOLD III), or very severe (GOLD IV).
Respiratory muscle strength
RMS was assessed using a digital manometer (MDI®, MVD300, Porto Alegre, Brazil), which provided measures of the maximum inspiratory pressure (PImax) and the maximum expiratory pressure (PEmax). The assessment was performed according to the recommendations for the Brazilian population. The Pimax followed by Pemax was obtained from residual volume and total lung capacity; during the maneuver, the subjects remained seated, wearing nose clips and with a rigid, plastic flanged mouthpiece in place.16 The values were then compared with those described in literature and expressed as percentage of predicted values.16
Heart rate variability
HR and RR intervals were recorded using a telemetric cardiac monitor (Polar® S810i, Kempele, Finland) at rest (10 minutes) and during an RSA-M (4 minutes). Recorded signals contained at least 256 points.17 An elastic band (Polar T31 transmissor) was placed around the patient’s thorax at the level of the lower third of the sternum while the patient was in sitting position, and signals were continuously transmitted to the receiving unit by an electromagnetic field. Recorded data were then transferred to the Kubios HRV® analysis software (version 2.2, Matlab Kuopio, Finland) for subsequent analysis.
For HRV recording during the RSA-M, subjects were instructed to perform a series of deep and slow inspirations and expirations, with a pulmonary volume that varied from the total lung capacity (maximal inspiration) to the residual volume (maximal expiration); each respiratory cycle was performed in 10 seconds, with a 5-second inspiration and a 5-second expiration, resulting in five to six respiratory cycles per minute.18
Frequency domain, time domain, and nonlinear analysis were performed on signals recorded at rest and during the RSA-M. Time domain analysis provided mean RR, standard deviation (SD) RR, mean HR, SD HR, the square root of the mean-squared differences of successive HR and RR intervals, and the RR tri-index. Spectral analysis provided the HRV signal power in the low-frequency (LF) and in the high-frequency (HF) bands, expressed in normalized units (nu), and the LF/HF ratio. Nonlinear analysis provided the approximate entropy (ApEn) and the sample entropy (SampEn) indices.
Statistical analysis
Data were analyzed using the Sigmaplot® statistical package (version 11.0, Systat Software Inc., San Jose, CA, USA). The results were analyzed for normality through the Shapiro–Wilk test and presented descriptively as mean and standard deviation (parametric) or as median and minimum and maximum interval (nonparametric). To reject the null hypothesis, the Student’s t-test was used for parametric data and the Mann–Whitney test was used for nonparametric data. Spearman’s correlation analysis was performed to investigate the correlations between variables. A linear regression model was used to determine the RMS effect on the HRV. Residuals were evaluated under the assumptions of normality, constant variance, and independence. P≤0.05 was considered significant.
Results
A total of 12 COPD patients were recruited; two patients who presented arrhythmias were excluded during the screening phase. Clinical characteristics of patients included in the study are listed in Table 1. Data are in line with others found in literature, with the exception of the number of COPD patients with obesity.
  | Table 1 COPD patients’ clinical characteristics |
Spectral and complexity HRV indices were significantly different between the resting condition and the RSA-M (Table 2). Our results showed that the RSA-M did not modify the time domain of HRV parameters (P>0.05). However, in the frequency domain, interestingly, the LF power and the LF/HF ratio increased (P=0.01), while the HF power decreased (P=0.01). This behavior suggests a sympathovagal modulation contrary to what is expected during the RSA-M. Moreover, ApEn and SampEn significantly decreased, indicating an HRV complexity decrease during the RSA-M.
Figure 1 shows the correlations between RMS and HRV. Moderate-to-strong correlations were found between PImax and spectral HRV index and between PEmax and spectral HRV index during the RSA-M (P<0.05).
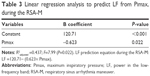
Strong correlations were also observed between HRV complexity indices (ApEn and SampEn) and PEmax during the RSA-M, as shown in Figure 2. A simple linear regression model was applied and the results are listed in Table 3. We found that, during the RSA-M, isolated PImax explained 44% of LFnu behavior.
Discussion
The primary finding of this study was that patients affected with COPD presented increased parasympathetic activity at rest in the sitting position when compared to the RSA-M. However, during the RSA-M, COPD patients presented enhanced sympathetic response and reduced parasympathetic tone, with an HRV complexity reduction. Finally, moderate-to-strong correlations were observed between RMS and spectral HRV index and between RMS and nonlinear HRV index. Our findings are relevant to understand COPD effects on HR autonomic modulation and their relationship with impaired RMS.
In this study, we observed marked parasympathetic modulation in COPD patients at rest. This is in line with literature findings and has been previously explained by the FEV1 reduction and the bronchoconstriction increase, which are characteristic in these patients.19 However, the RSA-M induces a stimulation of the ANS,15 as it is a maneuver able to elicit a parasympathetic response. We observed that patients presented a response contrary to what was expected during the parasympathetic accentuation maneuver. Our results are in line with those by Reis et al,18 who observed increased sympathetic activation and reduced parasympathetic response. Controlled breathing could possibly accentuate pulmonary hyperinflation, which is already present in these patients as a result of chronic airways obstruction.10,18
Novel results were obtained in this study regarding the ANS complexity, assessed through HRV nonlinear indices SampEn and ApEn; complexity was found to be reduced during the RSA-M when compared to resting conditions. Literature results show that COPD patients present reduced ANS complexity when compared with healthy subjects.20 In this line of evidence, Mazzuco et al9 observed that the RSA-M, when compared with other autonomic tests that predominantly stimulate the sympathetic drive, was able to better evidence the impairments caused by the disease. This can be explained by the fact that parasympathetic modulation is more impaired in these patients due to air trapping and gas-exchange disturbances.9
Moderate-to-strong correlations were observed in this study between RMS (PImax and PEmax) and spectral and nonlinear HRV indices; moreover, isolated PImax was found to be able to explain 44% of LF power behavior. Respiratory muscle weakness influences the phrenic dynamics and the expired air volume, with a functional residual capacity increase. Thus, it could be responsible for the alteration of the cardiac autonomic control response.12 Therefore, we can assume that impaired RMS can substantially influence the RSA-M effect and the HRV behavior and that inspiratory muscle weakness can determine greater vagal attenuation in COPD patients. It is known that respiratory muscle weakness leads to fast and shallow breathing and that diaphragmatic incursion is limited by pulmonary hyperinflation. Thus, the ergoreceptor may be activated early and may be responsible for the fast central response in cardiac autonomic control.12 A similar result was obtained between respiratory muscle weakness and reduced HRV in chronic heart failure patients.11 Based on the result of this study, we propose an equation for LF prediction during the RSA-M: LF during the RSA-M =120.71– (0.623× PImax).
This study does possess limitations that deserve to be mentioned. Because of rigid exclusion criteria and the selection of patients with more than 95% of sinus beats, our sample is not fully representative of the entire COPD population, which is known to include patients with arrhythmias that compromise data recording and analysis. Moreover, only patients with GOLD stage II or higher COPD stage were included in the study; however, patients in the early stages of the disease could have a lower impact of the disease on cardiac autonomic control. In this study, we evaluated a relatively small cohort of COPD patients. Interestingly, most of the previous studies enrolled similar numbers of patients,5,9–12 whereas few studies analyzed larger cohorts of patients.18–20 Another limitation of this work consists of the fact that underlying inflammation was not evaluated and that sarcopenia was not quantified. Such analyses could contribute to a better understanding of the mechanisms involved in mechanoneurological control, such as flow and blood oxygenation reduction, both in the brain and in the peripheral muscles.21 Therefore, studies with greater, heterogeneous samples, including more comprehensive investigations, are needed.
This study bears great significance and importance for the clinical management of COPD patients. The novel results hereby presented about RMS in COPD patients might lead to an effective improvement in pulmonary rehabilitation in a clinical setting. Respiratory muscle training, potential clinical routine use of controlled breathing pattern in COPD patients during pulmonary rehabilitation, and any adverse effects on cardiopulmonary dynamics need further investigation in future studies.
Conclusion
In conclusion, patients affected by COPD presented increased parasympathetic activity and ANS complexity at rest in the sitting position when compared to the RSA-M. This suggests an autonomic modulation alteration in basal conditions. During the RSA-M, a marked sympathetic modulation and a reduced parasympathetic response, with an HRV complexity reduction, were induced. Finally, RMS was found to be strongly associated with the sympathovagal response in COPD patients. These findings are relevant to understanding of COPD effects on HR autonomic modulation, and this is important to elucidate pathobiological mechanisms linking COPD to its comorbidities.
Acknowledgments
This study was funded by the University of Santa Cruz do Sul – UNISC, Santa Cruz Hospital and DECIT/SCTIE-MS/FAPERGS/CNPq 1264-2551/13-1. FAPESP (n 2013/23013-0).
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Pocket Guide to COPD Diagnosis, Management and Prevention. Global Initiative for Chronic Obstructive Lung Disease; 2015. Available from: http://www.goldcopd.it/materiale/2015/GOLD_Pocket_2015.pdf. Accessed October 27, 2015. | ||
Dal Negro RW, Bonadiman L, Turco P. Prevalence of different comorbidities in COPD patients by gender and GOLD stage. Multidiscip Respir Med. 2015;10(1):24. | ||
Divo M, Cote C, Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. | ||
Roque AL, Valenti VE, Massetti T, et al. Chronic obstructive pulmonary disease and heart rate variability: a literature update. Int Arch of Med. 2014;7:43. | ||
Nicolino J, Ramos D, Leite MR, et al. Analysis of autonomic modulation after an acute session of resistance exercise at different intensities in chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis. 2015;10:223–229. | ||
Caruso FCR, Reis MS, Siqueira ACB, Gardim M, Catai AM, Borghi-Silva A. Determining anaerobic threshold through heart rate variability in patients with COPD during cycloergometer exercise. Fisioter Mov. 2012;25(4):717–725. | ||
Paschoal MA, Petrelluzzi KFS, Gonçalves NVO. Study of heart rate varability in patients with chronic obstructive pulmonary disease. Rev Ciênc Méd. 2002;11(1):27–37. | ||
Abreu LC. Heart rate variability as a functional marker of development. J Hum Growth Dev. 2012;22(3):279–282. | ||
Mazzuco A, Medeiros WM, Sperling MPR, et al. Relationship between linear and nonlinear dynamics of heart rate and impairment of lung function in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:1651–1661. | ||
Pantoni CBF, Reis MS, Martins LEB, Catai AM, Costa D, Borghi-Silva A. Study on autonomic heart rate modulation at rest among elderly patients with chronic obstructive pulmonary disease. Rev Bras Fisioter. 2007;11(1):35–41. | ||
Reis MS, Arena R, Archiza B, Toledo CF, Catai AM, Borghi-Silva A. Deep breathing heart rate variability is associated with inspiratory muscle weakness in chronic heart failure. Physiother Res Int. 2014;19(1):16–24. | ||
Reis MS, Arena R, Deus AP, Simões RP, Catai AM, Borghi-Silva A. Deep breathing heart rate variability is associated with respiratory muscle weakness in patients with chronic obstructive pulmonary disease. Clinics. 2010;65(4):369–375. | ||
Reis MS, Sampaio LM, Lacerda D, et al. Acute effects of different levels of continuous positive airway pressure on cardiac autonomic modulation in chronic heart failure and chronic obstructive pulmonar disease. Arch Med Sci. 2010;6(5):719–727. | ||
Gibson GJ, Whitelaw W, Siafakas N. Tests of overall respiratory function. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):521–526. | ||
Pereira CAC, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007;33(4):397–406. | ||
Neder JA, Andreoni S, Castelo-Filho A, Nery LE. Reference values for lung function tests. I. Static volumes. Braz J Med Biol Res. 1999;32:703–717. | ||
Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Task Force of European Society of Cardiology and the North American Society of Pacing Electrophysiology. Eur Heart J. 1996;17:354–381. | ||
Reis MS, Ana P, Rodrigo P, Aniceto IAV, Catai AM, Borghi-silva A. Autonomic control of heart rate in patients with chronic cardiorespiratory disease and in healthy participants at rest and during a respiratory sinus arrhythmia maneuver. Rev Bras Fisioter. 2010;14(2):106–113. | ||
Carvalho TD, Pastre CM, Abreu LC De, Marques LC. Fractal correlation property of heart rate variability in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:23–28. | ||
Cheng ST, Wu YK, Yang MC, et al. Pulmonary rehabilitation improves heart rate variability at peak exercise, exercise capacity and health-related quality of life in chronic obstructive pulmonary disease. Heart Lung. 2014;43(3):249–255. | ||
Oliveira MF, Zelt JT, Jones JH, et al. Does impaired O2 delivery during exercise accentuate central and peripheral fatigue in patients with coexistent COPD-CHF? Front Physiol. 2015;5:514. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.