Back to Journals » Patient Preference and Adherence » Volume 12
Relationship between beliefs about medicines, adherence to treatment, and disease activity in patients with rheumatoid arthritis under subcutaneous anti-TNFα therapy
Authors Horne R, Albert A, Boone C
Received 24 February 2018
Accepted for publication 2 May 2018
Published 22 June 2018 Volume 2018:12 Pages 1099—1111
DOI https://doi.org/10.2147/PPA.S166451
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Rob Horne,1 Adelin Albert,2 Caroline Boone3
1University College London School of Pharmacy, London, UK; 2Biostatistics, University Hospital of Liége, Liége, Belgium; 3Medical Department, Pfizer SA/NV, Brussels, Belgium
Objective: In patients with rheumatoid arthritis (RA), nonadherence to treatment is often related to patients’ beliefs and concerns regarding their medication. This study aimed to analyze the correlations regarding patients’ medication beliefs, medication adherence, and objective measures of disease activity and safety in patients with RA established on subcutaneous (SC) anti-tumor necrosis factor α (TNFα) therapy.
Methods: This Phase IV, noninterventional, non-drug-specific study enrolled patients with RA being treated with stable-dose SC anti-TNFα (adalimumab, etanercept, golimumab, and certolizumab pegol). At initial visit and 6 and 12 months later, patients completed the Beliefs about Medicines Questionnaire-Specific section, assessing perceptions of personal need for anti-TNFα therapy (anti-TNFα-Necessity) and concerns (anti-TNFα-Concerns), Medication Adherence Rating Scale (MARS), mean Disease Activity Score in 28 joints (DAS28), and other scales. Longitudinal data were analyzed by linear mixed models.
Results: A total of 460 patients were included. At initial visit, anti-TNFα-Necessity beliefs were high (mean ± SD: 4.3 ± 0.55) vs anti-TNFα-Concerns (2.8 ± 0.78). Medication adherence (MARS) was high (4.8 ± 0.39). All scores remained stable over the 1-year follow-up period. Anti-TNFα-Necessity beliefs and anti-TNFα-Concerns were not related to each other, but strongly correlated with medication adherence. While concerns worsened with disease activity, clinical status, and low quality of life, necessity beliefs remained unaffected.
Conclusion: In patients with RA established on stable-dose SC anti-TNFα, anti-TNFα-Necessity beliefs persistently outweighed anti-TNFα-Concerns, but both correlated with adherence. These findings may be of use in subsequent studies looking to predict adherence in patients starting treatment with SC anti-TNFα.
Keywords: arthritis, rheumatoid, biological therapy, tumor necrosis factor-alpha, medication adherence
Plain-language summary
Rheumatoid arthritis (RA) is a chronic, long-term condition that causes pain, swelling, and stiffness in the joints. Tumor necrosis factor α (TNFα) is one of the components of the immune system that causes joint inflammation in RA. A class of biological disease-modifying antirheumatic drugs binding to TNFα prevent it from causing the symptoms of RA. However, these drugs can have side effects. Worries about side effects are one of the reasons patients stop taking their medication. This study was designed to investigate the beliefs patients have about their RA medication over a year of taking it. At the beginning of the year, after 6 months, and at the end of the year, patients were asked questions about the necessity of taking their medication, their concerns about their medication, and how closely they adhered to their medication schedule. Patients’ beliefs in the necessity of taking their medication outweighed their concerns regarding their medication throughout the year. While concerns grew as patients’ disease and quality of life worsened, beliefs regarding the necessity of the treatment remained unaffected. Patients with a strong belief in the necessity of their medication and low concerns regarding their medication had higher treatment adherence.
Introduction
Rheumatoid arthritis (RA) is a chronic multisystem disease with a global estimated prevalence of 0.35% in women and 0.13% in men.1 Disease-modifying antirheumatic drugs (DMARDs) are important for the successful treatment of RA and can be classified into biological and nonbiological agents. Nonbiological DMARDs are widely used as first-line treatments for RA.2 Current clinical practice guidelines recommend that clinicians start biological DMARDs if patients have suboptimal responses or are intolerant to one or two nonbiological DMARDs.2 TNFα inhibitors are the largest group of biological DMARDs available to treat RA, and include adalimumab, etanercept, infliximab, golimumab, and certolizumab pegol.3,4 Clinical trials of these medications consistently show excellent and comparable efficacy in improving clinical, functional, and radiological disease outcomes in patients with RA.5
The ultimate goal of DMARD treatment is to achieve remission.6 With improving treatment strategies and an increasing number of available effective treatments, the proportion of patients reaching sustained remission has grown.5 If complete remission cannot be achieved, the management goals are to control disease activity and maximize the patient’s quality of life.7
In patients with RA who are established on anti-TNFα therapy, optimal patient outcomes depend on continued adherence to treatment. Studies across long-term conditions, including RA, show that adherence to treatment tails off over time.8,9 It is estimated that in developed countries, adherence to long-term therapy for chronic illnesses averages 50%.8 Nonadherence is often related to patients’ beliefs regarding their medication, doubts about continued need, and concerns, even when patients are doing well on treatment.10 A recent meta-analysis of 94 peer-reviewed studies spanning 18 countries and involving over 25,000 patients across 24 long-term conditions, including RA, consistently showed that nonadherence was related to doubts about medication necessity and concerns about potential adverse effects.11 Investigating beliefs about medication is especially important in RA, as it is a chronic disease, and patients are often advised to take potentially toxic drugs, including anti-TNFα.12 Being able to identify patients with RA who are at risk of medication nonadherence could assist in the design and appropriately timed delivery of interventions to support optimal adherence, thus improving patients’ health.12
There is a relative lack of information regarding the beliefs about anti-TNFα medication held by patients with RA who are established on anti-TNFα therapy. Only one cohort study has evaluated the beliefs about anti-TNFα medicines in patients with RA, and that study was restricted to patients receiving adalimumab.13
The aim of this study was to assess patients’ beliefs about the necessity of and concerns regarding subcutaneous (SC) anti-TNFα therapy, and to analyze the correlations regarding medication beliefs and self-reported adherence to medication, objective measures of RA disease activity, and safety profiles over a 12-month follow-up period – in particular the correlation between belief in the necessity of treatment and the Disease Activity Score in 28 joints (DAS28), which was the study primary objective. It also purposed to identify factors influencing patients’ beliefs and concerns regarding SC anti-TNFα therapy.
Methods
Study design
This was a 4-year, open-label, multicenter, Phase IV, noninterventional, non−drug-specific study conducted in patients with RA who were being treated with stable-dose SC anti-TNFα (adalimumab, etanercept, golimumab, and certolizumab pegol) prior to enrollment. Patients were recruited from 34 treatment centers in Belgium. The study was initiated on October 1, 2010, and the last patient was enrolled on December 30, 2013. The last follow-up visit took place on January 14, 2015. This study was conducted in compliance with the ethical principles originating in or derived from the Declaration of Helsinki, and the protocol adhered to the International Conference on Harmonisation Guidelines for Good Clinical Practice. Patients provided written informed consent before participating in the study. The protocol and informed consent documents were reviewed and approved by the institutional review board/independent ethics committee of the main institution (approving board AZ St Jan Brugge Oostende AV Ethics Committee, site number OG 065/049, date of approval August 6, 2010) and all other study centers before patient enrollment. This study was registered on ClinicalTrials.gov (NCT01432366). Each participating study center is listed in Table S1.
At the initial study visit, patient demographics, duration of disease and treatment, and details of current medication and comorbidities were recorded, with several questionnaires and scales completed. Patients were assessed 6 and 12 months after the initial visit; the same questionnaires were completed and details of current medication and anti-TNFα and DMARD-related adverse events (AEs) were recorded at these follow-up visits. The primary objective of the study was to estimate the correlation between patient beliefs about the necessity of SC anti-TNFα and DAS after a 1-year follow-up.
The Beliefs about Medicines Questionnaire (BMQ) – Specific (BMQ-S11, © R Horne) comprises two scales: Specific-Necessity and Specific-Concerns.14 The two scales together include eleven statements (five Necessity, six Concerns). Details regarding these can be found in the Supplementary material. Patients indicated their level of agreement with each statement on a 5-point Likert scale where 1 = strongly disagree and 5 = strongly agree. Both BMQ Necessity and Concerns scores were scaled to range from 1 to 5, with higher scores indicating stronger beliefs regarding medicine. The BMQ-Specific Necessity scale was used to assess patients’ beliefs about their personal need for anti-TNFα therapy, with higher scores indicating stronger beliefs in medication necessity. The BMQ-Specific Concerns scale assessed patients’ concerns about the potential adverse effects of using anti-TNFα, based on beliefs about the potential for harm now and in the future, and other concerns, such as being dependent on medicines. A Necessity-Concerns differential (NCD) was calculated as a numerical indicator of how each individual judged their personal need for anti-TNFα treatment relative to their concerns about taking it (range −4 to 4). Patients with missing BMQ items were excluded from all BMQ-score calculations.
The Medication Adherence Rating Scale (MARS) is a 5-item scale in which the patient himself/herself assesses how often he/she engages in nonadherent behavior. Each item is rated on a 5-point Likert scale where 1 = always and 5 = never. The total score is scaled to range from 1 to 5, with higher scores indicating higher levels of self-reported adherence.15 Details regarding the items of the MARS can be found in the Supplementary material.
Other instruments used to document patients’ health included the DAS28 (either erythrocyte-sedimentation rate or C-reactive protein could be used to calculate the DAS28 score, and the mean score was used if both were available for an individual patient),16 DAS28 remission (score <2.6), Health Assessment Questionnaire (HAQ),17 pain visual analog scale (VAS),18 fatigue VAS,19 European Quality of Life-5 Dimensions (EQ5D),20 physician and patient satisfaction regarding medication using a 0–100 VAS where 0 = absolutely not satisfied and 100 = extremely satisfied, and the Patient Health Questionnaire (PHQ-9) depression questionnaire (DQ).21 Safety was categorized and scored as 1 = absence of AEs, 2 = presence of nonserious AEs only, and 3 = presence of one or more serious AEs for each patient.
Patients
Patients were eligible to participate in this study if they were ≥18 years of age with a diagnosis of active RA. Patients had to be receiving stable SC anti-TNFα therapy for ≥1 consecutive year, to ensure that treatment was well established and disease activity well managed. SC anti-TNFα therapies were administered at the recommended labeled dose (etanercept 50 mg/week once or 25 mg/week twice, adalimumab 40 mg/once every other week, golimumab 50 mg once a month, and certolizumab pegol at 200 mg/once every other week). Any other therapies for RA also had to be taken at stable doses for defined periods (DMARDs, including methotrexate, for ≥12 weeks before the initial visit; oral corticosteroids for ≥4 weeks before the initial visit and maximum dose 10 mg/day; intravenous or intra-articular corticosteroids for ≥4 weeks before the initial visit). Patients had to provide written informed consent and be capable of understanding and completing the study questionnaires. Patients were excluded from the study if they had a current or former psychiatric illness that would interfere with their ability to comply with protocol requirements or give informed consent, or if they were participating in other clinical or observational trials.
Statistical analyses
Results are expressed as mean ± SD for quantitative data, median and interquartile range (IQR) for lifetime data, and frequency tables for categorical findings. Correlation coefficients were used to measure association between two quantitative variables. Mean values were compared by one-way analysis of variance, while for proportions the χ2 test was used. The time evolution of each study variable was analyzed by a generalized linear mixed-effect model in which patients were considered as random and time the only fixed covariate. The same method was used to test the relationship between BMQ scores (Necessity and Concerns) and each variable separately (adherence and clinical parameters) over the 12 months by accounting for repeated data within patients. Results were expressed as regression coefficients with associated standard error (SE). Calculations were always done on the maximum number of data available. Results were considered significant at the 5% critical level (P<0.05). Data analysis was carried out using SAS version 9.4 for Windows and R version 3.2.2.
Results
Patient disposition
A total of 477 patients were screened for this study, and 17 were found to be ineligible to participate (Figure 1). Of the 460 patients included, 427 (92.8%) had one or more follow-up visits and 392 (91.8%) completed all study visits.
  | Figure 1 Patient disposition. |
Demographics and patient history
Demographic and clinical characteristics of the study population are shown in Table 1. Among the 460 patients, there was a majority of women (73.0%) and the average age was 59.3 years. A total of 437 patients had previously been taking one or more DMARDs, with over half (58.6%) taking two. Most patients (84.3%) were taking one SC anti-TNFα medication and had not previously taken any other biological treatments for RA (89.7%).
Patients’ initial beliefs, adherence, clinical status, and safety
Patients’ beliefs about medicines (anti-TNFα-Necessity and anti-TNFα-Concerns), self-reported adherence, clinical status, and safety parameters were assessed throughout the study (Table 2). At the initial visit, the average NCD was positive (1.46), although 26 of 408 (6.4%) patients had a negative NCD. The average MARS total score was 4.76, and less than 1% of patients scored at or below the MARS midpoint, indicating high levels of self-reported adherence to treatment. Figure 2 provides a profile of the beliefs held about RA medication and reasons for nonadherence in this patient population.
Table 3 shows patients’ responses to the individual BMQ items at the initial visit. Less than 2% of patients scored at or below the anti-TNFα-Necessity scale midpoint (≤3 on a scale of 1–5), indicating a high level of belief in the need for their RA medication. The percentage of patients scoring below the scale midpoint (totally disagree/disagree) for the anti-TNFα-Necessity items (“N” in Table 3) ranged from 0.9% (My health at present depends on my medicines) to 3.5% (My medications protect me from becoming worse). Almost half (48%) of the patients, however, scored at or above the anti-TNFα-Concerns scale midpoint, indicating increased concerns about their RA medication. The percentage of patients scoring above the scale midpoint (agree/totally agree) for the anti-TNFα-Concerns items (“C” in Table 3) ranged from 15.7% (My medications disrupt my life) to 61.8% (I sometimes worry about the long-term effects of my medications). At the initial visit, no correlation was seen between anti-TNFα-Necessity and anti-TNFα-Concerns scores (r=−0.056, P=0.26). Anti-TNFα-Necessity scores were correlated with MARS, patient-satisfaction, and safety scores, while anti-TNFα-Concerns scores were correlated with all clinical and quality-of-life parameters, but not with safety scores (Table S2).
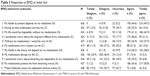  | Table 3 Responses to BMQ at initial visit |
Evolution of patients’ beliefs and clinical parameters over 12 months
After the initial visit (Table 2, Figure S1), mean anti-TNFα-Necessity, anti-TNFα-Concerns, MARS, and DAS28 scores remained stable during the entire 1-year follow-up. In particular, the NCD was maintained at a positive mean level of about 1.44 points and generalized linear mixed-effect model analysis showed no time effect. The number of patients with a negative NCD did not change over the course of the year. This was also the case for the other instrument scores, except safety, where a small increase in incidence of AEs was noted at 6 months (P=0.012). Remission patterns were also fairly stable, with the status of almost two-thirds of patients not changing over the 12 months: 126 (41.2%) patients were constantly in remission and 66 (21.6%) were never in remission.
Given the stable evolution pattern, the relationship between BMQ scales (dependent variable) and each individual parameter (covariate) was assessed by linear mixed-effects models accounting for repeated values over 12 months (Table 4). Results shown in Table 4 confirmed the lack of correlation between anti-TNFα-Necessity and anti-TNFα-Concerns (P=0.062) observed at initial visit, the strong positive associations of adherence and patient satisfaction with anti-TNFα-Necessity, and the negative associations with anti-TNFα-Concerns (all P<0.0001). Neither anti-TNFα-Necessity nor anti-TNFα-Concerns were related to safety. More importantly, while anti-TNFα-Concerns was found to be significantly correlated with disease activity (DAS28), clinical status (HAQ, pain and fatigue VAS, PHQ-9-DQ), and quality of life (EQ5D), no association was found between anti-TNFα-Necessity beliefs and these parameters. Specifically, the study’s primary objective of estimating correlation between anti-TNFα-Necessity and the DAS28 showed that there was none after a 1-year follow-up.
Discussion
This study of beliefs about SC anti-TNFα treatment (adalimumab, etanercept, golimumab, and certolizumab pegol) in patients with persistent RA is the first to investigate the relationship between these beliefs and disease activity and self-reported treatment adherence. In this study of patients with stable and generally well-managed disease, most had positive views about anti-TNFα treatment and agreed that anti-TNFα medication was necessary to maintain health now and in the future. However, some harbored concerns about the potential adverse effects of treatment. More than a fifth (22.4%) of patients agreed that their anti-TNFα medication caused unpleasant side effects, and 61.8% were concerned about long-term effects, but concerns went beyond the experience of side effects; patients also reported worrying about having to take medication (46.0%) and becoming too dependent on their medication (36.3%). However, patients generally considered their RA medication necessary (ie, average scores were greater than the scale midpoint) and tended to disagree that potential adverse consequences of taking their medication were a cause for concern. The NCD was consistently positive, indicating that patients generally rated their need to take SC anti-TNFα more highly than their concerns about the potential disadvantages. The positive association between anti-TNFα-Necessity and time since RA symptoms and diagnosis suggests that patients with longer duration of disease were more likely to consider their medication necessary for controlling their RA. The significantly lower anti-TNFα-Concerns scores for patients in remission suggest that patients with lower disease burdens were less concerned about the potential side effects of their medication. The average BMQ scores (Necessity and Concerns) in this study were similar to those reported in the only other study of beliefs about SC anti-TNFα treatment published to date.13 Studies of other RA medications have also reported similar BMQ Necessity12,22,23 and Concerns12,22–24 scores, although one had lower Necessity scores than have been reported here and elsewhere.24
The patients in the present study had mostly high self-reported adherence to treatment, which was strongly correlated with a belief in the necessity of treatment. Concerns regarding AEs correlated with poor clinical status and were inversely correlated with adherence. A previous study of adalimumab in the treatment of RA has also found that patient beliefs impacted treatment adherence; the importance of medication necessity for adalimumab users (regardless of the level of concern) predicted increased adherence.13 However, that study focused on patients who were beginning biological DMARD treatment with adalimumab as their first anti-TNFα medication, while the study reported here involved persistent patients. This suggests that belief in the importance of the medication could be indicative of high levels of adherence, regardless of how long the patient has been receiving anti-TNFα medication; however, a study with a direct comparison between groups (patients who recently started receiving anti-TNFα vs those established on this medication) would be required to confirm this. Studies of nonbiological therapies for RA,22,24,25 as well as studies involving patients with other chronic conditions,10,11,26–30 have also shown the important effect of patient beliefs on medication adherence.
In the study reported here, significant (P<0.05) correlations were seen regarding Necessity and Concerns scores and several other variables. Some of these correlations are similar to those seen in a previous study of beliefs about medications in patients with RA.12 Neame and Hammond12 reported significant correlations between Necessity scores and disease duration (as seen in our study), but they also found significant correlations between Necessity scores and Pain VAS, Fatigue VAS, and HAQ, which our study did not. Differences between these results could reflect the different treatments being assessed (SC anti-TNFα in this study vs DMARDs in the earlier study) and the different study populations (patients in our study were selected on the basis of receiving stable treatment, while no such selection was applied in the other study).
This study followed a cohort of persistent patients with RA, who were recruited after they had been receiving anti-TNFα treatment for a median of 5 years. The data did not vary significantly over the 12-month study period and can thus be viewed as a profile of the clinical and psychological characteristics of persistent and stable patients with RA. It would be useful to see if the belief profile observed in this persistent and adherent population (anti-TNFα-Necessity outweighing anti-TNFα-Concerns) can help predict which patients starting treatment are likely to become nonpersistent (discontinue treatment before 12 months) or have lower self-reported treatment adherence. Beliefs about medicines in patients with RA have previously been shown to predict side effects over 6 months.31 More detailed studies of patients’ beliefs in other long-term conditions32–34 have found that doubts about treatment necessity are often linked to logical but potentially misplaced beliefs about the illness (eg, perceiving that regular treatment is less important in the absence of symptoms). Likewise, concerns about specific medicines are often linked to mistrust of pharmaceuticals as a class of treatment. Addressing these beliefs in negotiated approaches to treatment (where the patient is involved in making treatment decisions) can support informed treatment choices and help ensure that nonadherence does not result from misplaced beliefs.35,36 If (as we expect) treatment necessity beliefs and concerns are shown to influence persistence and long-term adherence, then adherence-support programs could take account of these beliefs, as recommended by the National Institute for Health and Care Excellence.37
This study did have some limitations. Given that patients were on stable SC anti-TNFα for ≥1 year at the initial study visit and had a median treatment duration of 5 years before enrollment, the study population could be biased toward positive beliefs regarding their study medication. Also, a stable study population means that it is not possible to test whether beliefs about medicines can predict treatment outcome (such as remission, discontinuing therapy, or the occurrence of AEs), and there was no cohort of patients starting anti-TNFα therapy included to allow such predictions to be made. Another limitation is that accurately measuring self-reported adherence to medication is difficult and self-reported measures tend to overestimate adherence compared with other assessment approaches.38 This study utilized a patient-reported measure of adherence that is open to some interpretation. As the anti-TNFα therapies covered in this study are self-injectable and the study protocol did not include other measures of adherence, such as the collection of used self-injection devices, there was no way of independently verifying levels of medication adherence.
Conclusion
This study found that beliefs about medicines strongly correlated with medication adherence. Beliefs about medicines and medication adherence did not change over the 12-month follow-up period, giving a clinical and psychological profile of a persistent, stable RA population being treated with SC anti-TNFα. These findings may be of use in subsequent studies looking to predict adherence in patients starting treatment with SC anti-TNFα.
Acknowledgments
This study was funded by Pfizer. Medical writing support for this manuscript was provided by Lorna Forse, PhD, and Samantha Forster, PhD, of Engage Scientific Solutions and was funded by Pfizer.
Disclosure
RH was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North Thames at Bart’s Health NHS Trust. He has undertaken speaker engagements with honoraria with AbbVie, Amgen, Biogen Idec, Gilead Sciences, GlaxoSmithKline, Janssen, Pfizer, Roche, Shire Pharmaceuticals, MSD, Astellas, AstraZeneca, DRSU, Erasmus, and Novartis. He is founder and shareholder of an UCL-business spin-out company (Spoonful of Sugar), providing consultancy on medication-related behavior to health care policy makers, providers, and industry. AA is professor emeritus of biostatistics and adviser at the University Hospital of Liège and was funded by Pfizer for the statistical analysis of this study. CB was employed by Pfizer at the time of the study and owns stock in Pfizer. The authors report no other conflicts of interest in this work.
References
Cross M, Smith E, Hoy D, et al. The global burden of rheumatoid arthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1316–1322. | ||
Kumar P, Banik S. Pharmacotherapy options in rheumatoid arthritis. Clin Med Insights Arthritis Musculoskelet Disord. 2013;6:35–43. | ||
Scott DL. Biologics-based therapy for the treatment of rheumatoid arthritis. Clin Pharmacol Ther. 2012;91(1):30–43. | ||
Gibofsky A. Comparative effectiveness of current treatments for rheumatoid arthritis. Am J Manag Care. 2012;18(13 Suppl):S303–S314. | ||
Radner H, Aletaha D. Anti-TNF in rheumatoid arthritis: an overview. Wien Med Wochenschr. 2015;165(1–2):3–9. | ||
Combe B, Landewe R, Lukas C, et al. EULAR recommendations for the management of early arthritis: report of a task force of the European Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2007;66(1):34–45. | ||
American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002;46(2):328–346. | ||
World Heath Organization. Adherence to Long-Term Therapies: Evidence for Action. Geneva: WHO; 2003. Available from: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Accessed July 21, 2017. | ||
Joplin S, van der Zwan R, Joshua F, Wong PK. Medication adherence in patients with rheumatoid arthritis: the effect of patient education, health literacy, and musculoskeletal ultrasound. Biomed Res Int. 2015;2015:150658. | ||
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness: processes and applications. J Psychosom Res. 1999;47(6):555–567. | ||
Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS One. 2013;8(12):e80633. | ||
Neame R, Hammond A. Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatology. 2005;44(6):762–767. | ||
Morgan C, McBeth J, Cordingley L, et al. The influence of behavioural and psychological factors on medication adherence over time in rheumatoid arthritis patients: a study in the biologics era. Rheumatology (Oxford). 2015;54(10):1780–1791. | ||
Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. | ||
Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–247. | ||
Prevoo ML, van ‘t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38(1):44–48. | ||
Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–145. | ||
Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. New York: Guilford Press; 1992:134–151. | ||
Shahid A, Wilkinson K, Marcu S, Shapiro CM. Visual analogue scale to evaluate fatigue severity (VAS-F). In: Shahid A, Wilkinson K, Marcu S, Shapiro C, editors. STOP, THAT, and One Hundred Other Sleep Scales. Heidelberg: Springer; 2011:399–402. | ||
EuroQol Group. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. | ||
Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J Gen Intern Med. 2001;16(9):606–613. | ||
Treharne GJ, Lyons AC, Kitas GD. Medication adherence in rheumatoid arthritis: effects of psychosocial factors. Psychol Health Med. 2004;9(3):337–349. | ||
van den Bemt BJ, van den Hoogen FH, Benraad B, Hekster YA, van Riel PL, van Lankveld W. Adherence rates and associations with nonadherence in patients with rheumatoid arthritis using disease modifying antirheumatic drugs. J Rheumatol. 2009;36(10):2164–2170. | ||
de Thurah A, Nørgaard M, Harder I, Stengaard-Pedersen K. Compliance with methotrexate treatment in patients with rheumatoid arthritis: influence of patients’ beliefs about the medicine. A prospective cohort study. Rheumatol Int. 2010;30(11):1441–1448. | ||
Hope HF, Bluett J, Barton A, Hyrich KL, Cordingley L, Verstappen SM. Psychological factors predict adherence to methotrexate in rheumatoid arthritis; findings from a systematic review of rates, predictors and associations with patient-reported and clinical outcomes. RMD Open. 2016;2(1):e000171. | ||
Nicklas LB, Dunbar M, Wild M. Adherence to pharmacological treatment of non-malignant chronic pain: the role of illness perceptions and medication beliefs. Psychol Health. 2010;25(5):601–615. | ||
Phatak HM, Thomas J. Relationships between beliefs about medications and nonadherence to prescribed chronic medications. Ann Pharmacother. 2006;40(10):1737–1742. | ||
Gonzalez JS, Penedo FJ, Llabre MM, et al. Physical symptoms, beliefs about medications, negative mood, and long-term HIV medication adherence. Ann Behav Med. 2007;34(1):46–55. | ||
Horne R, Cooper V, Gellaitry G, Date HL, Fisher M. Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence: the utility of the necessity-concerns framework. J Acquir Immune Defic Syndr. 2007;45(3):334–341. | ||
Jamous RM, Sweileh WM, El-Deen Abu Taha AS, Zyoud SH. Beliefs about medicines and self-reported adherence among patients with chronic illness: a study in Palestine. J Family Med Prim Care. 2014;3(3):224–229. | ||
Nestoriuc Y, Orav EJ, Liang MH, Horne R, Barsky AJ. Prediction of nonspecific side effects in rheumatoid arthritis patients by beliefs about medicines. Arthritis Care Res (Hoboken). 2010;62(6):791–799. | ||
Chapman SC, Horne R, Eade R, Balestrini S, Rush J, Sisodiya SM. Applying a perceptions and practicalities approach to understanding nonadherence to antiepileptic drugs. Epilepsia. 2015;56(9):1398–1407. | ||
Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health. 2002;17(1):17–32. | ||
Horne R, Parham R, Driscoll R, Robinson A. Patients’ attitudes to medicines and adherence to maintenance treatment in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(6):837–844. | ||
Clifford S, Barber N, Elliott R, Hartley E, Horne R. Patient-centred advice is effective in improving adherence to medicines. Pharm World Sci. 2006;28(3):165–170. | ||
Petrie KJ, Perry K, Broadbent E, Weinman J. A text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol. 2012;17(1):74–84. | ||
National Institute for Health and Care Excellence. Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence. London: NICE; 2009. Clinical guideline [CG76]. Available from: https://http://www.nice.org.uk/Guidance/CG76. Accessed July 21, 2017. | ||
Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470–482. |
Supplementary materials
Beliefs about Medicines Questionnaire items: BMQ-Specific
The BMQ-Specific consists of two scales assessing the patient’s beliefs about the Necessity (N) of the currently prescribed medications for controlling the disease (BMQ-Necessity) and his/her Concerns (C) about potential adverse consequences of taking them (BMQ-Concerns).
The items are:
- My health at present depends on my medicines (N)
- Having to take medications worries me (C)
- My life would be impossible without my medications (N)
- I sometimes worry about the long-term effects of my medications (C)
- Without my medications I would be very ill (N)
- My medications are a mystery to me (C)
- My health in the future will depend on my medications (N)
- My medications disrupt my life (C)
- I sometimes worry about becoming too dependent on my medications (C)
- My medications protect me from becoming worse (N)
- These medicines cause me unpleasant adverse events (C).
Respondents indicate their degree of agreement with each statement on a 5-point Likert scale, ranging from 1 = strongly disagree to 5 = strongly agree. Scores obtained for individual items within both scales are summed and divided by the total number of items in the scale to give a scale score of 1–5. Higher scores indicate stronger beliefs.
Medication Adherence Report Scale items
This five-item scale asks the patient to rate the frequency with which he/she engages in each of the five aspects of nonadherent behavior:
- Forget to take medications
- Modify doses
- Stop taking medications during a certain period
- Decide to miss a dose
- Take less than what is prescribed.
Each item is rated on a 5-point Likert scale, where 1 = always, 2 = often, 3 = sometimes, 4 = rarely, and 5 = never. Scores for each of the five items are summed and divided by five to give a scale score of 1–5, where higher scores indicate higher levels of reported adherence.
  | Table S1 Participating study centers |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






