Back to Journals » Clinical Ophthalmology » Volume 15
Refractive Error and Visual Impairment Among School Children: Result of a South-Eastern Nigerian Regional Survey
Authors Maduka-Okafor FC, Okoye O, Ezegwui I, Oguego NC, Okoye OI, Udeh N, Aghaji AE, Nwobi E , Aneji C, Onwasigwe E, Umeh RE
Received 24 December 2020
Accepted for publication 20 April 2021
Published 4 June 2021 Volume 2021:15 Pages 2345—2353
DOI https://doi.org/10.2147/OPTH.S298929
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Ferdinand C Maduka-Okafor,1 Obiekwe Okoye,1 Ifeoma Ezegwui,1 Ngozi C Oguego,1 Onochie I Okoye,1 Nnenma Udeh,1 Ada E Aghaji,1 Emmanuel Nwobi,2 Chiamaka Aneji,3 Ernest Onwasigwe,1 Rich E Umeh1
1Department of Ophthalmology, College of Medicine, University of Nigeria, Ituku, Enugu, Nigeria; 2Department of Community, College of Medicine, University of Nigeria, Ituku, Enugu, Nigeria; 3Division of Neonatal Perinatal Medicine, McGovern Medical School, University of Texas Health Science Center, Houston, TX, USA
Correspondence: Obiekwe Okoye
Department of Ophthalmology, College of Medicine, University of Nigeria, Ituku, Ozalla, Enugu, Nigeria
Email [email protected]
Purpose: To determine the prevalence refractive errors and causes of visual impairment in school children in the south-eastern region of Nigeria.
Methods: School-based cross-sectional samples of children 5 to 15 of age in both urban and rural areas were profiled through cluster sampling. The main outcome measures were presenting, uncorrected, and best-corrected visual acuity using the Refractive Error in School-age Children (RESC) protocol.
Results: A total of 5723 children were examined during the study period comprising 2686 (46.9%) males and 3037 (53.1%) females; (M:F ratio 0.9:1) and aged 10.49± 2.74SD of mean (range, 5 to 15 years). The age group 12 to < 13 accounted for the highest 776 (13.6%) number of the study participants. The uncorrected visual acuity (VA) of < 20/40 (6/12) was seen in 188 (3.4%) of the study participants while the presenting and best-corrected visual acuity of < 20/40 (6/12) were noted in 182 (3.4%) children and 14 (0.2%) children, respectively. Refractive error was the principal cause of visual impairment.
Conclusion: Prevalence of refractive error is low. Myopia is the principal cause of refractive error occurring more in females and in urban schools. The main cause of visual impairment is refractive error, and most children that need spectacle correction did not have them. Program to identify children with refractive error in addition to providing free or affordable optical services remains the key to preventing visual impairment from refractive error particularly in resource-poor settings.
Keywords: refractive error, school children, prevalence, visual impairment, Nigeria
Introduction
Refractive error occurs when the optical system of the non-accommodating eye fails to bring parallel rays of light to focus on the retina.1 They have been identified as a cause of public health and economic concern.2 This is evidenced by its inclusion in the priority areas of Vision 2020: The Right to Sight, a global initiative spearheaded by a conglomerate of non-governmental organizations and the World Health Organization.3 Globally, refractive error remains one of the primary causes of visual impairment in children.4,5 In children with significant uncorrected refractive errors, there is consistently poorer performance on a range of visio-cognitive and visio-motor tests compared with children without significant refractive errors, with attendant implications for general development and educational performance.6 Reliable data on population-based surveys on prevalence and pattern of distribution of refractive errors are needed to plan cost-effective systematic vision screening programs for reduction of visual impairment and blindness in children. Several investigators7–9 has reported a prevalence of refractive error among school children ranging from 5.2% to 8.9%. Two local surveys,10,11 identified refractive error as the leading cause of visual impairment in school children accounting for 70.7% and 61.1% of cases. Although these studies amongst others provide evidence-based data in understanding the magnitude of refractive error and visual impairment, comparisons across study reports are generally difficult. This is largely due to the different measurement methods and non-uniform definitions used. In 1998, the Refractive Error Study in Children (RESC) protocol was developed to assess the prevalence of visual impairment and refractive error in children of different ethnic origins and cultural settings by using consistent definitions and methods.12 This directly makes it possible to provide comparable data from entirely different parts of the world. From 1998 to 2003, surveys using the RESC protocol were carried out in Nepal,13 China,4 Chile,14 India,15 South Africa,16 and Malaysia.17 These were population-based studies largely among children not attending schools. More recently, it has been found that in communities where there is high school attendance RESC survey protocols carried out in schools give comparable results as population-based surveys.18,19
The main purpose of the Nigeria school eye health guideline20 launched in 2020 is to provide direction for those planning and implementing school eye health programmes within the health and education sector. This guideline is intended for policy makers, educational and health care authorities, health planners, eye care delivery organizations and professionals, including teachers, parents and children. This guideline also takes an integrated approach to school eye health, in which there is an active collaboration between the Federal and State Ministries of Education and Health for joint ownership to ensure effective and efficient delivery of identified initiatives. This document has also noted that only 50% of children needing glasses actually obtained them with cost of procurement being identified as a major contributing factor. Currently in Nigeria, there are no government incentives in form of price subsidy or outright free dispensing of glasses to children as parents pay out of pocket in a background of weak health insurance framework.
To the best of our knowledge, this study represents the only refractive error survey among school children using the RESC protocol in Nigeria. The objective of this study is to generate data using standardized protocol that allows for comparison with that elsewhere and forms the basis for evidence-based policy formulation for efficient resource mobilization and utilization towards a cost-effective, cross-cultural acceptable intervention in reducing the burden of childhood refractive error and visual impairment in Nigeria, and elsewhere in Africa.
This study reports the prevalence of refractive error and visual impairment in school children in Nigeria and compares findings with previous studies in other countries that adopted the RESC protocols.
Methods
The south-eastern region of Nigeria comprises 5 states, namely; Anambra, Enugu, Ebonyi, Abia and Imo state.
The study was a cross-sectional, school-based survey carried out in selected primary and junior secondary schools (public and private) in both urban and rural communities of the 5 states from December 2017 to February 2018. Prior to commencement of study, ethical clearance compliant with the Declaration of Helsinki on research involving human subjects was obtained from the University of Nigeria Teaching Hospital (UNTH)’s Medical and Health Research Ethics Committee (Institutional Review Board). Relevant approvals for the study were also obtained from State Universal Basic Education Board and Post Primary School Management Board. Institutional consent was obtained from the respective school authorities, and informed consent for all the recruited participants was obtained from the parents or guardians.
Sample Size Determination
The primary sampling unit (PSU) was the school (primary or Junior Secondary). There are 6675 primary and Junior Secondary Schools in South East Geopolitical zone, being the study area. Minimum sample size was calculated for the PSU using Version 2 of OpenEpi, applying confidence limits of 5%, confidence level of 95% and a design effect of 1.8 for cluster surveys. The hypothesized % frequency of outcome was 1.4%.
Minimum sample size so calculated is 39 schools (clusters) in the study area. However, this was adjusted upwards to 50 clusters to enable equal distribution of 10 clusters per state. In each cluster, we targeted 2 arms or classes of 30 students each. The minimum expected sample size was 3000 pupils/student. However, we surveyed 5723 pupils for ethical reason of extending the benefit of the survey to more children who would have felt left out if only some of their classmates were recruited.
Sample Selection
The study sample was selected through multistage cluster sampling. In each of the 5 states, the Local Government Areas (LGAs) were stratified into urban and rural. Then from each stratum, one LGA was selected by balloting. In the respective urban and rural LGAs, 1 public primary school and 1 public junior secondary school were selected by balloting. One private primary school and 1private junior secondary school were also selected by balloting. In the respective schools, each grade is subdivided into classes; the classes were the primary sampling unit. In each of the schools, 1 class(arm) per grade was selected by balloting. All children aged 5–15 years in selected classes were approached for recruitment for the survey. If the required number of children was not reached in one class(arm) of the grade level, children in another class but same school or a similar grade level but another school in the same local government area was selected until the required number of children was reached. The overall target was to screen a minimum of 60 pupils in each grade level in each LGA, ie, 720 primary (360 each in the urban and rural LGAs, ie, 6 grade levels so 6×60) and 360 junior secondary (180 each in the urban and rural LGAs, ie, 3 grade levels so 3×60) school pupils in the state. A total of 4 secondary schools and 6 primary schools per state were finally selected and visited. Birth certificates/baptismal/immunization cards and/or school records were used to verify the ages of the enrolled children, when in doubt.
Field Operations
On obtaining the consent from the school authorities, lists of the registered, age-eligible pupils were obtained from the schools and study consent forms were handed over for subsequent distribution to these pupils. Parents were encouraged to call the project team on phone for clarifications or to appear on the scheduled days for the screening visits to meet with the team. Examinations were usually conducted during and after school hours at periods chosen by the school authorities, in such a manner as not to disrupt the daily routine for the concerned pupils. Multiple visits, ranging from 2 to 5 visits, were made to each selected school to achieve the required sample. Children already wearing spectacles were also encouraged to wear them to school. Only those children who presented with signed consent forms. Only those agreeing to the ocular instillation of cycloplegic agents in the eyes of their children were considered as having granted consent. The screening was always preceded on the first day by an eye health education session to the entire school.
Ocular Examination
The clinical examination was conducted by a team usually comprising 3–6 ophthalmologists (consultants and residents in training), 1 experienced optometrist, 2–3 trained visual acuity assistants, 1 trained nurse and 6 additional field workers. A pilot study had been conducted among over 200 school children from Ituku-Ozalla. Standardization of study procedures, training and, re-retraining and validation of all the ophthalmologists were carried out to ensure good agreement in findings. The principal investigator was present at all the sites. The examinations took place in temporary stations in carefully selected appropriate points within the school premises. The examinations were largely according to the RESC protocol for school-based screening.18
Visual acuity was measured uniocularly by the trained personnel at 4metres using retroilluminated logMAR chart with five tumbling E-Optotypes on each line (Precision Vision, La sale, Illinois, USA). The children were directed to indicate the direction of the E optotype by pointing with their hand or by calling out the direction to the hearing of the examiner. The visual acuity was tested with and without spectacles for children who wore their glasses to school.
Corneal light reflex was used to detect the presence of tropias while prism cover test was used to measure the deviation in prism dioptres. The external eye, anterior and posterior segments of the eyes of all the recruited children were then examined, using the pen torchlight, magnifying loupe (x4), direct and indirect (when applicable) ophthalmoscopes (Welch Allyn, Skaneateles, NY). These examinations were carried out by ophthalmologists.
For children with unaided (uncorrected) visual acuity of 20/40 (6/12) or worse in either eye, cycloplegia was induced with 2 drops of 1% cyclopentolate, administered by the nurse 5 minutes apart, with a third drop after 15 minutes. Pupillary dilation of 6mm or more with absence of light reflex was considered complete cycloplegia, on final evaluation after an additional 20–30 minutes. Autorefraction was done by the optometrist using an autorefractor (APPA autorefracto-keratometer AARK-1M 7000). The lens power of the children who wore glasses to school was determined with a focimeter (Manual lensmeterAppasamy KMS-14). For quality assurance, every 10th child had his or her VA and refraction measured again by the principal investigator or any of the senior consultant ophthalmologists on the field. Subjective refraction was performed on all the children with uncorrected VA worse than or equal to 20/40 (6/12) in either eye.
From a checklist of 8 categories of causes, the examining consultant ophthalmologist assigned a principal cause of visual impairment for eyes with uncorrected visual acuity (UCVA) equal to or worse than 20/40 (6/12); with refractive error being routinely assigned as the cause if the acuity improved to better than 20/40 (6/12) with refractive correction. For children with correctible refractive error, free spectacles were prescribed and dispensed. Those needing minor medical attention received such on-site, and those with more serious eye conditions were referred to our base UNTH Ituku-Ozalla. At the end of each examination day, the team also usually attended to other school children and staff members who required eye examination.
Study Definitions
1. Visual Acuity was categorized as follows:19
- normal/near normal vision (20/32 (6/9.5) or better in both eyes),
- unilateral visual impairment (20/32 (6/9.5) or better in one eye only),
- mild impairment in the better eye (≤20/40 (6/12) −20/63 (6/19) in the better eye),
- moderate impairment in the better eye (≤20/80 (6/24)-20/160 (6/48) in the better eye),
- severe visual impairment/blindness (20/200 (6/60) or worse in both eyes).
2. Refractive error was defined as myopia or hypermetropia in either eye. Estimates of refractive error were based on measurement with cycloplegic autorefraction. Eyes with normal or near-normal vision were considered emmetropic. If neither eye was myopic or hyperopic by study definitions, such children were considered emmetropic.
3. Myopia was defined as spherical equivalent (SE) refractive error of at least −0.50D or worse. Children with myopia in one eye or both eyes were regarded as myopic.
4. Hypermetropia was defined as SE of +2.0D or greater. Children with hyperopia in one eye or both eyes were regarded as hyperopic, as long as neither eye was myopic.
5. Astigmatism was investigated at cylinder values of <0.75,>/= 0.75 to <1.50,>/=1.50 to <2.00, and >/= 2.00D.
6. Amblyopia was regarded as the cause of impairment in eyes with best-corrected VA(BCVA) equal to or worse than 20/40 (6/12) and no apparent organic lesion if one or more of the following criteria were met:
(1) Esotropia, exotropia or vertical tropia at 0.5m,
(2) Anisometropia of 2.00D spherical equivalent (SE) or more,
(3) Bilateral ametropia of at least +6.00D SE.
7. Uncorrected visual acuity is the visual acuity of the children without any spectacles whether the child has spectacles or not.
8. Presenting visual acuity is the visual acuity of the child with habitual glasses if worn to school or visual acuity without glasses if the child has no glasses.
Data Management and Analysis
All the data were recorded on a standardized questionnaire. Data cleaning was done on-site by the principal investigator and the questionnaires were checked for completeness and accuracy of entries. Coding and double entry of data were done in the research office by the 2 data entry clerks, after another round of cleaning. Measurement data ranges, frequency distributions, and consistency among related measurements were checked with data cleaning programs. Statistical analysis was done with Statistical Package for Social Sciences (SPSS), version 22 (SPSS Inc., Chicago, Illinois, USA). The prevalence of visual impairment based on UCVA, presenting VA and BCVA was calculated. Statistical tests of significance were conducted using the Chi-square test for proportion, as appropriate. Confidence intervals (95% CIs) and probabilities significance at <0.05 for prevalence estimates were calculated.
Results
A total of 5723 children were examined during the study period comprising 2686 (46.9%) males and 3037 (53.1%) females; (M:F ratio 0.9:1) and aged 10.49±2.74SD of mean (range, 5 to 15 years). The age group 12 to <13 accounted for highest 776 (13.6%) of the study participants. The demographic characteristics of the children is as shown in Table 1. The children were predominantly in public schools 3200 (55.9%) in urban areas 2873 (50.2%) and attending primary schools 3762 (65.7%).
 |
Table 1 Demographic Characteristics of School Children Surveyed |
Uncorrected visual acuity of 20/32 or better in at least one eye was found in 5524 (96.5%) of children; Table 2. One hundred and ninety-eight (5.3%) children had visual impairment (20/40 or worse) with 5(0.08%) of these blind (20/200 or worse). The uncorrected, presenting and best-corrected VA of <20/40 (6/12) was noted in 188 (3.4%) children, 182 (3.4%) children and 14 (0.2%) children, respectively. A total of 55 children were wearing spectacles, and among the 198 children with visual impairment in both eyes based on uncorrected vision, 25 (12.6%) had spectacles. With testing of best-corrected visual acuity, it was possible to reduce the bilateral visual impairment to 16 (0.25%).
 |
Table 2 Distribution of Uncorrected, Presenting and Best-Corrected Visual Acuity |
Refractive error is the principal cause of visual impairment (Table 3). Amblyopia, satisfying the predefined criteria, was the second main cause of amblyopia in 30 eyes (5.8%); 15 each of right and left eyes. The cause of visual impairment was undetermined in 19 eyes. Children who either were wearing or not wearing spectacles, had VA improvement with pinhole but did not undergo auto-refraction because they were uncooperative were classified as presumed refractive error.
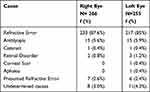 |
Table 3 Primary Causes of Visual Impairment |
The age-sex specific prevalence of refractive error was 2.1% across all age groups and gender; (Table 4). The prevalence of refractive error is higher in females (2.5%) p = 0.003. The prevalence of hypermetropia and myopia was 0.1% and 2.0%, respectively.
 |
Table 4 Age, Sex and Location Specific Prevalence of Refractive Error in Children |
There is a statistically significant higher prevalence of refractive error in urban schools (84, 2.9%, p=0.001) and in the 7th grade class (28,4.2%, p=0.001)
Imo State has the highest prevalence of 3.4% while Abia state had the lowest (1.2%) (Table 5)
 |
Table 5 State Specific Prevalence of Refractive Error |
Visual impairment with astigmatism of 0.75D or greater was found in 114 (2.0%) right eyes and in 134 (2.3%) left eyes (Table 6).
 |
Table 6 Prevalence of Visual Impairment with Astigmatism |
Discussion
This survey provides reliable and comparative data on prevalence of refractive error and visual impairment amongst school-aged children in the south-eastern region of Nigeria. This is the first survey in Nigeria using the RESC protocol.
There is an overall slight female preponderance in this survey and in keeping with a similar survey in Brazil.19 This may be a reflection of the outcome of consistent global advocacy for the girl child education particularly in low- and middle-income countries.
The prevalence of uncorrected, presenting and best-corrected visual acuity of ≤20/40 in the better eye in this study was 3.4%, 3.4% and 0.2%, respectively. Other investigators have reported similar,21 higher,19 and lower22 prevalence rates. The differences in study populations with attendant variations in genetic and environmental influences in the aetio-pathogenesis of visual impairment in the children could account for these differences.
The prevalence of refractive error in this survey was found to be 2.1% across all age groups and gender. Of the 120 children with refractive error, 84 were seen in the urban schools. Most of the refractive errors were due to myopia (2.0%) occurring more in the female cohort, children in 7th grade and among urban school populations. This is lower than the 4.1% reported in India,15 Chile (6.8%)14 and China (16.2%).23 Syaratul-Emma et al24 reported a higher refractive error prevalence of 7% in a similar survey using same definitions. However, the study populations were wholly primary school children in sub-urban areas of Malaysia, while almost 50% of our cohorts were in rural schools. Same study24 observed that better socio-economic factors may have contributed to the higher prevalence of refractive errors in metropolitan cities. This will be critical in resource distribution by eye-care providers in effectively combating vision loss among the pediatric population.
The overall prevalence of hyperopia of 0.1% is lower than the 0.78% in children from India,15 3.5% in China23 and 16.3% in Chile.14 The prevalence of astigmatism of 0.75D or more (2.0%) was comparable with the 2.8% reported in children from India15 and 2.2% from Nepal.13 However, there is wider discrepancy when compared with results from China24 (15%) and Chile14 (19%). Variations in data results could be due to variations in populations studied in different settings such as urban, semi-urban and core rural settings. Dandona et al15 reported findings from a predominantly rural Mahabubnagar district of India while our study was randomized among urban and rural settings of 5 states of Nigeria with comparable socio-economic status. Recent studies suggest that known genetic factors explain 35% of myopia,25 and that education can potentiate these effects. Lack of time spent outdoors, parental education and myopia are other important risk factors, with a systematic review suggesting that there is a 2% reduction in the progression of myopia with every hour spent outdoor.26
Refractive error is the principal cause of visual impairment in this survey accounting for 87.6% and 85% of the left and right eyes, respectively. This is consistent with reports from various RESC and non-RESC-based population and school-based surveys12–14,19,21–24 with varying rates. This underscores the reason for the inclusion of refractive errors as a priority area of global intervention in the WHO template for the global initiative for the elimination of avoidable blindness.27 Amblyopia ranked second as a cause visual impairment occurring in 5.6% and 5.9% of the right and left eye, respectively. Goh et al17 also reported that amblyopia is second only to refractive error as a cause of visual impairment. Though the aetio-pathogenesis of amblyopia is known to be multifactorial, uncorrected high refractive error has been noted to be a dominant cause of amblyopia in children.28 Baseline preventive measure implementation by eye-care stakeholders at all strategic levels will include; early case detection, eye examination, refraction, dispensing of glasses and follow-up to ensure compliance with prescription.27
Most of the children who needed refractive correction did not have them. This collaborates with reports of a similar survey in India15 and Brazil.19 An African survey29 have identified cost as the principal barrier to uptake of refractive services in a typical low- and middle-income (LMIC) setting as Nigeria. The implication for practice is that even in the uncertain presence of optical services, vulnerable and economically dependent children with significant refractive error will be unable to access optimal optical assistance.
As noted by Dandona et al,15 vision screening is critical in reducing visual impairment in children. However, this must be done by trained personnel with good refraction skill with a backup arrangement to provide corrective spectacles for those that need it and finally to include all school-aged children in and out of school.
The strength of this study lies in its large sample size. A potential limitation of this study is that it was school-based, which may not reflect the clinical conditions in these communities where a significant number of children may not attend school due to poverty. The school-based design is vulnerable to selection bias. In addition, severely visually impaired children are unlikely to be attending school.
Conclusion
Prevalence of children with VA less than 20/32 and refractive error is low. Myopia remains the dominant cause of refractive error predominantly in females and urban schools. Refractive error is the principal cause of visual impairment. However, most children do not have the needed spectacle for optimal optical correction and treatment. Effective school eye health program to identify children with refractive error in addition to providing free or affordable optical services remains the key to preventing visual impairment from refractive error particularly in resource-poor settings. Timely screening for the early detection of eye and vision problems in children is vital to avoid life-long visual impairment. Early detection provides the best opportunity for effective treatment.
Disclosure
This research was funded by the Tertiary Education Trust Fund (TETFUND) an initiative of the Ministry of Education of the Federal Republic of Nigeria. The authors reported no other potential conflicts of interest for this work.
References
1. The Eye Disease Prevalence Research Group. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol. 2004;122:495–505. doi:10.1001/archopht.122.4.495
2. Hyman L. Myopic and hyperopic refractive error in adults: an overview. Ophthalmic Epidemiol. 2007;14:192–197. doi:10.1080/09286580701535517
3. Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull of the World Health Organ. 2008;86(1):63–70. doi:10.2471/BLT.07.041210
4. He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in Southern China. Invest Ophthalmol Vis Sci. 2004;45:793–799.
5. Nepal BP, Koirala S, Adhikary S. Ocular morbidity in school children in Kathmandu. Br J Ophthalmol. 2002;87:531–534. doi:10.1136/bjo.87.5.531
6. Atinson J, Anker S, Nardini M, et al. Infant vision screening predicts failures on motor and cognitive tests up to school age. Strabismus. 2002;10:187–198. doi:10.1076/stra.10.3.187.8125
7. Agrawal D, Sahu A, Agrawal D, Prevalence of ocular morbidities among school children in Raipur district, India. Indian J Ophthalmol. 2020;68:340–344. doi:10.4103/ijo.IJO_1454_19
8. Shrestha GS, Sujakhu D, Joshi P. Refractive error among school children in Jhapa, Nepal. J Optom. 2011;4(2):49–55. doi:10.1016/S1888-4296(11)70041-3
9. Alam H, Siddiqui MI, Jafri SIA, Khan AS, Ahmed SI, Jafar M. Prevalence of refractive error in school children of Karachi. J Pak Med Assoc. 2008;58:322–325.
10. Ekpenyong BN, Naidoo K, Ndep A, Akpan M, Ekanem E. Prevalence and determinants of visual impairment amongst school-aged children in Southern Nigeria. Afr Vision Eye Health. 2020;79(1):a534.
11. Megbelayin OE, Asana EU. Visual impairment among school children- Calabar vision screening survey in secondary schools. Internet J Ophthalmol Visual Sci. 2013;10(1):1–8.
12. Negrel AD, Maul E, Pokharel GP, et al. Refractive error study in children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129:421–426. doi:10.1016/S0002-9394(99)00455-9
13. Pokharel GP, Negrel AD, Munoz SR, Ellwein LB. Refractive error study in children: results from Mechi zone, Nepal. Am J Ophthalmol. 2000;129:421–426. doi:10.1016/S0002-9394(99)00453-5
14. Maul E, Barroso S, Munoz SR, et al. Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol. 2000;129:445–454. doi:10.1016/S0002-9394(99)00454-7
15. Dandona R, Dandona L, Srinivias M, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:623–631.
16. Naidoo KS, Raghunandan A, Mashige KP, et al. Refractive error and visual impairment in African children in South Africa. Invest Ophthamol Vis Sci. 2003;44:3764–3770. doi:10.1167/iovs.03-0283
17. Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB. Refractive error and visual impairment in school-age children in Gomba District, Malaysia. Ophthalmology. 2005;112:678–685. doi:10.1016/j.ophtha.2004.10.048
18. World Health Organization. Assessment of the prevalence of visual impairment attributable to refractive error or other causes in school children. Available from: https://www.who.int/blindness/causes/RESCProtocol.pdf.
19. Salamao SR, Cinoto RW, Berezovsky A, et al. Prevalence and causes of visual impairment in low-middle income school children in Sao-Paulo, Brazil. Invest Ophthalmol Vis Sci. 2008;49(10):4308–4313. doi:10.1167/iovs.08-2073
20. National School Eye Health Guideline, Federal Ministry of Health, Nigeria 2020. Available from: https://www.health.gov.ng/doc/National-School-Eye-Health-Guidelines.pdf.
21. Kumah BD, Ebri A, Abdul-Kabir M, et al. Refractive error and visual impairment in private schools in Ghana. Optom Vis Sci. 2013;90(12):1456–1461. doi:10.1097/OPX.0000000000000099
22. Rezvan F, Khabazhoob M, Fotouhi A, et al. Prevalence of refractive errors among school children in Northeastern Iran. Ophthalmic Physiol Opt. 2012;32(1):25–30. doi:10.1111/j.1475-1313.2011.00879.x
23. Zhao J, Pan X, Sui R, et al. Refractive error study in children: results from Shunyi District, China. Am J Ophthalmol. 2000;129:41–426. doi:10.1016/S0002-9394(99)00452-3
24. Syaratul-Emma H, Tan H-K, Wan-Hazabbah WH, Mohtar I. Prevalence of refractive error in Malay primary school children in suburban area of Kota Bharu, Kelantan, Malaysia. Ann Acad Med Singapore. 2008;37:940–946.
25. Jeremy A, GuggenheIim GK, Stuart AH. The heritability of high myopia: a reanalysis of Goldschmidt’s data. J Med Genet. 2009;37:210–212.
26. Sherwin JRM, Keogh R, Khawaja A, Mackey D, Foster P. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012;119(10):2141–2151. doi:10.1016/j.ophtha.2012.04.020
27. Global initiatives for the Elimination of Avoidable Blindness. Action Plan 2006-2011. Available from: www.who.int/blindness/vision2020_report.pdf.
28. Rajavi Z, Sabbaghi H, Baghini A, et al. Prevalence of amblyopia and refractive errors among primary school children. J Ophthalmic Vis Res. 2015;10(4):408–416. doi:10.4103/2008-322X.176909
29. Thompson S, Naidoo K, Gonzalez-Alvarez C, Harris G, Mphil CF, Loughmen J. Barriers to use of refractive services in Mozambique. Optometry Vis Sci. 2015;92(1):1–11. doi:10.1097/OPX.0000000000000431
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
