Back to Journals » Clinical Ophthalmology » Volume 9
Recurrent rates and risk factors associated with recurrent painful bullous keratopathy after primary phototherapeutic keratectomy
Authors Kasetsuwan N , Sakpisuttivanit K, Reinprayoon U, Puangsricharern V
Received 25 May 2015
Accepted for publication 6 July 2015
Published 28 September 2015 Volume 2015:9 Pages 1815—1819
DOI https://doi.org/10.2147/OPTH.S89163
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ngamjit Kasetsuwan, Kanokorn Sakpisuttivanit, Usanee Reinprayoon, Vilavun Puangsricharern
Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand
Objective: To assess the recurrent rate, mean survival time, and risk factors associated with recurrent painful bullous keratopathy (BK) after primary treatment with phototherapeutic keratectomy.
Methods: Medical records from 72 patients (72 eyes) who had phototherapeutic keratectomy for painful BK were evaluated. Data for sex, age, duration of BK, associated ocular and systemic diseases (hypertension, diabetes mellitus, ischemic heart disease, asthma, dyslipidemia, and rheumatoid arthritis), frequency and degree of pain (grade 1–3), visual acuity, corneal thickness, intraocular pressure, and laser setting were extracted and analyzed.
Results: The mean age of the patients was 64.2±11.4 years. The mean preoperative duration of BK was 15.0±11.0 months. Most patients had pseudophakic BK (69.40%). Majority of the cases had grade 3 degree of pain (48.60%). Glaucoma and hypertension were markedly found among these patients (51.40% and 19.40%, respectively). Preoperative mean intraocular pressure and corneal thickness were 13.70±4.95 mmHg and 734.1±83.80 µm, respectively. The mean laser diameter and depth were 8.36±1.22 mm and 38.89±8.81 µm, respectively. Systemic disease was significantly associated with the risk for developing recurrent painful BK (P=0.022, hazard ratio [HR] 1.673, 95% confidence interval [CI] 1.08–2.58). The overall recurrent rate was 51%. The average duration time of recurrent painful BK was 17.3±12.9 months (range 1–50 months). The median survival time before recurrence was 29.0±6.6 months.
Conclusion: Systemic disease was found to be the only risk factor significantly associated with the development of recurrent painful BK. Low recurrent rate and long mean survival time showed that phototherapeutic keratectomy was effective in relieving recurrent painful BK and can be used as an alternative procedure for patients waiting for corneal transplantation.
Keywords: bullous keratopathy, recurrent painful, phototherapeutic keratectomy, PTK, risk factor, mean survival time
Introduction
Since 1983, argon fluoride (ArF) excimer laser was widely used for refractive surgery and treatment of corneal diseases.1 The laser emits ultraviolet light of 193 nm wavelength, and these radiations are immediately absorbed by the corneal surface; this causes minimal damage to the tissue surrounding the treatment zone. Its high energy breaks carbon–carbon bonds both within and between molecules, ablating the superficial tissue in a process known as the “photoablative decomposition” or “photoablation”. Furthermore, this laser is extremely precise in ablating 0.25 μm of tissue with just one pulse.
Excimer laser is used in phototherapeutic keratectomy (PTK) to treat corneal diseases. PTK has been used for more than 20 years, and its efficacy and safety have been verified. Many pathological corneal lesions are treated with this procedure.2–11 In 1995, PTK was approved by the US Food and Drug Administration for the treatment of corneal diseases such as epithelial basement membrane dystrophy, granular and lattice dystrophy, corneal scar and opacity (from trauma, infection, degeneration, and others), and irregular corneal surface (ie, Salzmann’s nodular degeneration, keratoconus nodule, and other irregular surface).4,6,7,9,11
However, there are no efficacy data on the use of PTK for the treatment of recurrent painful bullous keratopathy (BK). BK is a pathological condition characterized by the presence of corneal stromal edema and epithelial bullae due to endothelial dysfunction. Reduction or damage to the endothelial cell density results in the failure of the endothelial cell pump mechanism, which in turn leads to an imbalance due to dehydration in the cornea. Symptoms associated with this condition are severe loss of vision, ocular discomfort, tearing, photophobia, and intense pain when the bulla ruptures and exposes the corneal nerve endings. Management strategies for BK rely on the severity of the symptoms and potential visual acuity.
The treatment of choice for patients with good visual potential is a full-thickness corneal transplantation or endothelial keratoplasty, whereas for patients with poor visual prognosis, other modalities such as Gundersen flap, anterior stromal puncture, amniotic membrane transplantation (AMT), and PTK may be used to relieve the painful symptoms. There have been several reports on the efficacy of AMT and PTK in patients with BK. AMT, by itself, can provide a healthy substrate for epithelial healing by making the underlying surface smoother, but unfortunately, the adhesion between epithelium and the underlying tissue is not strong. This can lead to higher and earlier rates of recurrent BK. Therefore, it is recommended that AMT should be used along with PTK. This combination of procedures results in a painless postoperative recovery and a smoother surface with a longer symptom-free interval. Regardless of this advantage, to our knowledge, there are no reports on the use of PTK for the treatment of painful BK, risk factors, and mean survival time. Hence, this study aims to assess risk factors associated with the development of recurrent painful BK after primary treatment with PTK, the recurrent rate, and mean survival time.
Materials and methods
Medical records of patients who had PTK because of symptomatic, painful BK at the Chula Refractive Surgery Center of the King Chulalongkorn Memorial Hospital between October 1997 and September 2010 were reviewed. We excluded immunocompromised patients to avoid the effects of abnormal wound healing and response, as well as those with uncontrolled ocular inflammatory diseases.
Patients with painful BK, had PTK treatment, and were older than 18 years were included in the study.
Basic characteristics and demographic data of the patients before surgery were extracted from the medical records: medical history, sex, age, duration of BK, diagnosis, ocular-associated diseases, systemic underlying diseases, and frequency and severity of the pain, which were graded on a fixed response scale (Table 1). Other parameters were also collected: best corrected visual acuity (BCVA), central corneal thickness (CCT) (by ultrasonic pachymetry; Sonogage, Cleveland, OH, USA), intraocular pressure (IOP) (by applanation/noncontact tonometer), anterior segment details by slit-lamp biomicroscopy, and posterior segment status by dilated fundus examination or B-scan ultrasonography. All PTK procedures were performed under topical anesthesia (using 0.5% proparacaine hydrochloride), instilled three times every 5 minutes before the laser treatment. After a manual epithelial debridement using a hockey knife, laser ablation was performed with a 193 nm ArF excimer laser (Nidek EC 5000; Nidek, Tokyo, Japan). The depth and diameter of ablation zone were recorded. Postoperative parameters that were analyzed were BCVA, time to re-epithelialization (day), duration of being symptom free (months), and complications. The Snellen visual acuity both pre- and postoperation were converted into LogMAR system. The visual acuity was reported as counting fingers, hand motion, and light and no light perceptions, which were transformed into LogMAR by using Holladay’s technique.12 Missing data were excluded from the statistical analysis.
  | Table 1 Grading scale to assess pain of the patients |
Since this is a retrospective study, we obtained permission from the director of the King Chulalongkorn Memorial Hospital to access and use the patients’ data without getting the patients’ consent. This study was approved by the Ethical Committee of the Faculty of Medicine, Chulalongkorn University.
Statistical analysis
We used survival analysis to analyze the data. Kaplan–Meier curves with log-rank test were used to determine the significance of the categorical data. Numerical data were used in the Cox regression analysis. Only variables that had a trend to becoming significant were analyzed in the multivariate analysis by using the Cox regression hazard model to assess the possible risk factors associated with recurrent painful BK. Parameters with P-values of <0.05 were considered statistically significant. Statistical analyses were done by using SPSS (SPSS version 17.0 for Windows, IBM Corporation, Armonk, NY, USA).
Results
A total of 72 eyes from 72 patients were analyzed. There were 45 males and 27 females. The mean age of the patients was 64.2±11.4 years. The diseases associated with the patients prior to the surgery are shown in Table 2. The mean duration of BK before surgery was 15.0±11.0 months (range 1–72 months). The range of duration of follow-up was 1–77 months.
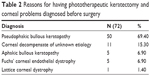  | Table 2 Reasons for having phototherapeutic keratectomy and corneal problems diagnosed before surgery |
The pain severity was found to be 48.6% (n=35), 38.9% (n=28), and 12.5% (n=9) in grade 3, 2, and 1, respectively.
Prevalence of ocular- and systemic-associated diseases among the study patients is shown in Tables 3 and 4, respectively.
  | Table 3 Prevalence of ocular-associated diseases among the study patients |
  | Table 4 Prevalence of systemic-associated diseases among the study patients |
Preoperative mean BCVA was 2.29±0.89 in LogMAR. The average IOP and CCT were 13.78±4.95 mmHg and 734.71±83.80 μm, respectively. The mean diameter and depth of laser ablation were 8.36±1.22 mm and 38.89±8.81 μm, respectively.
In the univariate analysis, systemic disease was identified as a significant risk factor for recurrence (P=0.009). Other variables were not significantly associated with survival in the univariate analysis. Duration of BK, preoperative visual acuity, and diameter of laser ablation showed trends toward significance and were added in to the multivariate Cox regression analysis. Multivariate analysis showed that systemic disease was significantly associated with the risk for recurrence (P=0.022, hazard ratio [HR] 1.67, 95% confidence interval [CI] 1.08–2.58) (Table 5).
Further, subgroup analysis was performed among these diseases and the recurrence of ischemic heart disease (IHD) was found to be statistically significant (HR =14.50). There was only one IHD patient in whom recurrent painful BK occurred 3 months after surgery.
Median survival time in regard to time to recurrence was 29.0±6.6 months, as shown in Figure 1. The survival rates were 80%, 54%, 46%, and 36% at 1, 2, 3, and 4 years of follow-up, respectively. The overall recurrent rate was 51% at the average time of 17.3±12.9 months (range 1–50 months). Postoperative mean BCVA in LogMAR was 2.24±0.84, which showed that there was a stable vision after surgery. The average complete re-epithelialization time was 7.03±4.13 days. No pain was experienced by all the patients after re-epithelialization was completed. None of the patients developed any complications after PTK.
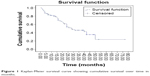  | Figure 1 Kaplan-Meier survival curve showing cumulative survival over time in months. |
Discussion
Penetrating keratoplasty (PK) is the treatment of choice for BK for improving the patients’ visual acuity and alleviating symptoms of pain, redness, and watering, and this is achieved by controlling the formation of the bullae. However, in developing countries such as India7 and Thailand, there is a lack of high-quality donor corneal tissue, and hence many patients end up on the long waiting list for keratoplasty, rather than being treated for the ailment. In Thailand, the average duration of time from registration to receiving the donated eyes for corneal transplantation surgery is approximately 36–60 months, but this time period is highly variable depending on other factors and criteria such as having unilateral/bilateral visual impairment or being a child. The treatment for painful BK includes the use of a combination of medications (ie, hyperosmotic agents, artificial tear solutions) and surgical procedures, such as anterior stromal puncture, AMT, PTK, etc. These surgical procedures have been shown to be effective, but the unavailability of amniotic membrane, long surgical time of AMT (~0.5–1 hour), and severe pain after anterior stromal puncture make them unattractive. In this study, we confirmed that all our patients who had a successful PTK for the treatment of painful BK did not suffer from severe pain after surgery.2,3,5,8 The vision of the patients was stable, which is evident from the BCVA values of 2.29±0.89 to 2.24±0.84 in LogMAR. This unchanged vision may cause patients more acceptable of the results compared to using amniotic membrane graft which may cause decrease of vision. In addition, a smoother anterior corneal surface and a stable tear film can make the patients feel more comfortable after surgery.7
However, the recurrence of BK after treatment is a matter of great concern. In our study, the risk factors for recurrence (duration of BK, preoperative visual acuity, and diameter of laser ablation) showed trends toward significance (Table 5). The duration of BK as well as preoperative visual acuity is important because, similar to chronic corneal stroma edema, they can lead to loss of corneal integrity in the diseased patients. Another factor that may influence the success of PTK is the diameter of the laser ablation. A larger ablation diameter may cause the corneal tissue to have a tighter adhesion to the underlying stroma, providing better results and hence delaying the recurrence of BK.
But according to both univariate and multivariate analyses, systemic diseases were shown to be significantly associated with the risk for recurrence (P=0.022, HR 1.67, 95% CI 1.08–2.58). In our study, systemic diseases such as hypertension (19.40%), diabetes mellitus (1.40%), and IHD (1.40%) were observed in the patients. It is possible that systemic diseases were strongly associated with recurrence because eye problems are more likely to be ignored. In addition, the mean age of the patients (64.2±11.4 years) in our tertiary care center indicates that they had poor health education as well as financial constraints because they were unable to control or monitor their health efficiently. These patients did not adhere to the medications prescribed by the ophthalmologists, which resulted in epitheliopathy of the corneal surface, recurrent corneal erosion, and painful symptoms.
Moreover, 9%–38.5% of the patients reported pain2,4,5 after PTK during the 36 months of follow-up.1,3,4 In our study, the overall recurrent rate was 51% with an average time of 17.3±12.9 months (range 1–50 months). As for the time to recurrence, the median survival time was 29.0±6.6 months. The survival rate at 1, 2, 3, and 4 years of follow-up were 80%, 54%, 46%, and 36%, respectively. Our data indicated that PTK was effective in treating painful BK and can be used as an alternative procedure in countries with limited resources. Even though PK is the standard and preferred treatment for painful BK, however, it should be noted that in many developing countries, donors are scarce and the waiting list is extremely long that it would be unethical to make the patients suffer from both visual deterioration and recurrent pain as they wait for their treatment.
One of the limitations of this study is its retrospective nature. In this study, CCT data for 44 eyes (61.1%) were missing and hence were excluded from the statistical analysis, which could have affected the final results obtained in this study. Regardless of this, our study had a higher recurrent rate when compared to other trials,2,4,5 but that is because our study had a longer follow-up period. Besides this, we are the first and the only group to report the recurrence rate and risk factors associated with the development of recurrent painful BK after primary treatment with PTK.
As a result of our findings, we recommend that ophthalmologists need to carefully evaluate, educate, and promote general health to the patients to avoid developing systemic diseases, which was one of the risk factors associated with recurrent painful BK. In addition, other modalities of the treatment, such as AMT and use of contact lens, combined with PTK may delay the recurrence. Therefore, it is important to promote and stimulate eye donation programs so that the patients with BK can quickly obtain the standard treatment of corneal transplantation as well as minimize the duration of suffering.
Conclusion
Both recurrent rate and mean survival time showed that PTK is an effective procedure that can be used as an alternative in patients waiting to undergo PK. Systemic underlying diseases were significantly associated with the risk of developing recurrent painful BK.
Disclosure
We declare that we have no conflicts of interest or proprietary interests related to this manuscript. This article has not been previously published or considered for publication elsewhere.
References
Trokel SL, Srinivasan R, Braren BA. Excimer laser surgery of cornea. Am J Ophthalmol. 1983;96:710–715. | ||
Thomann U, Meier-Gibbons F, Schipper I. Phototherapeutic keratectomy for bullous keratopathy. Br J Ophthalmol. 1995;79:335–338. | ||
Thomann U, Niesen U, Schipper I. Successful phototherapeutic keratectomy for recurrent erosion in bullous keratopathy. J Refract Surg. 1996;12(2):S290–S292. | ||
Foster W, Atzler U, Ratkay I, Busse H. Therapeutic use of 193-nm excimer laser in corneal pathologies. Graefes Arch Clin Exp Ophthalmol. 1997;235:296–305. | ||
Maini R, Sullivan L, Snibson GR, Taylor HR, Loughnan S. A comparison in different depth ablation in the treatment of painful bullous keratopathy with phototherapeutic keratectomy. Br J Ophthalmol. 2001;85:912–915. | ||
Fagerholm P. Phototherapeutic keratectomy: 12 years experience. Acta Ophthalmol Scand. 2003;81:19–32. | ||
Sharma N, Prakash G, Sinha R, Tandon R, Titiyal JS, Vajpayee RB. Indications and outcomes of phototherapeutic keratectomy in developing world. Cornea. 2008;27:44–49. | ||
Vyas S, Rathi V. Combined phototherapeutic keratectomy and amniotic membrane grafts for symptomatic bullous keratopathy. Cornea. 2009;28:1028–1031. | ||
Stasi K, Chuck RS. Update on phototherapeutic keratectomy. Curr Opin Ophthalmol. 2009;20:272–275. | ||
Chawla B, Sharma N, Radhika T, Kalaivani M, Titiyal JS, Vajpayee RB. Comparative evaluation of phototherapeutic keratectomy and amniotic membrane for management of symptomatic chronic bullous keratopathy. Cornea. 2010;29:976–979. | ||
Rapuano CJ. Excimer laser phototherapeutic keratectomy. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. China: Mosby Elsevier; 2011:1613–1623. | ||
Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13:388–391. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

