Back to Journals » Drug, Healthcare and Patient Safety » Volume 12
Rational Drug-Use Evaluation Based on World Health Organization Core Drug-Use Indicators in a Tertiary Referral Hospital, Northeast Ethiopia: A Cross-Sectional Study
Received 1 November 2019
Accepted for publication 4 January 2020
Published 16 January 2020 Volume 2020:12 Pages 15—21
DOI https://doi.org/10.2147/DHPS.S237021
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rajender R Aparasu
Desalegn Birara Mamo, 1 Belete Kassa Alemu 2
1Medicine Department, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Pharmacy, Pharmacology and Toxicology Unit, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Belete Kassa Alemu
Department of Pharmacy, College of Medicine and Health Sciences, Wollo University Address PO Box 1145, Dessie, Ethiopia
Tel +251 91 833 0307
Fax +251 333115052
Email [email protected]
Background: Irrational use of drugs is often observed in health-care systems throughout the world, particularly in developing countries. The World Health Organization estimates that more than half of all medicines are prescribed, dispensed, or sold inappropriately and that half of all patients fail to take them correctly. Therefore, the study was aimed at investigating the practice of rational drug use in a referral and teaching hospital in Northeast Ethiopia.
Methods: A hospital-based cross-sectional design was employed to conduct the study from February 2019 to May 2019. Systematic random sampling was used to select prescriptions dispensed in outpatient pharmacies. Convenient sampling was employed to select patient attendants and their prescriptions in outpatient departments during the study period. Data were collected using a structured and technical observational checklist for prescribing, patient care, and health-facility indicators. Face-to-face interviews were also employed to assess patient knowledge of correct dosage among patient-care indicators. Data were analyzed using SPSS version 20. Descriptive statistics are given using frequency, proportions, and summary measures.
Results: An average of 2.5 drugs per encounter were prescribed, with 34.64% and 13.80% of prescriptions being antibiotics and injections, respectively. Generics were used in 90.53% of prescription, and nearly 83% of drugs were prescribed from an essential-drug list. Average consultation and dispensing times were 1.57 minutes and 47 seconds, respectively. A total of 362 drugs were prescribed, with 82.6% actually dispensed and only 22.7% adequately labeled. The hospital had its own drug formulary and essential drug list, but no standard treatment guidelines. Moreover, except propyl thiouracil, all key essential drugs included in the study were available.
Conclusion: The majority of World Health Organization–stated core drug-use indicators were not met by the referral hospital in this study, which is especially problematic regarding patient-care indicators.
Keywords: rational drug use, WHO core drug-use indicators, prescribing indicators, patient-care indicators, health-facility indicators, Dessie Referral Hospital
Introduction
Rational drug use (RDU) is the process of appropriate prescribing, dispensing, and patient use of drugs for diagnosis, prevention, and treatment of diseases.1 It encompasses rational prescribing (good diagnosis practice and good prescribing practice, ie, the process of safe, effective, and economical ordering of drugs for the benefit of the patient), rational dispensing (the process of providing the right drug to the right patient in the right formulation or dosage, proper counseling, clear patient instructions, and good stock-management practice), and rational patient use (patient adherence/compliance).2–4
Even though drugs are important components of health care and play a crucial role in saving lives, their use is a complex issue concerning the physician, the dispenser, and the patient as a whole. The World Health Organization (WHO) has developed indicators to evaluate the practice of RDU in health facilities.2 These indicators are most often prescribing, health-facility, and patient-care indicators. According to the WHO, inappropriate prescribing and dispensing of medicines accounts for >50% of all medicines in the market and irrational use of medicines by patients results in various forms of health risks and costs.5
Irrational use usually arises from multiple prescribing and dispensing errors.6 The period that the dispenser has contact with the patient is an important factor that affects the quality of the patient-care process. As such, it is highly recommended that dispensers/pharmacists have sufficient time for proper counseling and dispensing of drugs to patients so that patients will have clear understanding of how to take medications and significantly improve drug adherence.3,7 Moreover, self-medication by patients is another cause of irrational DU.3
Inappropriate use of drugs is a common problem, especially in developing countries, substantially contributing to deleterious effects on health and economic burden. Therefore, this study was aimed at investigating the practice of RDU by using WHO DU indicators in Dessie Referral Hospital (DRH), in order to identify the extent of the problem, improve RDU practice, and provide information for further investigation.
Methods
Study Area, Design, and Period
DRH is the only public referral and teaching hospital in northeast Ethiopia — in Amhara regional state, South Wollo administrative zone — 401 km from Addis Ababa, the capital of Ethiopia. Currently, the hospital serves about 7 million patients. An institution-based, retrospective, cross-sectional study design was employed was used to evaluate prescribing indicators, while a prospective approach was employed for patient-care and facility indicators to assess the practice of RDU based on WHO core DU indicators in DRH. The study was conducted from February 2019 to May 2019.
Study Population
The study population comprised all those for whom prescriptions were dispensed in the outpatient pharmacy from February 2019 to May 2019 (prescribing indicators), whereas patient attendants and their outpatient prescriptions in daytime working hours from February 2019 to May 2019 were assessed for patient-care indicators. Drugs available most commonly and in Ethiopia's 2013 Essential Drug List (EDL) were considered as facility indicators.
Sample-Size Determination and Sampling
Prescribing Indicators
Based on WHO recommendations, 500 prescription encounters were taken from a total of 15,360 prescriptions that were dispensed in the hospital outpatient pharmacy from February 2019 to May 2019.2 With systematic random sampling, 500 outpatient prescriptions were selected by taking every thirty prescription in DRH. Average number of drugs per encounter, percentage of generic drugs prescribeds, percentage of prescriptions with antibiotics, percentage of prescriptions with injections, and percentage of prescribed drugs from EDL were determined.
Patient-Care Indicators
The WHO recommends that at least outpatient attendants (encounters) be included for a health facility.2 For a more reliable result, 150 patients were assessed by prospective convenient sampling. Only one outpatient pharmacy with five windows through which drug dispensating and consultation were done by five pharmacists every day was found.
Health-Facility Indicators
Every health facility must have a minimum of 20 essential drugs.2 In this study, to make the percentage availability of these drugs more feasible, 30 essential drugs were selected (Table 1). The drugs were selected based on the information that these key drugs are commonly used to manage top ten diseases of a hospital and are part of EDL of 2013 of Ethiopia.
 |
Table 1 Key Essential Drugs Selected in DRH in- and Outpatient Pharmacies as Health-Facility Indicator, February 1 to May 30, 2019 (n=30) |
Data-Collection Tools
A structured observational checklist was used to collect data on prescribing, facility, and patient-care indicators. Consultation and dispensing times were determined using a stopwatch. Face-to-face interview were usedto collect data on patient knowledge of correct drug information.
Data Quality Control
Training was provided to the data collectors and supervisors on how to collect and organize data. Frequent checks on the data-collection process to ensure completeness and consistency of the data collected were made. Pretesting of the data-collection instruments was done in Boru Meda Hospital, Dessie.
Data Processing and Analysis
Data were entered, processed, and analyzed using SPSS 20. In addition, WHO guidelines were used to evaluate the data explored in this study.
Results
Sociodemographic Characteristics
A total of 150 patients participated in the study to evaluate patient-care indicators, of which 63 (42%) were age range of 25–34 years. Males numbered 92 (61.3%), and 66 (44%) patients had completed primary school (Table 2).
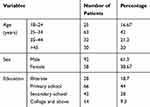 |
Table 2 Sociodemographic Characteristics of Patients in DRH OPP Interviewed for Patient-Care Indicators, February 1 to May 30, 2019 |
Prescribing Indicators
A total of 1,251 drugs were prescribed from 500 prescriptions by physicians (general practitioners, specialists, and subspecialists). The majority of the prescription encounters contained two drugs (224, 44.8%), followed by three drugs (159, 31.8%; Figure 1). It was found that an average of 2.5 drugs per encounter were prescribed. In addition, generics were used in 453 (90.53%) prescriptions, and 414 (82.83%) drugs from the EDL were prescribed. Furthermore, 173 (34.64%) prescriptions contained one or more antibiotics, and 69 (13.80%) injections were prescribed (Table 3).
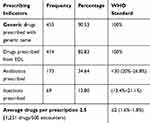 |
Table 3 Frequencies and Percentages of Prescribing Indicators in DRH, Eastern Amhara, Ethiopia, February 0 to May 30, 2019 as per WHO Criteria |
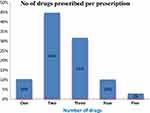 |
Figure 1 Distribution of drugs prescribed per encounter in DRH outpatient pharmacy from February 1 to May 30, 2019. |
Patient-Care Indictors
Average consultation and dispensing times in the present study were 1.57 minutes and 47 seconds, respectively. From a total of 362 drugs prescribed, 299 (82.6%) were actually dispensed, of which only 22.7% were adequately labeled (Table 4). From a total of 150 patients interviewed, 112 (74.67%) correctly responded and had adequate knowledge on how to take the medications (Table 5).
 |
Table 4 Average Dispensing and Consultation Times and Percentage of drugs dispensed and Labeled in DRH OPP from February 1 to May 30, 2019 |
 |
Table 5 Patient Knowledge of How to Take Correct Dosage in DRH OPP from February 1 to May 30, 2019 |
Health-Facility Indictors
The health facility has drug formularies and uses the EDL, but has no standard treatment guidelines (STGs). During the study period, all key essential drugs included in the study were available, except propyl thiouracil (Table 1).
Discussion
Prescribing Indicators
The average number of drugs per encounter in the current study was 2.5, which is higher than the standard set by the WHO (1.6–1.8).2 A similar study done in selected public hospitals of eastern Ethiopia, Bule Hora Hospital, and southern Ethiopia of eight hospitals showed that an average 2.34±1.08, 2.33, and 2.2 (1.7–2.7) drugs per encounter were prescribed, respectively, almost comparable with the present study.8–10 However, the result of the present study was higher than a study done in Jimma University Specialized Hospital (1.7).11 The observed likelihood of overprescribing drugs beyond the standard in the setting might be related to lack of adequate knowledge and training of health-care professionals and empirical prescribing and symptomatic treatment approaches. These prescribing habits may seriously affect health care by increasing drug interactions, adverse drug reactions, patient noncompliance, overuse and wastage of drugs, and increased patient costs for drugs, among others.2
In the current study, the proportion of generic drugs prescribed was found to be 90.53%, which is comparable to a study done in selected public hospitals of eastern Ethiopia (90.61%).8 This result was lower than the WHO standard (100%)2 and Bule Hora Hospital (96.8%).9 However, it was higher than studies conducted in southern Ethiopia of eight hospitals (78%)10 and Jimma University Specialized Hospital (87.15%).11 Even though the figure is large, as the study was conducted in a governmental hospital, a considerable number of prescriptions were prescribed by brand, significantly causing money wastage, due to purchasing branded drugs and difficulty of accessing these drugs.2 Prescription of some branded drugs in the study may have been due to doctors' linkage with drug promoters and business groups. The large health-care practice in Dessie attracts different business groups and drug promoters that galvanize the pharmaceutical market in the study area.
The proportion of antibiotic prescriptions was 34.64%, slightly higher than the WHO standard, which states that <30% of prescriptions should contain one or more antibiotics.2 This finding was also higher than the finding of studies conducted in Zimbabwe (29%),12 Jimma University Specialized Hospital (25.6%),11 and the United Arab Emirates (9.8%),13 but comparable with a study conducted in Latin American countries that showed the percentage of antibiotics prescribed was 27%–39%.1 However, the result of the present study was lower than the 63% in a study done in Sudan,14 57.87% in selected public hospitals in eastern Ethiopia,8 56% in Uganda,15 and 48% in Nigeria.16 Even though prescription of antibiotics in this study was generally acceptable compared to the WHO standard and other studies, overuse and irrational use of antibiotic has become a serious potential threat, due to the rapid emergence of antimicrobial resistance and the slow pace in the discovery and development of new antibacterial agents.
The proportion of encounters with injections in the present study was 13.8%, slightly higher than the WHO core DU-indicator standard (<10% of prescriptions should include injections)2 and the study done in selected public hospitals of eastern Ethiopia (10.9%).8 However, it was better than studies conducted in other parts of Ethiopia, such as 15% in southern Ethiopia (eight hospitals)10 and 20.3% in Bule Hora Hospital.9 There was a slight elevation from the WHO standard, which might have been due to prevalence of diabetic patients for whom insulin injection was commonly used and some sexually transmitted diseases being treated by ceftriaxone injection (gonorrhea) and 2.4 million U benzathine penicillin G (syphilis) in the hospital outpatient department.
Patient-Care Indicators
The time that prescribers and dispensers spend with each patient sets important limits on the potential quality of diagnosis and treatment. In the present study, the average times taken for consultation and dispensating of medicines were 1.57 minutes and 47 seconds, respectively. The average consultation time was considered very short (less than the 10 minutes of the WHO standard),2 and shorter than in other studies. A cross-sectional study done in selected public hospitals of eastern Ethiopia showed that average consultation and dispensing times were 4.61 minutes and 61.12 seconds, respectively.8 A study done in Bule Hora Hospital, southern Ethiopia showed an average consultation time of 5.50 minutes and average dispensing time of 1.22 minutes.9 Average consulting time in ten countries was 4.0 minutes,17 and average dispensing time in seven 105 seconds.18 Very short dispensating and consultation times in this study area might be due to high patient load because of the availability of only one outpatient pharmacy for the large catchment population. Very short dispensing times definitely affect appropriate labeling and provision of drug information, thereby increasing patient nonadherence.
From the prescribed medications in this study, only 82.6% drugs were actually dispensed, of which 22.7% were adequately labeled, far lower than the WHO standard (100%), while an average of 89% medicines were dispensed (12 countries) and 54% adequately labeled (eight countries) in other studies.17,18 The current study showed better than one done in selected public hospitals of eastern Ethiopia, which showed that only 75.77% of prescribed drugs were actually dispensed and 3.3% adequately labeled.8 Writing the patient’s name and generic name of the drug, expired date, strength, dosage, and total quantity of the drug on the label is necessary to help in reducing dispensing errors.
Regarding patient knowledge of correct dose and frequency, the present study highlighted that about 74.67% of interviewed patients correctly repeated the dose and frequency of each drug dispensed to them. This finding was almost in line with studies done in public hospitals of eastern Ethiopia (75.7%)8 and Bule Hora Hospital (73.3%).9 Knowledge of the patient is a very central factor in the therapeutic process. Even though the current study addressed dose and frequency to assess knowledge of patients, there should be comprehensive assessment of knowledge of side effects of drugs, drug interactions, drug–food interactions, names of dispensed medications, durations, and reason for taking the drug.
Health-Facility Indicators
The hospital has a national drug formulary and EDL, but no STGs. The WHO recommends the use of an EDL, STGs, and formulary for effective health delivery.2 In one study conducted in nine facilities, 78% had an EDL.1 However, in Ecuador only 38% of facilities had an EDL.5 On the other hand, except propyl thiouracil, all key essential drugs included in the study were available, which meant about 96.7% of key essential drugs were in stock during the study period. Essential medicines satisfy the precedence of health-care needs of the population and should be adequately available at all times. Careful selection of a limited range of essential medicines has several advantages in the supply, prescribing, cost, and patient use of medicines. All of these are even more important in resource-poor settings, where the availability of drugs in the sector is often erratic.19,20
Limitations of the Study
Evaluating RDU in health facilities based on WHO core DU indicators is critical to find major problem areas in the patient-care process. This study revealed actual gaps in RDU, but did not undertake qualitative investigation of the underlying causes of the problems in a hospital and failed to study whether prescribed drugs were in accordance with the diagnosis. Moreover, the study period was short and should be extended to 6, 9, or 12 months for better and valid evaluation of RDU.
Conclusion
Some RDU practices were not appropriate as evaluated by WHO core DU indicators, and especially more problematic with patient-care indicators. The average number of drugs per prescription and percentage of encounters dispensing antibiotics and injections were slightly above WHO recommendations, while the percentage of generic drugs prescribed was slightly lower than the WHO standard. Average consultation and dispensing times provided to patients at the pharmacy were found to be very short. Not all medications prescribed were dispensed within the hospital, substantialnumbers of drugs were not adequately labeled, and almost a quarter of patients were found to have inadequate knowledge about the correct dose and frequency of their medications. Moreover, the hospital had its own EDL and drug formulary, but no STGs, and most of the key essential drugs were in stock. Although the WHO benchmark for RDU was not met for all indicators, generally the study area is relatively good, especially with respect to most prescribing and health-facility indicators, though still requiring interventions in order to improve the practice of RDU.
Abbreviations
DRH, Dessie Referral Hospital; EDL, essential-drug list; RDU, rational drug use; STGs, standard treatment guidelines; WHO, World Health Organization.
Ethics Approval and Consent to Participate
Before the actual data-collection process, an official cooperation letter was obtained from Wollo University, College of Medicine and Health Sciences and submitted to the clinical director of the hospital. Then, data collection was commenced after permission from the director. Then, a brief explanation on objective of the study was provided to participants and written informed consent secured.
Data-Sharing Statement
All data generated or analyzed during this study are included in the manuscript and supplementary file (STROBE checklist for observational studies).
Acknowledgment
The authors would like to thank staff of DRH for their cooperation. We are also thankful to data collectors and the study participants.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Management sciences for health (MSH), Managing Drug Supply.
2. World Health Organization. How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators. Geneva: World Health Organization; 1993.
3. Drug Administration and Control Authority. Manual on Drug Supply Management. Addis Ababa, Ethiopia: Prepared by department of DACA; 1996.
4. World Health Organization. Promoting Rational Use of Medicines: Core Components. Geneva: World Health Organization; 2002.
5. World Health Organization, The world medicines situations: chapter 8, rational use of medicines, 2010. Available from: http://apps.who.int/medicinedocs/en/d/JS/6160e/10.html.
6. Drug Administration and Control Authority. Training Modules on Operation and Management of Special Pharmacies. Ethiopia: Birhane selam printing enterprise; 2003. Available from: http://daca.gov.et./downloads.html.
7. World Health Organization. The Role of the Pharmacist in the Health Care System: Preparing the Future Pharmacist: Curricular Development: Report of a Third WHO Consultative Group on the Role of the Pharmacist, Vancouver, Canada, 27–29 August 1997. Geneva: World Health Organization; 1997.
8. Sisay M, Mengistu G, Molla B, Amare F, Gabriel T. Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: a cross sectional study. BMC Health Serv Res. 2017;17(1):161. doi:10.1186/s12913-017-2097-3
9. Mariam AH, Raghavendra Y, Bobasa EM. Evaluating rational drug use with the help of World Health Organization’s core indicators in Bule Hora Hospital, Southern Ethiopia. Encounters. 2015;7(8):11.
10. Dilbato DD, Kuma ZG, Tekle-Mariam S. A baseline survey on prescribing indicators and the underlying factors influencing prescribing in Southern Ethiopia. Ethiop J Health Dev. 1998;12(2):87–94.
11. Yenet W. Baseline survey on drug prescribing indicators for outpatients in Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop J Health Sci. 2005;15(2).
12. Hogerzeil HV, Ross-Degnan D, Laing R, et al. Field tests for rational drug use in twelve developing countries. Lancet. 1993;342(8884):1408–1410. doi:10.1016/0140-6736(93)92760-Q
13. Mahmood A, Elnour AA, Ali AAA, Hassan NA, Shehab A, Bhagavathula AS. Evaluation of rational use of medicines (RUM) in four government hospitals in UAE. Saudi Pharm J. 2016;24(2):189–196. doi:10.1016/j.jsps.2015.03.003
14. Bannenberg W, Forshaw C, Fresle D, Salami A, Wahab H. Evaluation of the Nile Province Essential Drug Project. Geneva: WHO; 1991. WHO/DAP/91. 10. In: How to investigate drug use in health facilities. 2015.
15. Christensen R A strategy for the improvement of prescribing and drug use in rural health facilities in Uganda. Report for the Ministry of Health, Uganda: Uganda Essential Drugs Management Programme. 1990. doi:10.1099/00221287-136-2-327
16. Bimo D. Report on Nigerian field test. INRUD News. 1992;3(1):9–10. How to investigate drug use in health facilities Geneva: WHO. 1993:74.
17. Andom E. Drug Use Studies in Eritrean Health Facilities. Concentration paper Boston University School of Public Health, Department of International Health; 1999.
18. Arustiyono. Promoting rational drug use at the community health centers in Indonesia, Available from: http://dcc2.bumc.bu.edu/prdu/otherdocuments/ARUS/_INDONESIA_ PRDU_.htm.
19. World Health Organization. Model lists of essential drugs, 1977–2010. Geneva, Switzerland. Available from: http://www.who.int/medicines/services/essmedicines def/en/index.html.
20. Manual on Lists of Essential Medicines for Ethiopia.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
