Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Radiofrequency versus Ethanol Ablation for Single-Session Treatment of Benign Cystic Thyroid Nodules: A Short-Term Retrospective Study
Authors Nguyen VB , Nguyen Thi X , Nguyen Van Vy H, Pham Nguyen TL, Nguyen Hai T, Dinh Toan N , Le CV
Received 13 October 2022
Accepted for publication 11 January 2023
Published 24 January 2023 Volume 2023:19 Pages 97—104
DOI https://doi.org/10.2147/TCRM.S393213
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Van Bang Nguyen,1,* Xuan Nguyen Thi,1 Hau Nguyen Van Vy,1 Tuyen Linh Pham Nguyen,1 Thuy Nguyen Hai,2 Nguyen Dinh Toan,2 Chi Van Le2,*
1Center of Endocrinology and Diabetes, Family Hospital, Da Nang, Vietnam; 2Department of Internal Medicine, Hue University of Medicine and Pharmacy, Hue University, Hue City, Vietnam
*These authors contributed equally to this work
Correspondence: Van Bang Nguyen, Center of Endocrinology and Diabetes, Family Hospital, No. 73 Nguyen Huu Tho Str, Da Nang, Vietnam, Tel +84 973445417, Email [email protected] Chi Van Le, Department of Internal Medicine, Hue University of Medicine and Pharmacy, Hue University, Hue City, Vietnam, Tel +84913426457, Email [email protected]
Objective: This study aims to compare 1-month’s efficacy and safety of single-session ethanol ablation and radiofrequency ablation for treating both purely cystic nodules and predominantly cystic thyroid nodules.
Materials and methods: This short-term retrospective study was approved by the Ethics Committee of the Institutional Review Board of Danang Family hospital, and written informed consent for procedures was obtained for all patients. Thirty-nine patients who presented with cystic thyroid nodules and met inclusion criteria were extracted from the computerized medical records. The internal fluid of cystic thyroid nodules was aspirated as much as possible. Ethanol ablation was performed using 18-gauge needles with 99.5% ethanol, and RFA used a cooled-electrode RFA system and 18-gauge internally cooled electrodes via the trans-isthmic approach, moving-shot technique. Nodule volume, therapeutic success rate, the largest diameter, thyroid function tests, and complications were evaluated and compared before and after treatment in each group.
Results: Among 39 patients, 17 patients were undergone EA (mean age of 47.35 years; the proportion of female of 76.5%; purely thyroid cyst percentage of 41.4%) and 22 patients were undergone RFA (mean age of 46.63 years; the proportion of female of 86.4%; purely thyroid cyst percentage of 54.5%). Both treatment techniques showed a significant reduction of the largest diameter and nodule volume (p< 0.05) without complications. RFA reduced nodule volume and the largest nodule size greater than EA treatment at 1-month post-ablation (p< 0.05). In addition, the therapeutic success rate in the RFA group was higher than in the EA group.
Conclusion: Both RFA and EA treatment with single-session confirm the efficacy and safety for cystic thyroid nodules at 1-month follow-up, RFA reduced greater in nodule volume and the largest nodule size than the EA treatment. Thus, the therapeutic success rate in the RFA group was higher than in the EA group.
Keywords: radiofrequency ablation, ethanol ablation, cystic thyroid nodules, efficacy and safety
Introduction
Thyroid nodules are the 2nd most common endocrine disorder after diabetes.1 Among thyroid nodules, partially cystic accounted for 53.5%, with 13.7% described as greater than 75% cystic.2 The treatment of benign thyroid cystic nodules usually depends on the presence of compressible and/or cosmetic symptoms.
Ethanol ablation (EA), as well as radiofrequency ablation (RFA), for cystic thyroid nodules have been proven their efficacy according to nodule characteristics (solid proportion, vascularity, nodule size). However, a more effective technique for thyroid cystic nodule treatment is still debated. For purely cystic thyroid nodules, although RFA showed significantly greater volume reduction during the first 3 months after RFA, the difference seen at 6 months was not significant. Thus, EA has been recommended as the top priority because of its similar efficacy in volume reduction rate with fewer treatment sessions compared to RFA.3–5 However, for predominantly cystic thyroid nodules (PCTNs), EA shows a less volume reduction rate (VRR) with higher recurrence risk (from 26% to 33%) than RFA6,7 which is a result of regrowing or bleeding from the vascularity inside and around the solid component in PCTNs.6,8,9 Controversially, Baek et al conducted a single-blind, randomized trial which showed that the RFA’s efficacy in VRR is not superior to that of EA, 87.5 ± 11.5% for RFA and 82.4 ± 28.6% for EA.10 To the best of our knowledge, there is no study comparing the efficacy of 2 techniques in single-session treatment in both purely cystic nodules and PCTNs in short-term follow-up in Vietnam. Therefore, the purpose of this study was to compare 1 month’s efficacy and safety of single-session EA and RFA for treating both purely cystic nodules and PCTNs.
Methods
Study Design and Patient’s Selection
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Institutional Review Board of Danang Family hospital, Danang, Vietnam, and written informed consent for procedures was obtained for all patients.
We reviewed computerized medical records (Ehealth program) of 720 patients who underwent thyroid EA and RFA from May 2018 through December 2021 at the Centre of Endocrinology and Diabetes, Danang Family hospital, Danang, Vietnam. Fifty-six patients who presented with cystic thyroid nodules (purely cystic nodules and PCTNs) were extracted from the Ehealth program. Among them, 9 patients lacked the fine-needle aspiration cytology (FNAc) or thyroid function test results in the Ehealth program, and 8 patients lost to follow-up for unknown reasons. Finally, 39 patients (32 women and 7 men; 19 purely cystic nodules and 20 PCTNs) were involved in this study. Among the participants, 17 patients (13 women and 4 men; mean age, 47.35 years) were treated by EA, and 22 patients (19 women and 3 men; mean age, 46.63 years) were treated by RFA. All patients treated by EA or RFA above have been collected in this current study because they satisfied the following criteria: (1) nodules with greater than 50% of cystic portion; (2) present symptoms or cosmetic problems; (3) thyroid function including serum thyroid hormone (FT4) and thyrotropin concentrations (TSH) were collected; and (4) cytology confirmed benign thyroid nodules after two ultrasound-guided fine needle aspiration treatment technique (FNA); refusing for surgery; and being able to follow-up for at least 1-month post-ablation. For suitable patients, we already explained the advantages and disadvantages of thyroid EA or thyroid RFA to each patient before procedures.
Pre-Ablation Assessment
All patients underwent ultrasound performed by only one experienced radiologist in the same hospital. Ultrasound-guided FNA examinations were done by an endocrinologist (Nguyen VB), who has a licensed certificate as well as more than 5 years of experience in thyroid procedures (thyroid US-FNA/CNB, thyroid EA, and thyroid RFA). All cases have been applied an 8 to 12 MHz linear probe of a real-time ultrasound system (Acuson NX2 or NX3, Siemens Medical Solution, California, USA). Nodule size and internal fluid composition were evaluated on ultrasound. The three diameters of each nodule were measured, and the volume of each thyroid cyst was calculated as: V = πabc/6 (where V is volume; a, b, c are the 3 diameters), purely cystic was defined as nodules with <10% solid component, and PCTNs was defined as those with 10–50% solid component.11 Thyroid function was obtained before and a 1-month after the procedure.
Procedure
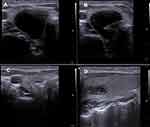
EA and RFA were performed in an outpatient ward with patients in the supine position and mild neck extension under ultrasound guidance by only one experienced endocrinologist. To prevent vascular injuries, we used Doppler ultrasonography to evaluate vascular structures along the approach way. After skin sterilization and local anesthesia with 2% lidocaine at the needle-puncture site and peri-thyroidal area (Figure 1A), we used an 18 gauge needle to puncture into the cyst under ultrasound guidance via the trans-isthmic approach. The internal fluid of cystic thyroid nodules was aspirated as much as possible by using a syringe of 20 mL or 50mL (Figure 1B). If the cysts contain high-viscosity fluid of colloid, the fluid was aspirated using a larger-bore needle (16 gauge), followed by injecting normal saline to remove colloid material before ethanol injection.
Ethanol Ablation Procedure
After finishing fluid aspiration, the volume of 99.5% ethanol injected via the same 18 gauge needle depended on the amount of aspirated fluid in the cyst, approximately 50–70% (Figure 1C). After 2 minutes of ethanol retention, the injected ethanol is aspirated as much as possible and the needle is withdrawn.12,13 Patients were asked to stay in the hospital for 30–60 minute after the procedure.
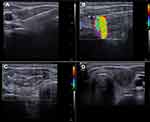
Radiofrequency Ablation Procedure
The internal cystic fluid was aspirated completely before ablating the nodule and its vascularity. An 18 gauge internally cooled monopolar electrode (5mm or 7mm in active tips) which was connected to a radiofrequency generator (CoATherm AK–F200, APRO KOREA Inc., Gyeonggi-do, Korea) was used to puncture into the nodule under US guidance via the trans-isthmic approach. The moving-shot technique was used to ablate the nodule from unit to unit (Figure 2A). Hydro-dissection was performed by slowly injecting 5% dextrose to protect important structures such as the nerve and artery. In addition, we tried to find the vascularities inside and around the nodules by using Doppler ultrasonography and ablated these as much as possible (Figure 2B). The nodules ablated completely were proven by the transient hyperechoic zone12,14,15 (Figure 2C).
Follow-Up
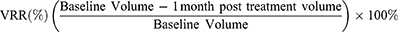
Follow-up ultrasound, thyroid function tests, and clinical examinations were identical to those performed before EA/RFA procedure and after 1 month (Figures 1D and (2D). Treatment efficacy (the primary endpoint) was assessed by measuring the VRR, and therapeutic success if VRR >50%. Safety outcomes (complications and side effects - the secondary endpoint) followed as reported by the international working group on image-guided tumor ablation. Major complications include substantial morbidity and disability, which increases the level of care, results in hospital admission, bleeding cases that need a blood transfusion, the case with permanent voice changes. Other complications were identified as minor complications (pain, transient voice change, etc.):16
Statistical Analysis
SPSS version 20.0 for Windows was used in this study for all statistical analyses. To compare sex distribution, age, initial nodule volume, largest nodule diameter, TSH, and FT4 between the two groups before treatment and efficacy at 1-month post-ablation, we applied the Mann–Whitney and Fisher’s exact tests. To assess the efficacy of the procedure by reductions in volume, the largest diameter, and thyroid function tests in each group, Wilcoxon’s signed rank test was used. The level of significance was defined as a p-value less than 0.05.
Results
From May 2018 through December 2021, 39 patients with a single purely thyroid cyst or PCTNs were identified via Ehealth program as qualified for inclusion. Among 39 patients, 17 patients were undergone EA (mean age of 47.35 years; the proportion of female of 76.5%; purely thyroid cyst percentage of 41.4%) and 22 patients were undergone RFA (mean age of 46.63 years; the proportion of female of 86.4%; purely thyroid cyst percentage of 54.5%).
About the treatment characteristics, the RFA’s meantime was 15.65 ± 9.24 minutes (range, 4.0–35 minutes) and the mean minimum and maximum RF power used were 17.95 ± 3.67 watts (range, 10–25 watts) and 32.05 ± 7.97 watts (range, 20–50 watts). The retention time of ethanol was 2 minutes in all cases. No major or minor complications were encountered in both groups.
Table 1 shows the patient demographic and initial nodule features of the two study groups. The figure showed no statistically significant differences between the two groups in gender, age, largest diameter, nodule volume, FT4 concentration, type of thyroid cyst, and volume of fluid aspirated but the TSH concentration and cost of treatment were significantly higher in the RFA group.
 |
Table 1 Baseline Characteristics of the Ethanol Ablation and Radiofrequency Ablation Groups |
Table 2 depicts the outcomes of EA and RFA treatment for cystic thyroid nodules. The largest diameter and volume of cystic thyroid nodules witnessed a significant decrease, while TSH and FT4 level were no significant differences after the 1-month follow-up.
 |
Table 2 Outcomes of the Ethanol Ablation and Radiofrequency Ablation Groups |
The comparison of therapeutic results at 1-month follow-up in the two groups is shown in Table 3. The mean volume reduction rate of the RFA group was 72.41 ± 23.17%, which was significantly higher than that of the EA group, 53.09 ± 26.23%. Regarding the subtype of thyroid cyst, the average VRR of the RFA group was significantly greater than that of the EA group in the purely thyroid cysts subgroup and there was no statistically significant difference in the PCTNs subgroup.
 |
Table 3 Results in the Ethanol Ablation and Radiofrequency Ablation Groups at 1 Month Follow-Up |
In the RFA group, the therapeutic success rate was 90.9%, while that for the EA group was 52.9%. This was a statistically significant difference between the two groups (p < 0.05). Although the difference between the two groups in terms of therapeutic success was not statistically significant in the purely thyroid cyst subgroup, this difference was significant in the PCTNs subgroup. It is noticeable that the figure for the largest diameter reduction was higher in the RFA group than that in the EA group (p<0.05). Meanwhile, thyroid function tests including TSH and FT4 levels were normal in all patients and not different in these groups during follow-up.
Discussion
In recent years, RFA and EA have been one of the minimally invasive alternative treatments of benign thyroid nodule(s) (including solid-cystic nonfunctioning benign nodules, autonomously functioning thyroid nodules, low-risk papillary thyroid carcinoma, and recurrent thyroid cancers).9,17–23 Our study demonstrated that both RFA and EA treatment with single-session confirm the efficacy and safety for cystic thyroid nodules at 1-month follow-up. Both treatment techniques showed a significant reduction of the largest diameter and nodule volume without complications, while no significant change in thyroid function tests was observed. Also, regarding efficacy, RFA reduced nodule volume and the largest nodule size at 1-month post-ablation by 72.4% and 9.89mm, which was greater than with EA treatment by 53.09% and 5.40mm. Thus, the therapeutic success rate in the RFA group was higher than the EA group. These results are in line with the previous findings, where it has been demonstrated that RFA showed better volume reduction than EA at 1-month post ablation and long-term period.8,24–26 In addition, in terms of thyroid function tests and complications, there were no significant differences between these two techniques. It is noticeable that in the purely thyroid cysts subgroup, the mean VRR of the RFA group was significantly higher than that of the EA group, while there was no statistically significant difference in the PCTNs subgroup. In contrast, some previous studies showed that RFA treatment is not significantly different from EA in terms of therapeutic efficacy as well as therapeutic safety for thyroid cyst nodules in short-term and long-term follow-up and EA is fewer treatment sessions and is less expensive than RFA.3,10,27 The reason for the similar results in both RFA and EA groups in previous studies was the presence of nodule’s colloid material as well as bleeding from the inside vascular solid component and around the cyst which was related to slow volume reduction, recurrence, and a need for repeat treatment.3,10 From this experience from these studies, we tried to remove completely internal viscous fluid before RFA and to find the vascularities inside and around the nodules by using Doppler ultrasonography and ablated these as much as possible. Baek et al explained that EA was less effective and easy to recurrence because venous inside the solid component and around the thyroid cyst absorb the injected ethanol10 and RFA showed good results for these recurrent cases.28
This study has three main limitations. Firstly, this study had a short-term follow-up of 1 month and a small sample size. In many longer follow-up studies, RFA proved the significantly greater VRR of cystic nodules at 1 and 3 months after ablation, however, the difference at 6 months was not significant.10,24 So, our study only showed the short-term result. The second limitation is retrospective study with convenience sampling which had selection bias. Also, since the data was not collected in a predesigned proforma as per the specific requirements of the study, some data would inevitably be missing. Finally, in the design of the study as a retrospective study, vascularity grade, cosmetic, and symptom score were not included because this information was not enough in computerized medical records (Ehealth). These limitations inspire our group to do larger and longer well-designed prospective blinded randomized studies to compare exactly the efficacy and safety of EA and RFA treatment for cystic thyroid nodules.
In conclusion, both RFA and EA treatment with single-session confirm the efficacy and safety for cystic thyroid nodules at 1-month follow-up, RFA reduced greater in nodule volume and the largest nodule size than the EA treatment. In addition, the therapeutic success rate in the RFA group was higher than in the EA group.
Abbreviations
CNB, Core needle biopsy; FNA, Fine Needle Aspiration; FT4, Free Thyroxine; PCTNs, predominantly cystic thyroid nodules; RF, Radiofrequency; RFA, Radiofrequency ablation; SD, Standard deviation; TSH, Thyrotropin; VRR, Volume Reduction Rate; US, ultrasound.
Data Sharing Statement
Availability of data and materials supporting our findings will be shared upon request.
Declarations
Ethics approval and consent to participate: Written informed consent form was given to patients.
Acknowledgments
The authors would like to thank the patients who agreed to collect their information in this study and Family Hospital, Danang, Vietnam for financial support.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Schlumberger MJ, Filetti S, Hay ID. Nontoxic diffuse and nodular goiter and thyroid neoplasia. In: Williams Textbook of Endocrinology. 2011:440–475.
2. Ross DS, Cooper D, Mulder J. Overview of thyroid nodule formation. In: U: Uptodate, Cooper DS. Waltham MA: UpToDate; 2017.
3. Sung JY, Kim YS, Choi H, Lee JH, Baek JH. Optimum first-line treatment technique for benign cystic thyroid nodules: ethanol ablation or radiofrequency ablation? Am J Roentgenol. 2011;196(2):W210–W214. doi:10.2214/AJR.10.5172
4. Deandrea M, Trimboli P, Creanza A, et al. Long-term follow-up of cystic thyroid nodules treated with percutaneous ethanol injection (PEI) using two different approaches. Euro J Endocrinol. 2020;183(5):489–495. doi:10.1530/EJE-20-0213
5. Cesareo R, Tabacco G, Naciu AM, et al. Long‐term efficacy and safety of percutaneous ethanol injection (PEI) in cystic thyroid nodules: a systematic review and meta‐analysis. Clin Endocrinol. 2022;96(2):97–106. doi:10.1111/cen.14530
6. Jang SW, Baek JH, Kim JK, et al. How to manage the patients with unsatisfactory results after ethanol ablation for thyroid nodules: role of radiofrequency ablation. Euro J Radiol. 2012;81(5):905–910. doi:10.1016/j.ejrad.2011.02.039
7. Lee JH, Kim YS, Lee D, Choi H, Yoo H, Baek JH. Radiofrequency ablation (RFA) of benign thyroid nodules in patients with incompletely resolved clinical problems after ethanol ablation (EA). World J Surg. 2010;34(7):1488–1493. doi:10.1007/s00268-010-0565-6
8. Valcavi R, Frasoldati A. Ultrasound-guided percutaneous ethanol injection therapy in thyroid cystic nodules. Endocrine Practice. 2004;10(3):269–275. doi:10.4158/EP.10.3.269
9. Park HS, Yim Y, Baek JH, Choi YJ, Shong YK, Lee JH. Ethanol ablation as a treatment strategy for benign cystic thyroid nodules: a comparison of the ethanol retention and aspiration techniques. Ultrasonography. 2019;38(2):166. doi:10.14366/usg.18033
10. Baek JH, Ha EJ, Choi YJ, Sung JY, Kim JK, Shong YK. Radiofrequency versus ethanol ablation for treating predominantly cystic thyroid nodules: a randomized clinical trial. Korean J Radiol. 2015;16(6):1332–1340. doi:10.3348/kjr.2015.16.6.1332
11. Shin JH, Baek JH, Chung J, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016;17(3):370–395.
12. Park HS, Baek JH, Choi YJ, Lee JH. Innovative techniques for image-guided ablation of benign thyroid nodules: combined ethanol and radiofrequency ablation. Korean J Radiol. 2017;18(3):461–469. doi:10.3348/kjr.2017.18.3.461
13. Hahn SY, Shin JH, Na DG, et al. Ethanol ablation of the thyroid nodules: 2018 consensus statement by the Korean Society of Thyroid Radiology. Korean J Radiol. 2019;20(4):609–620. doi:10.3348/kjr.2018.0696
14. Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. Am J Roentgenol. 2010;194(4):1137–1142. doi:10.2214/AJR.09.3372
15. Ha EJ, Baek JH, Che Y, et al. Radiofrequency ablation of benign thyroid nodules: recommendations from the Asian conference on tumor ablation task force. Ultrasonography. 2021;40(1):75. doi:10.14366/usg.20112
16. Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. J Vas InterRadiol. 2014;25(11):1691–1705. doi:10.1016/j.jvir.2014.08.027
17. Ha EJ, Baek JH, Lee JH. The efficacy and complications of radiofrequency ablation of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 2011;18(5):310–314. PMID: 21841482. doi:10.1097/MED.0b013e32834a9168
18. Cesareo R, Palermo A, Pasqualini V, et al. Efficacy and safety of a single radiofrequency ablation of solid benign non-functioning thyroid nodules. Arch Endocrinol Metab. 2017;61:173–179. doi:10.1590/2359-3997000000246
19. Che Y, Jin S, Shi C, et al. Treatment of benign thyroid nodules: comparison of surgery with radiofrequency ablation. Am J Neuroradiol. 2015;36(7):1321–1325. doi:10.3174/ajnr.A4276
20. Kim YJ, Baek JH, Ha EJ, et al. Cystic versus predominantly cystic thyroid nodules: efficacy of ethanol ablation and analysis of related factors. Eur Radiol. 2012;22(7):1573–1578. doi:10.1007/s00330-012-2406-5
21. Kanotra SP, Lateef M, Kirmani O. Non-surgical management of benign thyroid cysts: use of ultrasound-guided ethanol ablation. Postgraduate Med J. 2008;84(998):639–643. doi:10.1136/pgmj.2008.072777
22. Vu DL, Pham MT, Le TM. Efficacy and safety of radiofrequency ablation for the treatment of autonomously functioning thyroid nodules: a long-term prospective study. Ther Clin Risk Manag. 2022;18:11. doi:10.2147/TCRM.S344464
23. Nguyen VB, Nguyen TX, Nguyen VVH, Nguyen HT, Nguyen DT, Le CV. Efficacy and safety of single-session radiofrequency ablation in treating Benign thyroid nodules: a short-term prospective cohort study. Int J Endocrinol. 2021;2021:5.
24. Jeong WK, Baek JH, Rhim H, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008;18(6):1244–1250. doi:10.1007/s00330-008-0880-6
25. Cho YS, Lee HK, Ahn IM, et al. Sonographically guided ethanol sclerotherapy for benign thyroid cysts: results in 22 patients. Am J Roentgenol. 2000;174(1):213–216. doi:10.2214/ajr.174.1.1740213
26. Lee SJ, Ahn IM. Effectiveness of percutaneous ethanol injection therapy in benign nodular and cystic thyroid diseases: long-term follow-up experience. Endocrine J. 2005;52(4):455–462. doi:10.1507/endocrj.52.455
27. Sung JY, Baek JH, Kim KS, et al. Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective randomized study. Radiology. 2013;269(1):293–300. doi:10.1148/radiol.13122134
28. Kim DW. Usefulness of two-stage ethanol ablation in the treatment of benign predominantly cystic thyroid nodules. Endocrine Practice. 2014;20(6):548–555. doi:10.4158/EP13458.OR
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.