Back to Journals » Journal of Pain Research » Volume 14
Race Differences in Resilience Among Older Adults with Chronic Low Back Pain
Authors Morais CA , Fullwood D , Palit S, Fillingim RB, Robinson ME, Bartley EJ
Received 20 November 2020
Accepted for publication 3 February 2021
Published 9 March 2021 Volume 2021:14 Pages 653—663
DOI https://doi.org/10.2147/JPR.S293119
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jonathan Greenberg
Calia A Morais,1 Dottington Fullwood,2 Shreela Palit,1 Roger B Fillingim,1 Michael E Robinson,3 Emily J Bartley1
1Department of Community Dentistry and Behavioral Sciences, University of Florida, Gainesville, FL, USA; 2Institute on Aging, Department of Aging and Geriatric Research, University of Florida, Gainesville, FL, USA; 3Department of Clinical and Health Psychology, University of Florida, Gainesville, FL, USA
Correspondence: Calia A Morais
Department of Community Dentistry and Behavioral Sciences, University of Florida, 2004 Mowry Road, PO Box 100242, Gainesville, FL, 32610‑0404, USA
Tel +1 352-294-8881
Email [email protected]
Introduction: Racial minorities are disproportionally affected by pain. Compared to non-Hispanic Whites (NHWs), non-Hispanic Blacks (NHBs) report higher pain intensity, greater pain-related disability, and higher levels of mood disturbance. While risk factors contribute to these disparities, little is known regarding how sources of resilience influence these differences, despite the growing body of research supporting the protective role of resilience in pain and disability among older adults with chronic pain. The current study examined the association between psychological resilience and pain, and the moderating role of race across these relationships in older adults with chronic low back pain (cLBP).
Methods: This is a secondary analysis of the Adaptability and Resilience in Aging Adults (ARIAA). Participants completed measures of resilience (ie, gratitude, trait resilience, emotional support), as well as a performance-based measure assessing lower-extremity function and movement-evoked pain.
Results: There were 45 participants that identified as non-Hispanic White (NHW) and 15 participants that identified as non-Hispanic Black (NHB). Race was a significant correlate of pain outcomes with NHBs reporting greater movement-evoked pain (r = 0.27) than NHWs. After controlling for relevant sociodemographic characteristics, measures of movement-evoked pain were similar across both racial groups, F (1, 48) = 0.31, p = 0.57. Moderation analyses revealed that higher levels of gratitude (b = − 1.23, p = 0.02) and trait resilience (b = − 10.99, p = 0.02) were protective against movement-evoked pain in NHWs. In contrast, higher levels of gratitude were associated with lower functional performance in NHBs (b = − 0.13, p =0.02).
Discussion: These findings highlight racial differences in the relationship between resilience and pain-related outcomes among older adults with cLBP. Future studies should examine the potential benefits of targeted interventions that improve resilience and ameliorate pain disparities among racial minorities.
Keywords: racial differences, pain disparities, resilience, gratitude, older adults
Introduction
Chronic low back pain (cLBP) is the leading cause of disability worldwide.1 It is estimated that approximately 36% of older adults in the United States experience cLBP, making it one of the most prevalent health concerns and leading causes of disability among this cohort.1,2 The symptom burden of cLBP contributes to significant impairments in psychological and physical functioning, diminishing quality of life, and increasing pain-related disability.2 The impact of pain is greater for racial minorities, as non-Hispanic Blacks (NHBs) encounter higher rates of disabling and severe pain relative to non-Hispanic Whites (NHWs),3,4 an effect which contributes to adverse psychological outcomes such as higher rates of depression,5,6 disability7 and perceived stress.8 The high prevalence of cLBP and its adverse sequelae are particularly alarming, given the rapidly growing aging population in the United States.2
Behavioral interventions to reduce the symptom burden of pain have consistently targeted negative psychological states, such as fear-avoidance,9,10 pain catastrophizing,11,12 anxiety,13 and depression.14 While the relationship between negative psychological functioning and pain outcomes is well established,6,15 recent investigations have taken a broader view by examining the influence of resilience on pain-related experiences. Resilience is conceptualized as a dynamic and multifaceted process that promotes one’s ability to face and overcome stressors (ie, pain).16 Individuals with higher levels of resilience have the ability to quickly rebound from physiological or emotional stress, persist in meaningful activities despite ongoing hardship, and experience personal growth as a result of adversity, with multiple factors and resources contributing (eg, optimism, social support, positive affect).17
In recent years, a growing body of literature has highlighted the role of resilience factors on successful adaptation to pain.17–19 For example, optimism,20–22 hope,23 social support,24 and positive affect25,26 are associated with better pain-related outcomes. People with higher levels of trait resilience also report lower pain sensitivity, an increase in daily positive emotions, and reductions in daily reports of pain catastrophizing.27 Similarly, gratitude has been associated with a lower degree of negative emotions28 and increased subjective well-being.29
Interventions targeting positive, psychological processes (ie, positive activity interventions [PAIs]) such as social support, gratitude, optimism, and hope have also demonstrated adaptive benefits in clinical pain severity, psychosocial functioning, physical disability, and well-being.30–32 Combined, these findings support the protective role of resilience on pain and align with the Broaden-and-Build Theory of positive emotions, which posits that the accumulation of positive affective states increases personal resources through the broadening of one’s views, thoughts, and actions to promote adaptive coping.33
Considerable variability in pain and functioning exists across individuals, and evidence suggests that coping strategies differ across various racial and ethnic groups,34 thereby raising the possibility that resiliency may differentially influence pain among NHBs and NHWs. Indeed, emerging research from our group suggests that among older adults with knee osteoarthritis, higher optimism and positive well-being are protective against movement-evoked pain (ie, pain-induced upon movement) in NHBs, whereas positive affect is associated with lower movement-evoked pain in NHWs.3 These findings underscore the importance of identifying sources of resilience and their influence on pain and functioning across racial groups. Understanding these differences may facilitate the development of more culturally sensitive interventions that reduce racial disparities in pain and improve well-being among older adults.
The primary aim of this study was to examine race differences across resilience factors (ie, gratitude, trait resilience, emotional support) and pain-related outcomes (ie, movement-evoked pain, functional performance) among older adults with cLBP. As a secondary aim, we examined the moderating role of race in the relationship between resilience factors and pain outcomes. Though we anticipated differential effects across racial groups for these relationships based upon our previous research,18 no hypotheses were made regarding the direction of these effects given the limited research in this area. To the best of our knowledge, no studies have yet explored these associations in a sample of older adults with cLBP.
Materials and Methods
Participants
This cross-sectional study was based on a secondary data analysis from a larger study evaluating the effects of resilience mechanisms on pain modulation among individuals with chronic low back pain (cLBP). A total of 69 older adults (ages 60+ years) with cLBP were enrolled in the parent study.19 This sample size was determined based on pilot data suggesting that 60 participants would be necessary to achieve power = 0.80 at p = 0.05 to detect moderate to large effect sizes between measures of pain and resilience.18 The results reported in this paper are based on a sub-sample of participants (n = 60). A total of six participants were excluded from the final analyses due no longer meeting study criteria during their first laboratory appointment (n = 1: use of exclusion medications, n = 2: exclusionary medical condition, n = 3: not meeting pain duration criteria). In addition, a total of three participants did not identify as Non-Hispanic White (NHW) or Non-Hispanic Black (NHB), thus leaving 60 participants in the final analyses.
Participants were recruited from the community via flyers, media announcements, and word-of-mouth referrals. Participants were eligible to enroll in the study if they were ≥ 60 years of age and experienced at minimum mild LBP (≥ 2/10) for at least half of the days over the past three months. Exclusion criteria included the following: recent vertebral fracture; undergoing back surgery within the past six months; diagnosis of cauda equina syndrome; uncontrolled hypertension; severe cardiovascular disease; neurological diseases associated with somatosensory abnormalities (eg, neuropathy, seizures, Parkinson’s disease); current major medical illness (eg, metastatic or visceral disease); chronic opioid use; and systemic inflammatory disease (eg, spondyloarthropathies).
Procedures
All study procedures were approved by the University of Florida Review Board. Interested participants underwent a brief telephone screening to review study eligibility, and if eligible, they were scheduled for two study visits (2–3.5 hours each) held one week apart. During the first visit, participants provided informed consent in compliance with the Declaration of Helsinki and study eligibility was determined via self-reported demographic information and a medical history assessment. In addition, participants completed anthropometric measurements (ie, BMI), psychosocial questionnaires, and functional performance tests. Participants also completed several questionnaires at home between visit 1 and visit 2. Information regarding additional questionnaires administered as part of the parent study have been previously reported.18 Data collected during the second visit were not examined and are not included in this paper. Participants were compensated up to $100 for their participation.
Study Measures
Gratitude Questionnaire (GQ-6)
The 6-item GQ-6 was used to assess the disposition to experience gratitude in daily life (eg, “I have so much in life to be thankful for”).35 Participants rated their responses using a Likert scale with endpoints ranging from 1 (strongly disagree) to 7 (strongly agree). Reliability tests revealed good internal consistency for the study sample (Cronbach’s α = 0.86) that is consistent with published norms (Cronbach’s α = 0.84).35
Brief Resilience Scale (BRS)
The BRS assesses trait resilience, which captures an individual’s ability to bounce back and recover from stressful events and challenges.36 The BRS includes six items (eg, “I usually come through difficult times with little trouble”), and participants provided their responses using a 5-point Likert scale with endpoints ranging from 1 (strongly disagree) to 5 (strongly agree). The BRS was scored by calculating the sum of all six items (range 6–30) and then dividing by the number of items, resulting in a total score range of 1 to 5 (higher scores are indicative of greater resilience). The BRS demonstrated good internal consistency (Cronbach’s α = 0.84) in our sample, which is consistent with published norms (Cronbach’s α = 0.80 to 0.91).36
PROMIS Emotional Support
The short form of the PROMIS emotional support scale was used to assess social functioning (eg, “I have someone who will listen to me when I need to talk”).37 Participants responded to 8 items using a Likert scale with endpoints ranging from 1 (never) to 5 (always). A higher score represents more emotional support. The emotional domain of the PROMIS Social Support questionnaire has been shown to have high internal consistency (α = 0.99),37 which was excellent in our sample (α = 0.97).
Short Physical Performance Battery (SPPB)
The SPPB assesses functional capacity based on performance on three tests of lower-extremity function: standing balance, 4-minute walking speed, and the ability to rise from a chair. Participants receive a score based on their performance for each test with scores ranging from 0 (worst performance) to 4 (best performance). Total scores range from 0 to 12, with a higher score representing greater functional capacity and less disability.38 Movement-evoked pain (ie, pain induced upon movement) was determined by averaging pain ratings obtained from each functional capacity task.39 For this assessment, participants were asked to rate their current low back pain immediately after completion of each of the three tasks on the SPPB using a scale ranging from 0 (no pain) to 100 (most intense pain imaginable). The SPPB is a valid and reliable test of physical functioning with adequate internal consistency (Cronbach’s α = 0.63 to 0.66), and it is a good predictor of disability among older adults.40 In our sample, the internal consistency was acceptable (Cronbach’s α = 0.73).
Statistical Analysis
Statistical analyses were performed using SPSS 25.0, and the significance level was set at p < 0.05 (2-tailed). Race differences in demographic and clinical characteristics were assessed using chi-square for categorical variables (eg, marital status) and independent samples t-tests for continuous variables. Pearson’s correlations were performed to examine the association between sociodemographic characteristics and study variables (ie, resilience factors and pain-related outcomes). Race differences in psychological resilience and pain outcomes were tested using multivariate analysis of variance (MANOVA), and adjusted models were calculated to control for significant covariates (MANCOVA). Next, moderation analyses were conducted using Hayes’ PROCESS macro41 to examine the potential moderating effect of race on the relationships between resilience factors (ie, gratitude, trait resilience, emotional support) and pain outcomes (ie, functional performance, movement-evoked pain), while controlling for significant covariates. PROCESS is a tool that uses regression-based path-analytic modeling and automatically produces mean centering and conditional effects for moderation models. Categorical demographic variables that were entered in the moderation analyses were dummy coded as follows: sex as 0 = female and 1 = male, marital status as 0 = married, and 1 = not married. Partial eta squared (ηp2) was used to calculate effect sizes for group comparisons (small = 0.01, medium = 0.06, large = 0.14), and Cohen’s f 2 (small = 0.02, medium = 0.15, large = 0.35) was used to estimate effect sizes associated with significant findings from linear regression.42
Results
Sample Characteristics
Most of the participants were female (57%) and NHW (75%). The mean age was 68.3 years (SD = 7.2), and a substantial proportion of participants reported having a college degree (32%) and an annual income below $20,000 (34%). On average, participants reported having pain for 16.2 years (SD = 14.2) and the mean BMI was 28.8 kg/m2 (SD = 5.7). Table 1 shows significant race differences for age, sex, marital status, education, income, and BMI. These significant variables were entered as covariates in the moderation analyses.
 |
Table 1 Descriptive Characteristics of the Study Sample |
Pearson’s Correlations Across Study Measures
Table 2 presents the Pearson’s correlations between sociodemographic characteristics with resilience factors (gratitude, trait resilience, emotional support) and pain-related outcomes (functional performance-SPPB function, movement-evoked pain-SPPB pain). Across measures of resilience, being married was associated with higher trait resilience (p = 0.02) and greater perceived emotional support (p < 0.01). With regards to pain-related variables, being male and NHB was associated with a higher level of movement-evoked pain (p < 0.01 and p = 0.03, respectively). Greater education was associated with less movement-evoked pain (p = 0.04). There were no significant correlations between sociodemographic variables and SPBB function (ps > 0.05), with the exception that higher BMI was associated with lower physical performance (more physical disability) (p = 0.01).
 |
Table 2 Pearson Product-Moment Correlations Among Study Variables |
Race Differences Across Measures of Resilience and Pain
Table 3 shows race group differences across study variables. In the unadjusted analyses, NHBs reported greater movement-evoked pain compared to NHWs (p = 0.03); however, this effect was no longer significant after adjusting for covariates (p = 0.57). There were no other differences across race in psychosocial resilience measures or in physical functioning, although the effects for physical function (unadjusted analysis) approached significance (p = 0.06). In particular, NHBs exhibited lower physical function relative to NHWs.
 |
Table 3 Group Comparisons Across Psychological Resilience and Pain |
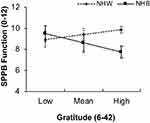
Moderation Analysis-Functional Performance
As seen in Table 4, after controlling for significant covariates (sex, age, marital status, income, education, and BMI), the overall moderation model for gratitude contributed 31% of the variance in functional performance (F = 2.25, R2 = 0.31, p = 0.03). There was a significant interaction between race and gratitude for SPPB function (b = −0.20, 95% confidence interval [CI] = −0.34 to −0.05, ΔR2 = 0.12, F = 7.81, p < 0.01, Cohen’s f 2 = 0.16, medium effect). The interaction plot (Figure 1) revealed a negative relationship between gratitude and functional performance for NHBs (b = −0.13, p = 0.02), and a positive relationship for NHWs that was not significant (b = 0.06, p = 0.13). There were no significant moderation effects observed for trait resilience (b = −0.99, 95% CI = −2.27 to 0.29, ΔR2 = 0.03, F= 2.41, p = 0.12) or emotional support (b = 0.06, 95% CI = −0.12 to 0.26, ΔR2 = 0.00, F = 0.49, p = 0.48).
 |
Table 4 Moderation Analysis for (A) Gratitude, (B) Trait Resilience, and (C) Emotional Support |
Moderation Analysis-Movement-Evoked Pain
After controlling for covariates, the overall model for gratitude was significant and explained 33% of the variance in movement-evoked pain (F = 2.45, R2 = 0.33, p = 0.02). There was a significant interaction between race and gratitude (b = 2.31, 95% CI = 0.60 to 4.02, ΔR2 = 0.11, F = 7.41, p < 0.01, Cohen’s f 2 = 0.17, medium effect). Simple slopes analysis (Figure 2) indicated that for NHWs there was an inverse relationship between gratitude and movement-evoked pain (b = −1.23, p = 0.02). These effects were not significant and in the opposite direction for NHBs (b = 1.07, p = 0.12).
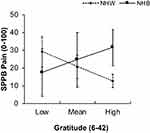 |
Figure 2 Relationship between gratitude and race for movement-evoked pain. Higher levels of gratitude were associated with lower movement-evoked pain for non-Hispanic Whites only. |
For trait resilience, the overall moderation model was significant and trait resilience accounted for 31% of the variance in movement-evoked pain (F = 2.37, R2 = 0.31, p = 0.02). As seen in Table 4, there was a significant interaction between race and trait resilience (b = 18.37, 95% CI = 3.32 to 33.41, ΔR2 = 0.09, F = 6.04, p = 0.01, Cohen’s f 2 = 0.13, small to medium effect). Simple slopes analyses (Figure 3) revealed that a higher level of trait resilience was associated with lower movement-evoked pain among NHWs (b = −10.99, p = 0.02); however, this relationship was non-significant and in the opposite direction for NHBs (b = 7.37, p = 0.20). The interaction between emotional support and race for movement-evoked pain was not significant (b = 1.54, 95% CI = −0.71 to 3.80, ΔR2 = 0.03, F = 1.90, p = 0.17).
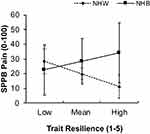 |
Figure 3 Relationship between trait resilience and race for movement-evoked pain. Higher levels of trait resilience were associated with lower movement-evoked pain for non-Hispanic Whites only. |
Discussion
The present study contributes to a growing body of research focused on improving our understanding of the impact of psychological resilience on pain-related outcomes among older adults. We expand on the previous literature by providing support regarding the relationships between resilience factors with pain and function and how they operate across racial groups. Our results bring attention to the potential buffering role of gratitude and trait resilience against movement-evoked pain among NHWs. With the expected older adult population increase and the growing racial and ethnic diversity of older adults,43 a better understanding of the factors that promote positive adjustment in individuals from various racial groups with chronic pain is needed.
Consistent with previous findings,3,44 we found that NHBs reported greater movement-evoked pain compared to NHWs; however, these differences were attenuated after controlling for clinical and sociodemographic characteristics (See Table 3). The causes underlying race differences in pain outcomes are complex, and the mechanisms operating on the relationship between sociodemographic factors, cultural experiences, and race are less clear. In the context of pain-related outcomes, lower socioeconomic status and perceived racial discrimination have been linked to greater pain severity and impairments in functioning.45,46 In a recent study, poverty level had a more significant impact on the pain experience of older adult NHBs compared to NHWs with knee osteoarthritis.47 These findings align with intersectionality theory which suggests that the convergent effects of various sociodemographic factors (eg, race, sex, age, SES) may help explain health disparities, including the impact of pain, across sociodemographic groups.48–50
Evidence also suggests that race differences in pain outcomes might be better accounted for by psychological variables and pain coping.51–53 Among low-income and minority populations, higher levels of depression were shown to mediate the relationship between race and pain-related outcomes.15 Pain catastrophizing, defined as a negative emotional and cognitive response to pain, has also been identified as a potential mechanism by which different racial groups respond to pain.54,55 Further, NHBs more frequently endorse the use of hoping, praying, and diverting attention as primary coping strategies for pain,56,57 effects which partially account for adverse pain outcomes among this group.58
Despite similar levels of gratitude and trait resilience across NHBs and NHWs, our results suggest that these resilience factors are differentially associated with pain-related outcomes across racial groups. Specifically, higher levels of gratitude and trait resilience were protective against movement-evoked pain among NHWs, signifying that augmenting these resources may be an important strategy to improve pain in this group. While future research is warranted to clarify the differential effects observed across race, our results underscore the important contribution of various sources of resilience on pain-related outcomes. In particular, our findings support the tenets of the Broaden-and-Build Theory, which proposes that positive emotions build personal resources to “undo” the consequences of adverse events.33 Evidence suggests that individuals with higher levels of gratitude adopt positive coping strategies (eg, reframing) and health-promoting behaviors that boost personal resources to adapt to adversity.59 In the context of pain, gratitude may prompt people to reinterpret pain as less aversive (ie, “I am glad/grateful for my cane/walker” and “I can keep going despite the pain”); in turn, this adaptive cognitive appraisal may lead to reductions in pain symptomatology. Discrete experiences of gratitude may also improve biological processes such as inflammation,60 and increase parasympathetic heart rate variability, which have been associated with reduced pain sensitivity.61 Likewise, higher levels of trait resilience may promote adaptation to pain by increasing motivational, goal-directed behaviors that augment one’s ability to face challenges.62 As a result, individuals may feel more assured about seeking and using pain reduction techniques to improve pain and function.
Conversely, there was a negative association between gratitude and physical functioning among NHBs. Although gratitude is generally associated with enhanced well-being and positive psychological function,63 there is also evidence linking gratitude to negative emotions such as indebtedness, guilt, and feelings of obligation.64 Despite the comparable levels of gratitude across our racial cohorts, it is possible that for NHBs, the degree of positive emotions evoked by gratitude may be insufficient to facilitate patterns of flexible thinking and shift attentional focus away from pain. However, this is speculative and warrants future investigation. The benefits of gratitude might also be driven by the frequency, intensity, and type of expression. Understanding the parameters by which sources of resilience, such as gratitude, impact pain and functioning among various demographic groups may be a step towards optimizing and tailoring our current therapeutic strategies.
While the advantages of positive, psychological processes have been established,16,17 evidence also highlights that these benefits are not universal.65,66 In fact, we did not observe a protective effect of emotional support on pain outcomes in our sample, which is in contrast with prior research.17,67 However, studies have addressed the need to distinguish between varying aspects of social support, including the quality and quantity of one’s social network and type of support received (eg, emotional and instrumental support), as these factors may differentially impact health and psychological function.16,68 Though varying facets of social support may demonstrate stronger relationships with pain and function among NHBs and NHWs with cLBP, this is an empirical question warranting further investigation.
Strengths and Limitations
To our knowledge, this is one of few investigations exploring the role of race on the relationship between sources of resilience and pain-related outcomes among older adults.3 Further, the examination of lower-extremity physical functioning provides unique information regarding functional capacity and limitations associated with cLBP, and our movement-evoked pain measure may be a better representation of an individual’s pain experience compared to retrospective pain ratings (static pain measure).19
Despite these strengths, there are limitations that warrant acknowledgment. First, the findings may not generalize to other patient populations varying in age and racial backgrounds. Second, our sample included individuals with cLBP, and it is unclear if the relationship between resilience and pain outcomes will also be moderated by race across other pain conditions. However, there is some initial evidence from our group that supports race differences in resilience factors among older adults with knee osteoarthritis.3 Third, the cross-sectional nature of the study limits the interpretation of the directionality and the conclusions made about the observed relationships. Fourth, given the multiple resources and processes contributing to resilience,18 it is also possible that other positive psychological constructs not examined in the current study limited our ability to capture processes that are protective in the experience of pain among NHBs. Indeed, resilience among NHBs has been attributed to a range of processes, including harmony, creativity, teamwork,69 and racial/ethnic identity.70 The extent to which individuals express positive feelings and views about their race has also been associated with positive psychological adjustment to stressors.71 However, the degree to which these cultural views and social experiences protect against pain among older NHBs with cLBP remains unexplored.
It is also worth examining resilience at the socioecological level, as the capacity to face and overcome stressors (ie, pain) is driven by the social environment in which pain occurs.18 Hence, community resilience (ie, bringing communities together for a common cause)72 may help facilitate a sense of belongingness in one’s community; thereby promoting positive adjustment through the upregulation of positive emotions (eg, pride).73,74 Therefore, future research should consider the interplay of individual and environmental resilience factors to help identify mechanisms influencing positive outcomes across demographic groups.
Lastly, it is important to acknowledge that while the parent study was adequately powered and we observed significant interaction effects in the current study, the disparity in sample sizes across racial groups (NHBs: n = 15; NHWs: n = 45) may have reduced the likelihood of detecting interaction effects among variables that were non-significant (ie, emotional support). The significant results reported in this study were of small to medium effect; thus, future studies with larger and diverse samples are needed to replicate these findings.
Conclusions
In sum, the current study contributes to the extant literature by highlighting the influence of race on the resilience–pain relationship. Importantly, findings suggest that gratitude and trait resilience may serve as protective agents against adverse pain outcomes among NHWs, while gratitude may lead to less optimal functional performance in NHBs. Given the limited research in this area, continued investigation is needed to replicate findings and illuminate the impact of various resilient factors across demographic groups. Likewise, the extent to which these findings may be applied clinically requires exploration. For instance, interventions focused on strengthening positive psychological processes such as positive affect, hope, optimism, and pain acceptance demonstrate adaptive effects on pain severity and other pain-related outcomes.23,30–32,60,75 Understanding the processes that promote resilience across various demographic groups may be a step towards developing culturally sensitive interventions that optimize pain management and reduce racial inequities in pain.
Acknowledgments
This research was supported by NIH/NIA Grants (K99AG052642, R00AG052642) awarded to EJB, NIH/NIA Grant (T32AG049673) provided to the University of Florida (CAM and SP), and NIH/NIA Grant (U01AG061389) to the University of Florida (DF). We thank Ralisa Pop, Stephanie Hersman, Morgan Ingram, Jordan McGee, Kylie Broskus, Paige McKenzie, and Michelle Jacomino for their assistance with data collection.
Disclosure Statement
The authors report no conflicts of interest in this work.
References
1. Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259.
2. Gibson SJ, Lussier D. Prevalence and relevance of pain in older persons. Pain Med. 2012;13(Suppl 2):S23–S26. doi:10.1111/j.1526-4637.2012.01349.x
3. Bartley EJ, Hossain NI, Gravlee CC, et al. Race/ethnicity moderates the association between psychosocial resilience and movement-evoked pain in knee osteoarthritis. ACR Open Rheumatol. 2019;1(1):16–25. doi:10.1002/acr2.1002
4. Meints SM, Cortes A, Morais CA, Edwards RR. Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Manag. 2019;9(3):317–334. doi:10.2217/pmt-2018-0030
5. Jeste DV, Savla GN, Thompson WK, et al. Association between older age and more successful aging: critical role of resilience and depression. Am J Psychiatry. 2013;170(2):188–196. doi:10.1176/appi.ajp.2012.12030386
6. Parmelee PA, Harralson TL, McPherron JA, DeCoster J, Schumacher HR. Pain, disability, and depression in osteoarthritis: effects of race and sex. J Aging Health. 2012;24(1):168–187. doi:10.1177/0898264311410425
7. Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52(4):1274–1282. doi:10.1002/art.20968
8. Taylor JL, Taylor JL, Parker L, Thorpe RJ, Whitfield KE. The relationship between pain and stress in older blacks. Innov Aging. 2019;3(Suppl 1):S70. doi:10.1093/geroni/igz038.274
9. Monticone M, Ferrante S, Rocca B, Baiardi P, Dal Farra F, Foti C. Effect of a long-lasting multidisciplinary program on disability and fear-avoidance behaviors in patients with chronic low back pain: results of a randomized controlled trial. Clin J Pain. 2013;29(11):929–938. doi:10.1097/AJP.0b013e31827fef7e
10. Richmond H, Hall AM, Copsey B, et al. The effectiveness of cognitive behavioural treatment for non-specific low back pain: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0134192. doi:10.1371/journal.pone.0134192
11. Darnall BD, Sturgeon JA, Kao M-C, Hah JM, Mackey SC. From catastrophizing to recovery: a pilot study of a single-session treatment for pain catastrophizing. J Pain Res. 2014;7:219. doi:10.2147/JPR.S62329
12. Burns JW, Day MA, Thorn BE. Is reduction in pain catastrophizing a therapeutic mechanism specific to cognitive-behavioral therapy for chronic pain? Transl Behav Med. 2012;2(1):22–29. doi:10.1007/s13142-011-0086-3
13. Wetherell JL, Afari N, Rutledge T, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain. 2011;152(9):2098–2107. doi:10.1016/j.pain.2011.05.016
14. Buhrman M, Syk M, Burvall O, Hartig T, Gordh T, Andersson G. Individualized guided internet-delivered cognitive-behavior therapy for chronic pain patients with comorbid depression and anxiety. Clin J Pain. 2015;31(6):504–516. doi:10.1097/AJP.0000000000000176
15. Newman AK, Van Dyke BP, Torres CA, et al. The relationship of sociodemographic and psychological variables with chronic pain variables in a low-income population. Pain. 2017;158(9):1687–1696. doi:10.1097/j.pain.0000000000000964
16. Bartley EJ, Palit S, Staud R. Predictors of osteoarthritis pain: the importance of resilience. Curr Rheumatol Rep. 2017;19(9):57. doi:10.1007/s11926-017-0683-3
17. Sturgeon JA, Zautra AJ. Resilience: a new paradigm for adaptation to chronic pain. Curr Pain Headache Rep. 2010;14(2):105–112. doi:10.1007/s11916-010-0095-9
18. Bartley EJ, Palit S, Fillingim RB, Robinson ME. Multisystem resiliency as a predictor of physical and psychological functioning in older adults with chronic low back pain. Front Psychol. 2019;10. doi:10.3389/fpsyg.2019.01932
19. Palit S, Fillingim RB, Bartley EJ. Pain resilience moderates the influence of negative pain beliefs on movement-evoked pain in older adults. J Behav Med. 2020;43:754–763. doi:10.1007/s10865-019-00110-8
20. Cruz-Almeida Y, Sibille KT, Goodin BR, et al. Racial and ethnic differences in older adults with knee osteoarthritis. Arthritis Rheumatol. 2014;66(7):1800–1810. doi:10.1002/art.38620
21. Goodin BR, Bulls HW. Optimism and the experience of pain: benefits of seeing the glass as half full. Curr Pain Headache Rep. 2013;17(5):329. doi:10.1007/s11916-013-0329-8
22. Hanssen MM, Peters ML, Vlaeyen JW, Meevissen YM, Vancleef LM. Optimism lowers pain: evidence of the causal status and underlying mechanisms. Pain®. 2013;154(1):53–58. doi:10.1016/j.pain.2012.08.006
23. Bartley E, Robinson M, Fillingim R. (494) Optimizing resilience in orofacial pain and nociception (ORION): exploring the efficacy of a hope intervention for pain. J Pain. 2016;17(4):S98. doi:10.1016/j.jpain.2016.01.301
24. Evers AW, Kraaimaat FW, Geenen R, Jacobs JW, Bijlsma JW. Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis. Behav Res Ther. 2003;41(11):1295–1310. doi:10.1016/S0005-7967(03)00036-6
25. Finan PH, Garland EL. The role of positive affect in pain and its treatment. Clin J Pain. 2015;31(2):177–187. doi:10.1097/AJP.0000000000000092
26. Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. J Consult Clin Psychol. 2005;73(2):212. doi:10.1037/0022-006X.73.2.212
27. Ong AD, Zautra AJ, Reid MC. Psychological resilience predicts decreases in pain catastrophizing through positive emotions. Psychol Aging. 2010;25(3):516. doi:10.1037/a0019384
28. Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol. 2003;84(2):365–376. doi:10.1037/0022-3514.84.2.365
29. Salces-Cubero IM, Ramírez-Fernández E, Ortega-Martínez AR. Strengths in older adults: differential effect of savoring, gratitude and optimism on well-being. Aging Ment Health. 2019;23(8):1017–1024. doi:10.1080/13607863.2018.1471585
30. Hausmann LRM, Ibrahim SA, Kwoh CK, et al. Rationale and design of the Staying Positive with Arthritis (SPA) study: a randomized controlled trial testing the impact of a positive psychology intervention on racial disparities in pain. Contemp Clin Trials. 2018;64:243–253. doi:10.1016/j.cct.2017.09.001
31. Muller R, Gertz KJ, Molton IR, et al. Effects of a tailored positive psychology intervention on well-being and pain in individuals with chronic pain and a physical disability: a feasibility trial. Clin J Pain. 2016;32(1):32–44. doi:10.1097/AJP.0000000000000225
32. Peters ML, Smeets E, Feijge M, et al. Happy despite pain: a randomized controlled trial of an 8-week internet-delivered positive psychology intervention for enhancing well-being in patients with chronic pain. Clin J Pain. 2017;33(11):962. doi:10.1097/AJP.0000000000000494
33. Fredrickson BL. The role of positive emotions in positive psychology: the broaden-and-build theory of positive emotions. Am Psychol. 2001;56(3):218. doi:10.1037/0003-066X.56.3.218
34. Meints SM, Miller MM, Hirsh AT. Differences in pain coping between black and white Americans: a meta-analysis. J Pain. 2016;17(6):642–653. doi:10.1016/j.jpain.2015.12.017
35. McCullough ME, Emmons RA, Tsang J-A. The grateful disposition: a conceptual and empirical topography. J Pers Soc Psychol. 2002;82(1):112. doi:10.1037/0022-3514.82.1.112
36. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi:10.1080/10705500802222972
37. Bartlett SJ, Orbai A-M, Duncan T, et al. Reliability and validity of selected PROMIS measures in people with rheumatoid arthritis. PLoS One. 2015;10(9):e0138543. doi:10.1371/journal.pone.0138543
38. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. JGerontol. 1994;49(2):M85–M94. doi:10.1093/geronj/49.2.M85
39. Corbett DB, Simon CB, Manini TM, George SZ, Riley III JL, Fillingim RB. Movement-evoked pain: transforming the way we understand and measure pain. Pain. 2019;160(4):757–761. doi:10.1097/j.pain.0000000000001431
40. Olsen CF, Bergland A. Reliability of the Norwegian version of the short physical performance battery in older people with and without dementia. BMC Geriatr. 2017;17(1):124. doi:10.1186/s12877-017-0514-4
41. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford publications; 2017.
42. Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2. doi:10.1037/a0024338
43. Ortman JMVV An aging nation: the older population in the United States. 2014.
44. Booker S, Cardoso J, Cruz-Almeida Y, et al. Movement-evoked pain, physical function, and perceived stress: an observational study of ethnic/racial differences in aging non-Hispanic Blacks and non-Hispanic Whites with knee osteoarthritis. Exp Gerontol. 2019;124:110622. doi:10.1016/j.exger.2019.05.011
45. Goodin BR, Phan QT, Glover TL, et al. Perceived racial discrimination, but not mistrust of medical researchers, predicts the heat pain tolerance of African Americans with symptomatic knee osteoarthritis. Health Psychol. 2013;32:1117–1126. doi:10.1037/a0031592
46. Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD. Racial and socioeconomic disparities in disabling chronic pain: findings from the health and retirement study. J Pain. 2017;18(12):1459–1467. doi:10.1016/j.jpain.2017.07.005
47. Thompson KA, Terry EL, Sibille KT, et al. At the intersection of ethnicity/race and poverty: knee pain and physical function. J Racial Ethnic Health Dispar. 2019;6(6):1131–1143. doi:10.1007/s40615-019-00615-7
48. Aroke EN, Jackson P, Overstreet DS, et al. Race, social status, and depressive symptoms: a moderated mediation analysis of chronic low back pain interference and severity. Clin J Pain. 2020;36(9):658–666. doi:10.1097/AJP.0000000000000849
49. McClendon J, Essien UR, Youk A, et al. Cumulative disadvantage and disparities in depression and pain among veterans with osteoarthritis: the role of perceived discrimination. Arthritis Care Res. 2020.
50. Quiton RL, Leibel DK, Boyd EL, Waldstein SR, Evans MK, Zonderman AB. Sociodemographic patterns of pain in an urban community sample: an examination of intersectional effects of sex, race, age, and poverty status. Pain. 2020;161(5):1044–1051. doi:10.1097/j.pain.0000000000001793
51. Day MA, Thorn BE. The relationship of demographic and psychosocial variables to pain-related outcomes in a rural chronic pain population. PAIN®. 2010;151(2):467–474. doi:10.1016/j.pain.2010.08.015
52. Edwards RR, Moric M, Husfeldt B, Buvanendran A, Ivankovich O. Ethnic similarities and differences in the chronic pain experience: a comparison of African American, Hispanic, and white patients. Pain Med. 2005;6(1):88–98. doi:10.1111/j.1526-4637.2005.05007.x
53. Jones AC, Kwoh CK, Groeneveld P, Mor M, Geng M, Ibrahim SA. Investigating racial differences in coping with chronic osteoarthritis pain. J Cross Cult Gerontol. 2008;23(4):339–347. doi:10.1007/s10823-008-9071-9
54. Forsythe LP, Thorn B, Day M, Shelby G. Race and sex differences in primary appraisals, catastrophizing, and experimental pain outcomes. J Pain. 2011;12(5):563–572. doi:10.1016/j.jpain.2010.11.003
55. Terry EL, Tanner JJ, Cardoso JS, et al. Associations of pain catastrophizing with pain-related brain structure in individuals with or at risk for knee osteoarthritis: sociodemographic considerations. Brain Imaging Behav. 2020;14:1–9. doi:10.1007/s11682-018-9957-2
56. Cano A, Mayo A, Ventimiglia M. Coping, pain severity, interference, and disability: the potential mediating and moderating roles of race and education. J Pain. 2006;7(7):459–468. doi:10.1016/j.jpain.2006.01.445
57. Meints SM, Mosher C, Rand KL, Ashburn-Nardo L, Hirsh AT. An experimental investigation of the relationships among race, prayer, and pain. Scand J Pain. 2018;18(3):545–553. doi:10.1515/sjpain-2018-0040
58. Meints SM, Stout M, Abplanalp S, Hirsh AT. Pain-related rumination, but not magnification or helplessness, mediates race and sex differences in experimental pain. J Pain. 2017;18(3):332–339. doi:10.1016/j.jpain.2016.11.005
59. Ng M-Y, Wong W-S. The differential effects of gratitude and sleep on psychological distress in patients with chronic pain. J Health Psychol. 2013;18(2):263–271. doi:10.1177/1359105312439733
60. Boggiss AL, Consedine NS, Brenton-Peters JM, Hofman PL, Serlachius AS. A systematic review of gratitude interventions: effects on physical health and health behaviors. J Psychosom Res. 2020;110165.
61. Appelhans BM, Luecken LJ. Heart rate variability and pain: associations of two interrelated homeostatic processes. Biol Psychol. 2008;77(2):174–182. doi:10.1016/j.biopsycho.2007.10.004
62. Goubert L, Trompetter H. Towards a science and practice of resilience in the face of pain. Eur J Pain (London, England). 2017;21(8):1301–1315. doi:10.1002/ejp.1062
63. Bartlett MY, Arpin SN. Gratitude and loneliness: enhancing health and well-being in older adults. Res Aging. 2019;41(8):772–793. doi:10.1177/0164027519845354
64. Watkins P, Scheer J, Ovnicek M, Kolts R. The debt of gratitude: dissociating gratitude and indebtedness. Cogn Emot. 2006;20(2):217–241. doi:10.1080/02699930500172291
65. Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. J Pers Soc Psychol. 2000;79(6):953–961. doi:10.1037/0022-3514.79.6.953
66. Cruza-Guet M-C, Spokane AR, Caskie GIL, Brown SC, Szapocznik J. The relationship between social support and psychological distress among Hispanic elders in Miami, Florida. J Couns Psychol. 2008;55(4):427–441. doi:10.1037/a0013501
67. Ethgen O, Vanparijs P, Delhalle S, Rosant S, Bruyère O, Reginster JY. Social support and health-related quality of life in hip and knee osteoarthritis. Qual Life Res. 2004;13(2):321–330. doi:10.1023/B:QURE.0000018492.40262.d1
68. Brown SL, Nesse RM, Vinokur AD, Smith DM. Providing social support may be more beneficial than receiving it: results from a prospective study of mortality. Psychol Sci. 2003;14(4):320–327. doi:10.1111/1467-9280.14461
69. Mattis, JS, Simpson NG, Powell W, Anderson RE, Kimbro LR, & Mattis JH. Positive psychology in African Americans. In: Chang EC, Downey CA, Hirsch JK, & Lin NJ, editors. Cultural, racial, and ethnic psychology book series. Positive psychology in racial and ethnic groups: Theory, research, and practice. American Psychological Association. 2016:83–107. doi:10.1037/14799-005
70. Ajibade A, Hook JN, Utsey SO, Davis DE, Van Tongeren DR. Racial/ethnic identity, religious commitment, and well-being in African Americans. J Black Psychol. 2016;42(3):244–258. doi:10.1177/0095798414568115
71. Franklin-Jackson D, Carter RT. The relationships between race-related stress, racial identity, and mental health for Black Americans. J Black Psychol. 2007;33(1):5–26. doi:10.1177/0095798406295092
72. Magis K. Community resilience: an indicator of social sustainability. Soc Nat Resour. 2010;23(5):401–416. doi:10.1080/08941920903305674
73. Seçkin G. I am proud and hopeful: age-based comparisons in positive coping affect among women who use online peer-support. J Psychosoc Oncol. 2011;29(5):573–591. doi:10.1080/07347332.2011.599361
74. Stein GL, Cavanaugh AM, Castro-Schilo L, Mejia Y, Plunkett SW. Making my family proud: the unique contribution of familism pride to the psychological adjustment of Latinx emerging adults. Cultur Divers Ethnic Minor Psychol. 2019;25(2):188–198. doi:10.1037/cdp0000223
75. Parks AC, Williams AL, Kackloudis GM, Stafford JL, Boucher EM, Honomichl RD. The effects of a digital well-being intervention on patients with chronic conditions: observational study. J Med Internet Res. 2020;22(1):e16211. doi:10.2196/16211
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.