Back to Journals » Patient Preference and Adherence » Volume 11
Questioning patient engagement: research scientists’ perceptions of the challenges of patient engagement in a cardiovascular research network
Authors Carroll SL , Embuldeniya G, Abelson J, McGillion M, Berkesse A, Healey JS
Received 23 February 2017
Accepted for publication 4 July 2017
Published 13 September 2017 Volume 2017:11 Pages 1573—1583
DOI https://doi.org/10.2147/PPA.S135457
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sandra L Carroll,1 Gayathri Embuldeniya,1 Julia Abelson,2 Michael McGillion,1 Alexandre Berkesse,3 Jeff S Healey4
1Faculty of Health Sciences, School of Nursing, McMaster University, Hamilton, ON, 2Faculty of Health Sciences, Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, ON, 3Faculty of Medicine, University of Montreal, Montreal, QC, 4Faculty of Health Sciences, Department of Medicine, McMaster University, Hamilton, ON, Canada
Background: Patient engagement in research is a dominant discourse in clinical research settings as it is seen as a move toward sustainable and equitable health care systems. In Canada, a key driver is the Strategy for Patient-Oriented Research of the Canadian Institutes of Health Research, which asserts that meaningful patient engagement can only be fostered when stakeholders understand its value. This study assessed researchers’ perceptions of the meaning and value of patient engagement in research within a Canadian cardiovascular research network. In doing so, the secondary aim was to inform the development of a structured patient engagement initiative by identifying potential challenges and related mitigation strategies.
Methods: We employed a multi-method strategy involving electronic surveys and semi-structured telephone interviews with network research scientists across Canada. Interview data were analyzed using thematic and content analysis. Survey data were analyzed using descriptive statistics.
Results: Thirty-eight electronic surveys (response rate =33%) and 16 interviews were completed with network members. Some participants were uncertain about the meaning and value of patient engagement. While voicing guarded support, four challenges relating to patient engagement were identified from the interviews: 1) identification of representative and appropriate patients, 2) uncertainty about the scope of patients’ roles given concerns about knowledge discrepancies, 3) a perceived lack of evidence of the impact of patient engagement, and 4) the need for education and culture change as a prerequisite for patient engagement. Research scientists were largely concerned that patients untrained in science and tasked with conveying an authentic patient experience and being a conduit for the voices of others might unsettle a traditional model of conducting research.
Conclusion: Concerns about patient involvement in research were related to a lack of clarity about the meaning, process, and impact of involvement. This study highlights the need for education on the meaning of patient engagement, evidence of its impact, and guidance on practical aspects of implementation within this research community.
Keywords: patient oriented research, health policy, medical culture, patient-centered care, stroke
Background
Patient engagement in research is currently a dominant discourse in clinical research settings, driven in part by Canada’s Strategy for Patient-Oriented Research (SPOR) and its vision to shape a sustainable and equitable health care system.1 In 2011, the Canadian Institutes of Health Research (CIHR) SPOR National Steering Committee led the development of a Patient Engagement Framework, based on the understanding of patients as “experts” with unique experiences and knowledge as a result of living with illness and navigating the health care system. It is expected that involving patients in research will improve its relevance and ultimately increase the quality of care.1 Similar initiatives are well under way outside Canada, such as INVOLVE, funded by the National Health Service in the United Kingdom,2 and PCORI, the Patient-Centered Outcomes Research Institute in the United States.3
Over the last 20 years, the international patient engagement movement has represented a collective, policy-oriented drive away from a traditional paternalistic model of health care. This trend is evidenced by the global proliferation of self-management programs, expert–patient shared decision-making initiatives, and participatory action research.4–7 As Karazivan et al suggest, “including patients as full partners in the health care team entails a significant shift in both the medical practice and medical education cultures.”8 But if including patients in the health care team involves a significant culture shift, the engagement of patients in research teams potentially involves an even greater one. Differences in how different types of knowledge are valued, entrenched power relationships,9 and widespread uncertainty about the meaning of patient engagement itself9–11 are challenges that will require a rethinking of the traditional modes of research practice. The full embrace of patient engagement by researchers is also hindered by concerns about tokenism, logistics, and fear of patient bias;6–8 lack of clarity about best practices;8 practical concerns around defining and representing the community whose engagement is sought;10 and a perceived lack of evidence of impact.12,13 This work sought to build on these insights while also exploring the link between the meaning of and value attributed to the concept of patient engagement in research and researchers’ perception of the challenges and barriers associated with it, of which there is little documentation in the literature.
Although few quantitative studies that measure the impact of patient engagement exist, three syntheses point to qualitative research exploring the impact of patient engagement in research.13–15 They include studies demonstrating that in addition to encouraging equity, patient engagement has improved study outcome selection; helped shape research questions; led to potentially higher rates of participant recruitment and retention; increased the quality, credibility, and applicability of evidence; developed trust between researchers and service users; and facilitated knowledge translation. Yet because of concerns about the quality of evidence and the lack of quantitative, measurable data, all three reviews suggest that the overall impact of patient engagement remains unclear.
Under SPOR, “the patient perspective is integrated into every step of the research process including the development of research questions, defining research objectives, data collection and evaluation,” with patients variously involved, from full membership in research teams to more limited, knowledge-specific ways.1
To realize SPOR goals, the Canadian Stroke Intervention Network (C-SPIN) moved to develop a patient engagement strategy in 2014. C-SPIN is a national multidisciplinary network of research scientists seeking to reduce atrial fibrillation (AF)-related stroke by sharing expertise, resources, and research. The C-SPIN collaboration has involved the design and initiation of eight randomized controlled trials aimed at preventing strokes due to embolic events primarily associated with AF and evaluating innovative strategies to increase uptake of stroke prevention interventions. Involvement in this research would be particularly appropriate for patients and families given that there are over 50,000 strokes each year, with AF being the cause of 15% of strokes overall.16 However, as indicated by CIHR, meaningful patient engagement can only be fostered in a climate where health care professionals “understand the value of patient involvement and patients see the value of these interactions.”1 Therefore, the aim of this study was to assess the perceptions of patient engagement in research across the C-SPIN network to aid in the development of a structured patient engagement initiative and identify potential barriers and facilitators to implementation.
Methods
Following ethics approval from the Hamilton Integrated Research Ethics Board (HiREB #15-244), we employed a multi-method approach over a 9-month period in 2015 using semi-structured telephone interviews and an electronic survey with consenting C-SPIN members. Qualitative methods were used to explore in depth the meanings given to the concept of patient engagement, while an electronic survey was used to understand the extent of the acceptance and resistance to it. Both the approaches provided participants with a standard definition of patient engagement in the context of SPOR and a definition of “patient” as an overarching term that includes individuals with personal experience with a health issue (for C-SPIN, this was AF, stroke, or cardiovascular disease). The definition of patient also included informal caregivers, family, and friends with similar experiential knowledge of AF.
Semi-structured telephone interviews
We invited network member investigators to participate in semi-structured 15- to 45-minute telephone interviews, guided by the SPOR Patient Engagement Framework and informed by some content used previously by one of the coauthors (JA) in a related grant (CIHR, HRA126902) (Figure S1). The interview guide was revised once adding demographic items and rewording two questions to enhance clarity. Interviews were conducted individually by the patient engagement leads of C-SPIN (SC and AD). Interview questions solicited participants’ understanding of patient engagement, perceptions of its value, and facilitators and challenges. Participants were chosen from a purposeful sample of C-SPIN research scientists/members spanning early, mid-, and senior career trajectories.
Interviews were recorded, transcribed, anonymized, and analyzed with key categories iteratively identified and organized using NVivo 10. Transcripts were read numerous times by GE, a cultural anthropologist, and SC, a nurse scientist, in consultation with each other, to develop a holistic sense of the data, and open codes were identified interpretively and iteratively based on both the prevalence of a concept and its potential to enrich the emerging data pool. Through this process, we “treat[ed] research methods as living entities,”17 drawing on insights from both thematic and content analysis to best account for our data. Inductive analysis was conducted with codes emerging from the data rather than a preexisting coding scheme.18,19 In addition, two C-SPIN patient partners reviewed a draft of the manuscript and provided feedback.
Electronic surveys
Electronic surveys paralleling the semi-structured interview guide questions were delivered to 115 network members including stakeholder partners (Figure S2). The survey included five closed-ended questions, two open-ended questions, and demographics. Survey data were collected using Research Electronic Data Capture (REDCap) and exported to the Statistical Package for the Social Sciences (SPSS). Quantitative data were analyzed using descriptive statistics where continuous variables were summarized using measures of central tendency and categorical variables using percentages and frequencies. Open-ended survey questions were analyzed using content analysis.
Results
Semi-structured interviews
Twenty-three C-SPIN investigator members consented to participate in the semi-structured interviews, 17 interviews were scheduled, and 16 completed (20% female). The final sample was based purely on the response rates from the C-SPIN members who consented. Although scheduled, 7 interviews were not completed because of 1) time constraints (of the participants’ clinical schedule) and 2) participant schedule changes. Three attempts were made to reschedule the interview, but the participants did not complete the electronic survey.
The majority of interviews (9) were conducted with cardiologists (including electrophysiologists) and also with two neurologists, a pharmacist, a social scientist, an internist, a clinical epidemiologist, a family physician, research trainees, a C-SPIN external advisory committee member, and 2 patient partners. Participants’ professional work experience ranged from 2 to 44 years, with a mean of 16 years (Table 1). With the exception of one participant in the United States, participants were based in Canada across four provinces.
  | Table 1 Interview participant characteristics |
Electronic surveys
The electronic survey response rate was 33%, with 38 electronic surveys fully completed. Survey participants represented a similar range of professional fields as interviewees. Whereas many interviewees and survey participants were mid- to late career researchers, others were early career professionals.
Understanding and valuing patient engagement
By contrasting electronic survey results with interviews, we revealed differences in how participants understood and described their perceptions of patient engagement in research. From the survey results, it was found that when participants were asked if they understood the meaning of patient engagement, 32 of 38 (84%) said they did (Figure 1). However, the narrative content of the interviews revealed a greater degree of indeterminacy in respondents’ understanding of patient engagement, which then informed perceptions of its value. Interview participants fell along a continuum, with one half seeing value in patient engagement despite voicing concerns about it and the other half seeing the value of patient engagement as overshadowed by concerns surrounding process and desirability.
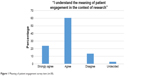  | Figure 1 Meaning of patient engagement survey item (n=38). |
Those who espoused a more holistic understanding of patient engagement (eg, thinking of patients as partners in research, involved in all aspects of the research process) were more likely to confer value to patient engagement, even though they too critiqued the concept. “I think it’s getting a different perspective on value from a societal measure of what we’re doing in a very focused academic environment,” said one participant, who also worried about the education patients would require to understand the research process [Participant O]. Those who were more negative about the concept also tended to know less about it or have a narrower definition of the term. “I’ve heard so little about [patient engagement] and I’ve read so little about it; I’m going to have to invent it as we go along,” said another, who claimed to be “skeptical,” voicing concerns about the challenge of identifying a representative patient and the lack of an established “curriculum” to guide patient engagement training [Participant F].
Both the electronic surveys (Figures 1 and 2) and the interviews indicated that patient engagement was valued because patients could identify research priorities, help with knowledge translation of findings, and provide a different perspective of value. Participants thought this would lend research legitimacy, relevance, and meaning while also balancing power and leading to the democratization of science, making it “very difficult to maintain that very sort of paternalistic approach that doctor knows best” [Participant H].
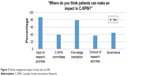  | Figure 2 Patient engagement impact survey item (n=38). |
Approximately half of all participants had been introduced to the concept of patient engagement within the last 2 years (Table 1). Yet patient engagement fostered a sense of uncertainty, even among those who claimed that they are “already doing it” and spoke about it in terms similar in scope to that forwarded by CIHR:
I think it means involving patients at multiple levels in the process of choosing research topics, designing research studies, and also potentially analyzing results and translating the results into new knowledge.… I’m really not sure…. I don’t know a lot about it [Participant B].
Concerns about patient engagement
The survey results indicated that the most frequently cited concern was a perceived lack of knowledge about research among patients, followed by the representativeness of patients and the challenge of selecting appropriate patients. Other challenges included researchers’ resistance to patient engagement, practical concerns such as funding and transport for patients, the difficulty of finding a common language, the need for role clarity and evaluation of patient engagement activities, the danger of tokenism, and the possibility of intimidated patients (Table 2).
  | Table 2 Survey – benefits and challenges of patient engagement |
Concerns raised by interview participants about patient engagement related to four challenges: 1) patient selection – who would be chosen? 2) role clarification – what would be the scope of patient engagement? 3) lack of evidence – why engage in patient engagement given the lack of evidence demonstrating its impact? and 4) the need for education (for patients and researchers) and culture change as a prerequisite for patient engagement.
Patient partner selection
Many participants were uncertain about how a patient engagement strategy may be practically implemented. They wondered about whom to include and how to include them meaningfully:
… Is it the smartest, the richest, the one with the most time on their hands, the one that’s most articulate, the one that’s the sickest because they had most interaction with the healthcare system; is it going to be men, women, young, old, well educated, less well educated…. How do we come up with a fair, reasonable process for finding those patients? [Participant F]
Researchers also worried about what constituted a “good” patient. An appropriate candidate, most agreed, would have to be a conduit for the voices of other patients, but there were inherent concerns about one patient representing others without simultaneously institutionalizing and professionalizing their roles. It seemed that a paradox lay at the heart of patient engagement: the need to retain the authenticity of a patient’s unique experience while simultaneously representing a global disease experience, represented by population-level data yielded by trials and observation studies. Furthermore, the patients who would tend to be chosen as likely candidates for patient engagement initiatives could not be “typical” or “representative” in many ways because of the need for them to be articulate, understand research, and engage with other health care professionals and other patients:
… when we’ve been asked to try to identify patient advocates to sit on this committee or that committee, we tend to look for people that are exceptional examples of people with the disease, not garden variety examples of people with the disease … and I’m not sure that that’s giving us what we want in patient engagement. [Participant P]
Research scientists also noted that practical concerns relating to time and money could inhibit participation from certain socioeconomic groups.
Role clarification
Many understood scientist and patient as occupying two different worlds, debatably equal but unequivocally separate. There was keen appreciation of stark differences in knowledge and power between patient and researcher. One spoke of “a knowledge gap,” “a power differential, like a teacher/student differential” [Participant G]. “Does the patient really need to read the whole research proposal and comments?” wondered another [Participant E]. Yet another suggested that patients “would not have sufficient knowledge to be able to choose the priorities for research….” [Participant D]. They may be able to provide “important elements of a given area,” but they should not “be assessing the science or the methodology” [Participant N]. Others voiced the need for “a bunch of education” for patients [Participant O] and for “orient[ing patients] to this world so that they can play a part [as] we have a research speak that nobody else understands” [Participant E].
The need to delimit patient engagement was echoed in survey data, where one respondent suggested that patient-entered data should be “audited against source data” to ensure “accuracy” and “objectivity” as the patient would tend to “provide subjective information”. Another similarly claimed that “the scientific approach of researchers does not work with the patient approach” and that the patient training required would be so significant that “very few patients would qualify for effective input”.
Concerns about the lack of patient knowledge of the research process were linked to concern about a shift in a historically well-established research paradigm. Allowing patients potentially untrained in scientific methods to dabble in research worried many and led to a broader concern about preserving the integrity of science itself.
Lack of evidence
Many participants were concerned about the lack of evidence demonstrating the impact of patient engagement. They wanted to “measure” patient engagement outcomes – a difficult proposition given that it was not clear what these outcomes should be (Participants D and H) or what statistical methods should be used to generate results (Participant K):
We actually don’t have a lot of evidence that it changes research, in what ways, in what situations, what type of patients…. [Participant H]
Furthermore, only certain, familiar modes of “measurement” were deemed appropriate:
… ultimately it’s … going to be descriptive. Whereas knowledge translation, you can measure things, you can do randomized trials…. [Participant D]
Without such familiar, dependable evidence, many respondents felt unable to attribute value to patient engagement. They feared that the interest in patient engagement was the “flavor-of-the-day” [Participant D] or tokenistic “window dressing” [Participant H] and said that researchers engaged in it because “we’re required to do it, not because we know what it is and how to go about it” [Participant P].
Need for culture change
A few participants reflexively identified the need for education and culture change around the concept of patient education for researchers themselves. As one participant put it, a “major barrier is challenge to [a] conventional model and acceptance by [the] research community”, whereas another wondered “how to change researcher culture to be more inclusive and more power sharing/co-creating”.
A few participants also reflexively suggested that health care providers’ hesitance in fully embracing patient engagement sprang from the shift it represented from a familiar and established mode of conducting research:
… there’s been an awful lot of structure and process put in place to help support patients…, but in fact I think it’s almost to support the researchers and the health care providers to have a level of comfort that it’s okay to invite people in. [Participant C]
It is noteworthy that the survey included two patient partners whose concerns about patient engagement echoed those of health professionals. When asked to check boxes indicating if patients could make an impact in a range of C-SPIN activities, from research priority setting to governance, only 3 of a possible 10 boxes were checked by the patients themselves. As another participant indicated, there is perhaps a need for “training for patients so they understand the research process [and] training for researchers so they understand how to meaningfully engage patients”.
Strengths and limitations
This study aimed to assess researchers’ perceptions of the meaning and value of patient engagement in research within the context of a Canadian cardiovascular research network. Our targeted recruitment of network member participants assisted our team to achieve our aim, and the knowledge gleaned from this work will inform further development of our patient engagement strategy. Although the survey response rate was low, limiting generalizability to similar networks, our multi-method approach to data collection allowed for greater reach across the network. While the ratio of cardiologists included in our interviews echoes the make-up of C-SPIN as a research network, and is therefore representatives of perspectives within this group, it may not be representative of researchers at large.
To improve the trustworthiness of the findings, several strategies were applied. The inclusion of qualitative interviews helped corroborate and provide further insight into survey responses through participants own narratives. Our sample included a range of participants in terms of years in practice, profession, and role in the network. Finally, the background and experience of the investigative team with this subject matter offers credibility to the interpretation of our findings.
Conclusion
Despite the lack of knowledge about how to best implement and realize meaningful patient engagement, the value that most saw in the overall goal of patient engagement must be acknowledged. Participants valued patient engagement because they thought patients could assist in selecting research activities, lend research relevance and legitimacy, and balance power by unsettling a traditionally paternalistic model of health care. However, few were prepared to embrace patient engagement unreservedly.
A key concern of participants related to patient selection: who would qualify as an “appropriate patient,” and how could researchers ensure the democracy of the selection process? These concerns reflected a dilemma over how to negotiate the “crisis of representation,”20 the problem of a possibly atypical patient speaking for others, with the potential for misrepresentation and loss of experiential authenticity. However, as Staniszewska et al have reminded us, in this context, the patient is an active collaborator and member of the research team, not a subject of data collection, and as such “would not necessarily be expected to provide a representative view of all patients, in the same way as a researcher would not be expected to provide a representative view of all researchers within a collaborative team.”21 As such, they suggest along with Hanley et al that “it might be helpful to think about seeking [patient] perspectives rather than [patient] representatives.”22
A related concern had to do with the scope of patients’ roles in research given perceived stark differences in knowledge and power between patient and researcher. As outlined by SPOR, although patients have the option of participating in research in circumscribed ways (eg, in developing research questions or as knowledge brokers), patients with the appropriate “readiness” may also contribute as fully fledged members of research teams. Researchers are encouraged to ensure that “the patient perspective is integrated into every step of the research process,”23 suggesting a significant reorienting of research, with patients’ perspectives potentially having equal weight to those of the researchers. As a few C-SPIN researchers pointed out, this represented a new way of conducting research that could potentially be unsettling. Their concerns about patients’ inability to understand, interpret, or even pay attention to scientific information have been voiced elsewhere.24,25
Finally, many wondered if patient engagement was justified given a perceived lack of evidence demonstrating impact. Their need for outcomes that could be “measured” in specific ways revealed a strong positivistic bias that displayed unfamiliarity with the existing, although limited, qualitative research noted above that documents the impacts of patient engagement as experienced by patients and researchers – research that CIHR could perhaps highlight in making an argument for patient engagement, quelling concerns that it is merely the flavor of the day.
Underpinning these concerns was uncertainty about what patient engagement actually means. This could be seen not just in the wide range of meanings it had for C-SPIN research scientists but also in the lack of clarity about the concept for individual respondents. The little available scholarship on the acceptability of patient engagement in research has similarly noted the varied meaning of patient engagement for different stakeholders;26–28 differences in understanding that have been shown to be linked to stakeholder positionality and value accorded to the concept.29 Indeed, a key observation we take from this study is the need for conceptual clarity. The results can be used to 1) ensure that research scientists are educated on the conceptual meaning and scope of patient engagement, 2) offer guidance to select patient partners with requisite knowledge and skills to engage in targeted roles, 3) facilitate access to resources and tools enabling the operationalization of patient engagement strategies, and 4) ensure that new evidence demonstrating the impact of patient engagement is disseminated within the research community.
For patient engagement to be seriously adopted and strategies developed, researchers must also be convinced that 1) patients’ knowledge and potential to be involved in research are commensurate with (although different from) those of researchers and 2) patient engagement has a meaningful impact on research outcomes. The former requires a rethinking of well-entrenched modes of producing research that has traditionally privileged the scientific knowledge and expertise of the researcher, and the latter requires researchers to rethink a traditionally positivistic mode of producing research and take seriously the qualitatively reported outcomes of patient engagement that do exist. Both entail a significant culture shift, a rethinking of how we conceptualize scientific epistemology itself.
Acknowledgments
We are grateful to Angie Djuric and Kimberly Begley, who assisted with the scheduling and conducting of the interviews; to Katherine Allan, who assisted with analysis of our survey data; and to [F] David and [A] Annette, who provided feedback on the manuscript in their capacity as patient partners at C-SPIN. Dr Healey is supported by a Heart and Stroke Foundation of Ontario Mid-Career Award (MC7450).
Disclosure
The authors report no conflicts of interest in this work.
References
Canadian Institutes of Health Research. Canada’s Strategy for Patient-Oriented Research. 2011:i–33. Available from: http://cihr-irsc.gc.ca/e/41204.html. Accessed July 2016. | ||
National Institute for Health Research. Involve 2017. Available from: http://www.invo.org.uk/. Accessed July 20, 2016. | ||
PCORI. Patient-Centered Outcomes Research Institute 2011–2017. Available from: http://www.pcori.org/. Accessed July 20, 2016. | ||
Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. | ||
Donaldson L. Expert patients usher in a new era of opportunity for the NHS. BMJ. 2003;326:1279. | ||
Entwistle VA, Renfrew MJ, Yearley S, Forrester J, Lamont T. Lay perspectives: advantages for health research. BMJ. 1998;316:463–466. | ||
Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Commun Health. 2006;60:854–857. | ||
Karazivan P, Dumez V, Flora L, et al. The patient-as-partner approach in health care: a conceptual framework for a necessary transition. Acad Med. 2015;90:437–441. | ||
Wallerstein N. Challenges for the field in overcoming disparities through a CBPR approach. Ethn Dis. 2006;16(1 Suppl 1):S146–S148. | ||
Chambers R, O’Brien LM, Linnell S, Sharp S. Why don’t health researchers report consumer involvement? Qual Prim Care. 2004;12:151–157. | ||
Lough S. Need to define patient engagement in research. Can Med Assoc J. 2015;187:E385–E386. | ||
Legare F, Boivin A, van der Weijden T, et al. Patient and public involvement in clinical practice guidelines: a knowledge synthesis of existing programs. Med Decis Making. 2011;31:E45–E74. | ||
Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14:89. | ||
Esmail L, Moore E, Rein A. Evaluating patient and stakeholder engagement in research: moving from theory to practice. J Comp Eff Res.2015;4:133–145. | ||
Brett J, Staniszewska S, Mockford C, Herron-Marx S, Tysall C, Suleman R. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient. 2014;7:387–395. | ||
Heart and Stroke Foundation. Atrial fibrillation – be pulse aware. 2014. Available from: https://www.heartandstroke.ca/search-results-page?q=pulse+aware. Accessed July 20, 2016. | ||
Sandelowski M. What’s in a name? Qualitative description revisited. Res Nurs Health. 2010;33:77–84. | ||
Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. | ||
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:79–87. | ||
Marcus GE, Fischer MMJ. Anthropology as Cultural Critque: An experimental Moment in the Human Sciences. Chicago: University of Chicago Press; 1999. | ||
Staniszewska S, Haywood K, Brett J, Tutton L. Patient and public involvement in patient reported outcome measures: evolution not revolution. Patient. 2012;5:75–77. | ||
Hanley B, Truesdale A, King A, Elbourne D, Chalmers I. Involving consumers in designing, conducting, and interpreting randomised controlled trials: questionnaire survey. BMJ. 2001;322:519–523. | ||
Canadian Institutes of Health Research. Strategy for Patient-Oriented Research (SPOR) – Patient Engagement Framework. 2014. Available from: http://www.cihr-irsc.gc.ca/e/48413.html#a13. Accessed July 20, 2016. | ||
Groene O. Patient and public involvement in developing patient-reported outcome measures: indispensable, desirable, challenging. The Patient. 2012;5:75–77. | ||
Nease RF, Frazee SG, Zarin L, Miller SB. Choice architecture is a better strategy than engaging patient to spur behavior change. Health Affairs. 2013;32:242–249. | ||
Barello S, Graffigna G, Vegni E, Bosio AC. The challenges of conceptualizing patient engagement in health care: a lexicographic literature review. J Participat Med.2014;6:e9. | ||
Bellows M, Burns KK, Jackson K, Surgeoner B, Gallivan J. Meaningful and effective patient engagement: what matters most to stakeholders. Patient Exp J. 2015;2:18–28. | ||
Khodyakov D, Stockdale SE, Smith N, Booth M, Altman L, Rubenstein LV. Patient engagement in the process of planning and designing outpatient care improvements at the Veterans Administration Health-care System: findings from online expert panel. Health Expect. 2017;20:130–145. | ||
Boaz A, Biri D, McKevitt C. Rethinking the relationship between science and society: has there been a shift in attitudes to patient and public involvement and public engagement in science in the United Kingdom? Health Expect. 2016;19:592–601. |
Supplementary materials
  | Figure S1 Patient engagement prevention network (C-SPIN) – interview guide. |
  | Figure S2 Electronic survey patient engagement. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
