Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Psychiatric comorbidities in patients with intentional methanol intoxication
Authors Yang WS, Yen TH , Juang YY, Lee SH, Wang BH, Lee CP
Received 31 October 2018
Accepted for publication 4 January 2019
Published 31 January 2019 Volume 2019:15 Pages 397—402
DOI https://doi.org/10.2147/NDT.S192943
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Wei-Sheng Yang,1,2 Tzung-Hai Yen,2,3 Yeong-Yuh Juang,4 Shwu-Hua Lee,1,2 Bi-Hwa Wang,5 Chin-Pang Lee1,2
1Department of Psychiatry, Chang Gung Memorial Hospital, Linkou, Taoyuan, Taiwan; 2School of Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan; 3Department of Nephrology and Clinical Poison Center, Chang Gung Memorial Hospital, Linkou, Taiwan; 4Department of Psychiatry, Koo Foundation Sun Yat-Sen Cancer Center, Taipei, Taiwan; 5School of Nursing, College of Medicine, Chang Gung University, Taoyuan, Taiwan
Background: Intentional methanol intoxication (IMI) is an emerging public health issue in Asian countries, but few data are available in the literature on underlying psychiatric comorbidities in these suicide attempters.
Patients and methods: We conducted a retrospective chart review on patients with methanol intoxication (MI) treated at Chang-Gung Memorial Hospital, Linkou, Taiwan during 2000–2016. Of the 56 cases of documented MI, 16 were IMI. Baseline demographic, clinical, laboratory, psychiatric diagnoses, and mortality data were collected and analyzed.
Results: Patient group with IMI had more females (62.5% vs 7.5%, P=0.000), less alcohol consumption (33.3% vs 92.5%, P=0.000), and less smoking (40.0% vs 79.5%, P=0.009), but higher past psychiatric disease (73.3% vs 10.0%, P=0.000) and past suicide attempts (81.1% vs 2.5%, P=0.000) than patient group with unintentional MI (UMI). Pesticides (50.0%) comprised the most common source used for suicide, followed by industrial methanol (37.5%). There was no significant difference in mortality rates between these two group (25.0% vs 22.5%, P=0.548). Twelve (75.0%) survivors of IMI were referred to a psychiatric consultation-liaison team, and depressive disorder (58.3%) and adjustment disorder (25.0%) were common.
Conclusion: There is a female predominance and a high prevalence of psychiatric comorbidities, namely depression and adjustment disorder in patients with IMI. Besides, alcohol consumption is a prevalent but not adequately treated condition in UMI group.
Keywords: alcohol, suicide, methanol intoxication, pesticide, depression
Introduction
Suicide accounts for 1.4% of all deaths worldwide.1 According to the WHO, it is estimated that nearly 800,000 people die from suicide. In Taiwan, suicide ranked as the 12th leading cause of death with a rate of 12.3 per 100,000 people in 2016,2 and the leading suicide methods were hanging, charcoal burning, and pesticide intoxication;3 in contrast, intentional methanol intoxication (IMI) remains uncommon. Methanol is available as a common solvent in many products (eg, antifreeze, paint, cleaner, nail polish, and pesticides) or as a raw industrial material, but it could also be present in contaminated alcohol causing mass intoxications.4–6 Ingestion of small amount of methanol leads to severe acidosis, visual loss, or even death with mortality as high as 29% in an outbreak in Kenya in 2014,7 and thus, IMI is considered to be a method of high lethality. There were only isolated case reports discussing patients who took to MI intentionally,8,9 but with little description on psychiatric comorbidity; most of the current studies take those intoxicated patients as a whole. Thus, in the present study, we aimed to survey psychiatric diagnoses among patients with IMI, and identify distinct characteristics of patients with IMI compared to those with unintentional MI (UMI).
Patients and methods
Ethical statement
This study complies with the guidelines of the Declaration of Helsinki and was approved by the Institution Review Board (IRB) of Chang Gung Memorial Hospital, Linkou (IRB number: 201800245B0). The IRB approved and waived the need for specific informed consent from the patients because this was a retrospective study based on case research or cases treated or diagnosed by clinical routines without enrollment of HIV positive cases. All primary data were collected according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines and confidentiality of each patient data was kept.
Patients
The Chang Gung Memorial Hospital, Linkou, is a tertiary referral medical center in northern Taiwan, and there are toxicology specialists in both the Departments of Medical Emergency and Nephrology. Between 2000 and 2016, a total of 59 patients were admitted to the ward of Department of Nephrology owing to methanol intoxication (MI) and all of their medical charts were systemically reviewed by one of the authors (Yang WS). If MI was highly suspected from history of exposure to methanol, physical symptoms, marked increased serum osmolal gap, and metabolic acidosis, then emergency treatments such as either ethanol ingestion (19 patients), hemodialysis (43 patients), or both were done at the emergency department. Fomepizole was not available in our hospital and, therefore, was not included in our standard treatment. The detail of the detoxification protocols is described elsewhere.10 All the laboratory data were collected on admission by blood sampling based on clinical evaluation. Concentration of serum methanol was detected by gas chromatography with limits of detection at <0.15 mg/dL and toxic level at >20.00 mg/dL. Among 59 patients with MI, three (5.1%) were unable to be classified as intentional or unintentional and, therefore, they were excluded. For the remaining 56 patients, demographic data and clinical characteristics were documented. Among them, 16 (28.6%) patients were considered as having IMI and four (25%) in the IMI group died. The remaining 12 patients were referred to a consultation-liaison psychiatric evaluation after stabilized physical condition. Board-certified psychiatrists conducted a face-to-face diagnostic interview and collateral information was collected to ascertain the validity of suicidal intention and reasons for suicide. Final psychiatric diagnoses were made according to the Diagnostic and Statistical Manual of Mental Disorder (DSM)-IV and DSM-5 criteria. One of the authors (Juang YY), a senior psychiatrist, supervised all the referrals to the consultation-liaison service as well as final psychiatric diagnoses. After initial chart review of all the 56 patients enrolled for MI, one of the authors, Yen TH, independently reviewed these charts in order to confirm data integrity.
Statistical analysis
Continuous variables were expressed as means, and categorical variables as numbers and percentages. We used independent Student’s t-test for quantitative variables and chi-square or Fisher’s exact test for categorical variables. Missing data were ignored. All probability levels of P<0.05 were considered significant. We used SPSS statistics 24.0 (IBM Corporation, Armonk, NY, USA) for all the statistical analyses of our study.
Results
Among 56 patients enrolled, a significant gender difference existed between the IMI and UMI groups. The female-to-male ratio was 1.67 for the IMI group, while it was 0.08 for UMI group (P<0.001). There were significantly more patients with history of alcohol consumption and smoking in the UMI group, while past psychiatric disorders and suicide attempts were more prevalent in the IMI group. With regard to past psychiatric diagnoses in the IMI group, depression accounted for the major part (81.8%, n=9), including five patients with major depressive disorder, and rest had bipolar disorder (9.1%, n=1) and heroin use disorder (9.1%, n=1). Comorbidities were noted in patients with depression, with one alcohol use disorder patient with sustained remission and one neurocognitive disorder patient (clinical dementia rating =0.5). In contrast, only four (10%) patients in the UMI group received past psychiatric diagnoses with depression being the most prevalent diagnosis (75%, n=3). All demographic and clinical characteristics are summarized in Table 1.
Oral intake was the most common route of methanol exposure (89.3%, n=50); but two patients, one of whom was in the IMI group, were exposed through intramuscular/intravascular injection, and there were four patients with unconfirmed route of exposure. Regarding sources of methanol exposure, commercial alcohol and moonshine were the major source in the UMI group, while in the IMI group pesticides were the leading source (50%, n=8), followed by industrial methanol (37.5%, n=6). Results are illustrated in Table 2. Complex suicide was noted in a third of patients of IMI group with methods combining drinking pesticides or industrial methanol with either charcoal burning, wrist cutting, or overdosing with benzodiazepines or other psychotropics. In triage, patients of UMI group had significantly higher pulse and respiratory rate (pulse rate: t43=−2.624, P=0.012; respiratory rate: t43=−2.046, P=0.047). Blood test revealed significantly higher serum methanol level in the IMI group (t45=2.6, P=0.012) and higher serum lactate in the UMI group (t14.3=−3.9, P=0.002), but there were no differences in the blood ethanol level, pH, and osmolality between the two groups. On the subject of clinical outcome, the overall mortality was 23.3%, and along with morbidity and other clinical courses, including rate and duration of intensive care unit (ICU) stay and total days of hospitalization, there was no difference in both groups. Details are shown in Table 3.
  | Table 3 Clinical outcomes of patients with MI (n=56) |
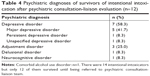
Psychiatric consultations were arranged for 12 (75.0%) patients in the IMI group, and the diagnoses are presented in Table 4. Depressive disorder was the most commonly encountered diagnosis (n=7, 58.3%) with major depressive disorder accounting for the majority, followed by adjustment disorder (n=3, 25.0%). Besides, among the four mortalities, two had past history of depression and one had heroin use disorder. In contrast to the high percentage of psychiatric consultation in the IMI group, only two patients in the UMI group received psychiatric interview and one of them was diagnosed with major depressive disorder. However, most of the patients in the UMI group had a record of habitual alcohol consumption.
Discussion
In recent years, early detection and management of MI in emergency departments have raised much attention, but psychiatric comorbidity of methanol intoxicated patients, whether intentional or unintentional, is not yet fully investigated. To our knowledge, our study is the first to specifically address the psychiatric comorbidities in patients having IMI. The main findings of our study are that the patients in IMI group were predominantly female, having past major psychiatric diagnoses and previous suicidal attempts, all of which were risk factors that had been mentioned in previous studies,11,12 and the most common diagnoses were depressive and adjustment disorders. Though differing in vital signs and serum methanol level in initial presentation, the morbidity and mortality of both groups were similar. Despite having small number of included patients, our data is still representative in northern Taiwan across 16 years.
Sources of MI
In a report of American Association of Poison Control Centers’ National Poison Data System, MI via ingestion remained the most common route of exposure (63.3%) during 2000–2013,13 which was consistent with our study, but Givens et al indicated inhalation as an emerging route of methanol exposure,14 which is not yet encountered in our study. In contrast with windshield cleaner and carburetor cleaner being the most common sources in the USA,14 commercial alcohol and moonshine were the primary sources in the UMI group and pesticide and industrial methanol were the primary sources in the IMI group in Taiwan (64.3%) based on our results. Strictly speaking, half of the patients originally attempted suicides by drinking pesticides but ended up being methanol intoxicated. Although some pesticides, such as carbamates and triazoles, are less toxic, the additive methanol caused morbidity and mortality. Our study is in line with studies from Korea, which brought the toxicity of additives or solvents in pesticides to our attention.15–17 The dissimilarity in sources of methanol worldwide is important for clinical practice and public health. In Asian countries, physicians should consider MI in case of pesticide poisoning and the toxicity of additives, especially methanol, should be tagged and access to methanol-containing pesticide should be restricted through legislative regulation for suicide prevention. Furthermore, the risk of MI in contaminated alcohol should be emphasized though public education for prevention of accidental intoxication.
Gender
The result of our study demonstrated a different female-to-male ratio between IMI and UMI groups. A male predominance in UMI group was compatible with past reports worldwide.4–7,13,14,18 One possible explanation is that the majority (74%) of UMI patients included in our study was composed of habitual drinkers, who were mostly males as a previous study disclosed.19 On the contrary, females accounted for a greater proportion in patients of IMI. Given that in MI, poisoning by substance other than drug and complex methods are considered lethal, our result was contrary to past concept that females are prone to suicide attempts by nonlethal methods.20 Considering that suicide is a process, factors other than gender should be taken into account in explaining this result.
Past and current psychiatric diagnoses
Compared to the UMI group, patients in the IMI group were less involved in alcohol consumption (P<0.001) or smoking (P=0.009), but they were more likely to have past major psychiatric diagnoses (depression or bipolar disorder) and previous suicidal attempts, which are risk factors for suicide that had been confirmed in previous studies.11,12 Among those patients of the IMI group who received psychiatric interview, depressive disorder, especially, major depressive disorder, was the leading diagnosis, which was in agreement with previous studies in Taiwan.21,22 Therefore, early detection and treatment of depression and identification of previous suicide attempt are important for suicide prevention. Additionally, 75% of patients in intentional intoxicated group received psychiatric consultation, but, in contrast, only two unintentionally intoxicated patients received psychiatric consultation despite most of the UMI patients being habitual alcohol users. This result sheds light on the inadequacy of the management of UMI patients.
Medical presentation and clinical outcomes
Both of the study groups showed acidosis, increased lactate level, and hyperosmolarity, but methanol level was significantly higher in the IMI group (82.1±77.7 vs 21.3±73.0 mg/dL, t45=2.610, P=0.012), while the lactate level was significantly higher in the UMI group (47.0±32.2 vs 159.5±92.6 mg/dL, t14.323=−3.906, P=0.002). This intriguing result indicated a more severe metabolic acidosis in UMI group, which could be explained by differences in timing of medical presentation. The patients of IMI were often brought to emergent department soon after exposure to the causative agent, therefore, serum methanol was sampled before it was metabolized to formaldehyde. On the contrary, in UMI cases, medical care could be delayed for days because of the inability to describe that exact time of exposure and delayed occurrence of intoxicated symptoms resulted from concomitant alcohol ingestion. Therefore, methanol level became low, tissue hypoxia occurred, and lactate level became high. In a systemic review, Kostic and Dart described a negative correlation between serum methanol level with delayed medical care,23 which in combination with respiratory compensation presented with the vital signs at triage, demonstrated different intentions of getting intoxicated. Despite different initial level of serum methanol level, there was no difference in the percentage of ICU admission, days of ICU stay, or total hospitalization days in both the groups, and even the mortality rate was identical. The overall mortality rate of total intoxicated patients in our study was 23.3%, which is identical to previous reports in consideration of limited access of fomepizole in Taiwan.24
Limitation
Several limitations should be noted in this study. First, this was a retrospective study and thus it inherited imitations natural to it. Second, samples in the present study were too small and so clinical implications and generalizations should be approached with caution. However, in consideration that methanol itself was uncommon for toxic poisoning, and according to Nationwide Poisoning Database of Taiwan, only 621 cases of MI were identified across 14 years.25 The sample size of the present study approached one-tenth of all cases of MI, and as a tertiary referral center where patients of MI were commonly referred to due to its high toxicity, our samples should be representative of northern Taiwan. Moreover, the information of each patient was documented in detail, which could hardly be achieved in a registry-based study. However, included samples were restricted to one hospital and those who could be transferred to our hospital. Those who expired or whose symptoms were not severe enough to be detected were automatically excluded. Third, although all psychiatric diagnoses were made based on DSM-IV or DSM-5 after interview by board-certified psychiatrists, we did not use any instrument to confirm the diagnoses or standardize the inter-rater reliability. However, the accuracy of diagnoses was supervised by the doctor in charge of the consultation-liaison team (Juang YY). Also, some would argue that physical condition in acute intoxication status could bias the validity of diagnoses and, indeed, some of the intentional intoxicated cases came with altered consciousness. Nevertheless, most of the intoxicated patients got admitted for several days, which provided us enough time span to conduct a routine consultation to validate previous diagnosis. Based on aforementioned reasons, the inter-rater reliability and validity of diagnosis should be considered acceptable. Fourth, the inconsistency of psychiatric diagnosis between the consultation-liaison psychiatric team and Outpatient Department of Psychiatry was not examined, and long-term follow-up of patients initially diagnosed with adjustment disorder could not be achieved, which resulted from low rate of follow-up. As a result, in light of all the limitations, a prospective study with proper sampling, adequately controlled valid consultation, and sufficient follow-up duration would provide further insight into IMI and its psychiatric comorbidity.
Conclusion
Based on our results, depression remains the major psychiatric comorbidity in the IMI group, therefore, being aware of depressive symptoms should be emphasized through public education, and primary care physicians should be equipped with adequate knowledge of identifying depressive patients in daily practice and provide them with appropriate treatment or expertise transfer. Besides, pesticide has become the major source of IMI. Hence, a proper legislative regulation should be warranted, and physicians should be aware that MI could come from substances other than industrial methanol or contaminated alcohol. Additionally, our study sheds light for physicians and psychiatrists on detection and treatment of comorbid alcohol use disorder in UMI patients.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Suicide data. 2016. Available from: https://www.who.int/mental_health/prevention/suicide/suicideprevent/en/. Accessed December 20, 2018. | ||
Taiwan Society of Suicidology. Available from: http://tspc.tw/tspc/portal/know/index.jsp?type=2. Accessed December 20, 2018. Chinese. | ||
Lin JJ, Chang SS, Lu TH, Th L. The leading methods of suicide in Taiwan, 2002–2008. BMC Public Health. 2010;10:480. | ||
Hovda KE, Hunderi OH, Tafjord AB, Dunlop O, Rudberg N, Jacobsen D. Methanol outbreak in Norway 2002–2004: epidemiology, clinical features and prognostic signs. J Intern Med. 2005;258(2):181–190. | ||
Zakharov S, Pelclova D, Urban P, et al. Czech mass methanol outbreak 2012: epidemiology, challenges and clinical features. Clin Toxicol. 2014;52(10):1013–1024. | ||
Hassanian-Moghaddam H, Nikfarjam A, Mirafzal A, et al. Methanol mass poisoning in Iran: role of case finding in outbreak management. J Public Health. 2015;37(2):354–359. | ||
Rostrup M, Edwards JK, Abukalish M, et al. The methanol poisoning outbreaks in Libya 2013 and Kenya 2014. PLoS One. 2016;11(3):e0152676. | ||
Bucaretchi F, de Capitani EM, Madureira PR, Cesconetto DM, Lanaro R, Vieira RJ. Suicide attempt using pure methanol with hospitalization of the patient soon after ingestion: case report. Sao Paulo Med J. 2009;127(2):108–110. | ||
Hsiao P-J, Chen T-Y, Chiu C-C, et al. Delayed high anion gap metabolic acidosis after a suicide attempt: case report. Clinica Chimica Acta. 2014;436:329–331. | ||
Lee CY, Chang EK, Lin JL, et al. Risk factors for mortality in Asian Taiwanese patients with methanol poisoning. Ther Clin Risk Manag. 2014;10:61–67. | ||
Chen W-J, Shyu S-S, Lin G-G, et al. The Predictors of suicidality in previous suicide attempters following case management services. Suicide Life Threat Behav. 2013;33(6):n/a–478. | ||
Zeppegno P, Gramaglia C, Castello LM, et al. Suicide attempts and emergency room psychiatric consultation. BMC Psychiatry. 2015;15(1):13. | ||
Ghannoum M, Hoffman RS, Mowry JB, Lavergne V. Trends in toxic alcohol exposures in the United States from 2000 to 2013: a focus on the use of antidotes and extracorporeal treatments. Semin Dial. 2014;27(4):395–401. | ||
Givens M, Kalbfleisch K, Bryson S. Comparison of methanol exposure routes reported to Texas poison control centers. West J Emerg Med. 2008;9(3):150–153. | ||
Gil HW, Hong JR, Song HY, Hong SY. A case of methanol intoxication caused by methomyl pesticide ingestion. Hum Exp Toxicol. 2012;31(12):1299–1302. | ||
Gil HW, Jeong MH, Park JS, Choi HW, Kim SY, Hong SY. An outbreak of food borne illness due to methomyl pesticide intoxication in Korea. J Korean Med Sci. 2013;28(11):1677–1681. | ||
Lee SH, Park S, Lee JW, et al. The anion gap is a predictive clinical marker for death in patients with acute pesticide intoxication. J Korean Med Sci. 2016;31(7):1150–1159. | ||
Onyekwere N, Nwadiuto I, Maleghemi S, et al. Methanol poisoning in South-South Nigeria: reflections on the outbreak response. J Public Health Afr. 2018;9(1):748. | ||
Erol A, Karpyak VM. Sex and gender-related differences in alcohol use and its consequences: contemporary knowledge and future research considerations. Drug Alcohol Depend. 2015;156:1–13. | ||
Mergl R, Koburger N, Heinrichs K, et al. What are reasons for the large gender differences in the lethality of suicidal acts? An epidemiological analysis in four European countries. PLoS One. 2015;10(7):e0129062. | ||
Lin C, Yen TH, Juang YY, et al. Comorbid psychiatric diagnoses in suicide attempt by charcoal burning: a 10-year study in a general Hospital in Taiwan. Gen Hosp Psychiatry. 2012;34(5):552–556. | ||
Lin C, Yen TH, Juang YY, Lin JL, Lee SH. Psychiatric comorbidity and its impact on mortality in patients who attempted suicide by paraquat poisoning during 2000–2010. PLoS One. 2014;9(11):e112160. | ||
Kostic MA, Dart RC. Rethinking the toxic methanol level. J Toxicol Clin Toxicol. 2003;41(6):793–800. | ||
Beatty L, Green R, Magee K, Zed P. A systematic review of ethanol and fomepizole use in toxic alcohol ingestions. Emergency Medicine International. 2013;2013(6):1–14. | ||
Chung JY, Ho CH, Chen YC, et al. Association between acute methanol poisoning and subsequent mortality: a nationwide study in Taiwan. BMC Public Health. 2018;18(1):985. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.