Back to Journals » Clinical Optometry » Volume 13
Pseudoexfoliation Syndrome and Associated Factors Among Adults at Gondar University Comprehensive Specialized Hospital Tertiary Eye Care and Training Center: A Cross-Sectional Study
Authors Yibekal BT , Adimassu NF , Ayele FA
Received 25 May 2021
Accepted for publication 11 August 2021
Published 24 August 2021 Volume 2021:13 Pages 249—255
DOI https://doi.org/10.2147/OPTO.S321716
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Betelhem Temesgen Yibekal,1 Nebiyat Feleke Adimassu,1 Fisseha Admassu Ayele2
1Department of Optometry, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar City, Ethiopia; 2Department of Ophthalmology, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar City, Ethiopia
Correspondence: Betelhem Temesgen Yibekal Email [email protected]
Background: Pseudoexfoliation syndrome is an age-related disorder characterized by the deposition of a distinct fibrillar extracellular material in various tissues and organs of the body. Glaucoma and cataract are the consistently reported clinical consequences of Pseudoexfoliation syndrome on the eye. This study aimed to estimate the proportion of pseudo-exfoliation syndrome and associated factors in Gondar university comprehensive specialized hospital tertiary eye care and training center.
Methods and Materials: Institution-based cross-sectional study was conducted from January to March 2019 at Gondar university comprehensive specialized hospital tertiary eye care and training center among 295 patients. Consecutive 295 participants aged above 40 years were involved in the study. A structured questionnaire and ocular examination were used to collect the data. Data were entered into EPI-INFO 3.5.1 and exported to SPSS version 20 for analysis. Factors associated with pseudoexfoliation syndrome were ascertained by chi-square and independent t-test. Statistical significance was considered when p-value < 0.05.
Results: A total of 295 adults participated in the study with a response rate of 92.8%. The median (±IQR) age of study respondents was 64(± 9) years and 67.8% were males. The proportion pseudoexfoliation syndrome was 34.6% [95% CI: 29.2– 40.7%]. The mean IOP and mean age were significantly higher among patients with pseudoexfoliation syndrome. Age, sex, high IOP, glaucoma, outdoor work, and rural residence were significantly associated with the proportion of pseudoexfoliation syndrome.
Conclusion: The proportion of pseudoexfoliation syndrome among participants aged ≥ 40 years was high. Age, sex, high IOP, glaucoma, outdoor work, and rural residence were factors having a significant association with the proportion of pseudoexfoliation syndrome.
Keywords: pseudoexfoliation syndrome, Ethiopia, Gondar
Introduction
Pseudoexfoliation syndrome (PXF) is an age-related disorder characterized by the deposition of a distinct fibrillar extracellular material in various tissues and organs of the body.1 Glaucoma and cataract are the most consistently reported clinical consequences of PXF on the eye.
The proportion of PXF has been investigated in different countries and it ranges from 1.5% to 40.9% worldwide.2,3 Literatures show in European countries the proportion is found to be 3.6% to 34.2%,4,5 in Asian countries 1.5% to 22.1%,2,6 in Africa 1.5% to 40.9%.3,7 Whereas, in Ethiopia, it is reported as to 12% to 13.2%.8,9
Pseudoexfoliation syndrome has different impacts on the eye. Pseudoexfoliation syndrome is the most common identifiable cause of glaucoma worldwide, accounting for the majority of cases in some countries, and causing both open and angle-closure glaucoma.9 Pseudoexfoliation glaucoma has a much worse visual field and higher optic nerve damage during diagnosis than primary open-angle glaucoma. This may be due to higher and greater fluctuations in pseudoexfoliation glaucoma.10 There are risks of complications such as lens subluxation, zonular dialyses or breaks, posterior capsular rupture, vitreous loss, subluxated intraocular lens, uveitis, hemorrhage, the formation of posterior synechiae, and corneal endothelial decompensation when performing cataract surgery in patients with PXF.7,10
However, studies on the magnitude of PXF and associated factors in our country are limited. Studying the magnitude of PXF and its associated factors is helpful for the early evidence-based intervention of the consequence of PXF on the eye. This study is designed to provide institution-based epidemiological information on pseudoexfoliation syndrome in the population older than 40 years at Gondar university comprehensive specialized hospital tertiary eye care and training center, Ethiopia.
Methods and Materials
Study Design and Period
A hospital-based cross-sectional study was done from January–March 2019.
Study Area
The research was carried out in Gondar university comprehensive specialized hospital tertiary eye care and training center, Gondar city, Northwest of Ethiopia. University of Gondar tertiary eye care and training center provides eye care services in a different specialty for 14 million people of northwest Ethiopia and training for eye care professionals such as optometrists, ophthalmic nurses, and ophthalmologists.
Source/Study Population
All adults who visit Gondar university comprehensive specialized hospital tertiary eye care and training center during the study period.
Inclusion Criteria and Exclusion Criteria
Adult ophthalmic patients age above 40 years who attended Gondar university comprehensive specialized hospital tertiary eye care and training center during the study period were included in the study. Whereas, adult ophthalmic patients age above 40 with cornea opacity which can hinder the anterior segment examination, aphakia, and angle-closure glaucoma were excluded from the study.
Sample Size Determination
The sample size was calculated using the single population proportion formula considering the proportion of PXF, p=39.3% which is taken from a study done in Addis Ababa Ethiopia,11 95% confidence interval and margin of error=5%. Then the calculated sample size was found to be N= 368. Since the total number of source population was less than 10,000 the reduction formula was used. Considering a 5% non-response rate, the final sample size was found to be 318.
Sampling Technique
All consecutive new patients who came to Gondar University comprehensive specialized hospital during the study period age ≥40 years were included in the study until the required sample is obtained.
Operational Definitions
Diagnosis of glaucoma was made if IOP > 21 mmHg with glaucomatous optic disc damage and/or any characteristic visual field defect and if the patient had a history of glaucoma surgery or use of anti-glaucoma eye drops in either eye.12
Participants were classified as having PXF if any pseudoexfoliation material was present on the iris or lens capsule on dilated slit-lamp examination in either eye.13
A participant who drunk >14 units of alcohol with a frequency of once weekly or more was ascertained as an alcohol consumer. Whereas a person who smokes any tobacco product either daily or occasionally is categorized as a smoker.14
A subject was considered to have diabetes if he or she had been diagnosed by a physician, was treated with insulin or oral hypoglycemic agents, findings of diabetic retinopathy in at least one eye during dilated fundus examination, or a combination of the above. Study participants were deemed to have hypertension if they reported being told by a physician that they had hypertension, they were taking antihypertensive medications, findings of hypertensive retinopathy in at least one eye during dilated fundus examination, or a combination thereof.14
Data Collection Tools and Procedures
A pre-tested and structured questionnaire consisting of questions for socio-demographic factors, clinical factors, behavioral factors, and systemic conditions was used to collect the data. Face to face interview was used to assess socio-demographic factors, behavioral factors, and systemic conditions. All participants underwent a complete ocular examination including intraocular pressure measurement, slit-lamp biomicroscope, and dilated fundus examination to obtain clinical factors. All patients’ visual acuity was tested using a standard illuminated Snellen’s chart with illiterate E-optotype. Complete anterior segment examination including pseudoexfoliation identification was held with a slit lamp biomicroscope. The posterior segment was assessed with slit lamp biomicroscope and Volk lens 90D after pupillary dilation with tropicamide 1%. Tonopen applanation tonometer and Goldman visual field analyzer were used to measure intraocular pressure and visual field, respectively.
For IOP measurement only one eye of each person was considered. In people with unilateral PXF, the eye with PXF was considered. In those with bilateral PXF and the patients without PXF, one eye was chosen randomly. Any IOP of more than 21mm Hg was considered as high.
Data Quality Assurance
Questions for socio-demographic factors, behavioral factors, and systemic conditions were translated into the local language Amharic and then translated back into English by language experts to check consistencies in meaning. Pretest was done on 5%16 of the sample size at Felege Hiwot Referral Hospital Bahir Dar.
Training on how to collect the data, the purpose of the study, and how to approach respondents to obtain consent was given for data collectors.
Four data collectors (optometrists) were assigned to administer the questionnaire after getting written informed consent from each participant and to review the chart. The principal investigator and supervisor were strictly engaged in the supervision during the data collection to assure the completeness and consistency of the data.
Data Processing and Analysis
Data were coded, checked, cleaned, and entered into Epi Info 3.5.1. After exporting the cleaned data analysis was performed with SPSS version 20. Frequencies, percentages, and mean were used to describe study results. Chi-square test was used to compare the frequencies and Student’s t-test was used to compare the means of the continuous quantitative variables. Variables with a p-value <0.05 were considered statistically significant.
Results
Sociodemographic Characteristics of Study Participants
In this study, 295 patients age >40 years and above were included in the study with a response rate of 92.8%. The median age (±IQR) was 64 ±9 years. From study participants two hundred (67.8%) were males. More than half of the study participants (56.9%) came from rural residents (Table 1).
 |
Table 1 Sociodemographic Characteristics of Study Participants at Gondar University Comprehensive Specialized Hospital Tertiary Eye Care and Training Center, Ethiopia 2019 |
Ocular, Systemic, and Behavioral Characteristics of Study Participants
Thirty-eight percent of participants had high IOP. Ninety-three (31.5%) participants had glaucoma and 161 (54.6) participants had cataract (Table 2).
 |
Table 2 Systemic and Behavioral Characteristics of Study Participants at Gondar University Comprehensive Specialized Hospital Tertiary Eye Care and Training Center, Ethiopia 2019 |
Proportion of Pseudo Exfoliation Syndrome
Pseudoexfoliation syndrome was found among 102 (34.6%) study participants (95% CI, 29.2–40.7). Among patients with PXF 79 (77.5%) had PXF at the pupillary border, 8(7.8%) had PXF at lens capsule and 15 (14.7%) had PXF at both pupillary border and lens capsule (Figure 1).
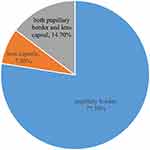 |
Figure 1 A pie chart showing the location of pseudoexfoliation among study participants at Gondar University comprehensive specialized Hospital Tertiary Eye Care and Training Center, Ethiopia 2019. |
Regarding laterality among patients with PXF 81 (50.4%) had PXF bilaterally and 21 (49.6%) had PXF unilaterally.
Factors Associated with Proportion of Pseudoexfoliation Syndrome Among Study Participants
The mean IOP in patients with PXF (26.4 ±11.4mmHg) was significantly higher than in participants without PXF (19.6 ± 8.3mmHg). The proportion of PXF among patients with IOP >21mmHg (50.9%) was significantly higher than those having IOP ≤ 21mmHg (24.6%). The proportion of PXF was significantly higher in patients with glaucoma (54.8%) than those without (25.2%).
The mean age among patients with PXF and those without PXF was significantly different (66.2± 11.8 years) and (60.1±12.6 years), respectively. The proportion of PXF significantly increased as the age increases. The proportion of PXF was 18.7% among patients less than 50 years whereas in patients aged greater than 70 years found to be 43.8%.
The proportion of PXF was significantly higher among males than females with the proportion of PXF 39% vs 25.3%, respectively. Similarly, there was a significant difference in the proportion of PXF among urban (17.3%) and rural (47.6%) residents. Moreover, the proportion of PXF was significantly higher in participants who had outdoor occupation (48.3%) than those who have indoor occupations (20.9%) (Table 3).
 |
Table 3 Factors Associated with the Proportion of Pseudoexfoliation Syndrome Among Adults at Gondar University Comprehensive Specialized Hospital, Gondar, Ethiopia, 2019 |
Discussion
In this study, the proportion of PXF among adults aged ≥40 years was found to be 34.6 (95% CI, 29.2–40.7). This finding is comparable with other study done in Addis Ababa, Ethiopia (39.3%).11 This similarity may be due to a similar study setting since both studies are hospital-based studies. Nevertheless, the result of this study is higher than studies done in Japan (1.5%),2 India (22.1%),6 Jordan (4.9%),15 Latvia (21.6%),16 Turkey (11%),17 Russia (3.6%),4 Nigeria (1.5%),7 and Ethiopia (13.2%).9 One reason for this may be the different study setting, as this study was hospital-based while others were community-based studies. This might also be because of the sample size and age range difference among the study participants.
In this study, the proportion of PXF significantly increases as the age increases. It is well-recognized PXF increases with age since the PXF is considered an age-related disease.18 This result is in agreement with previous studies.3,8,19 Though the explanation for this is indefinite, some speculate that advancing in age results in variation in gene expression which in turn leads to PXF.20
Even though there was no significant gender predominance in previous studies, there was significantly male predominance in the proportion of PXF (39% and 25.3%) in the current study. This finding is in agreement with the Nigerian study.7 This may perhaps be due to men spending most of their time carrying out more outdoor activities compared with women. But it is different from other study done in Sweden21 which shows female predominance. This could be due to the higher proportion of female study participants in Sweden’s study.
The result of this study showed that the mean IOP was significantly high among patients with PXF and the proportion of PXF among study participants with IOP >21mmHg (55.9%) was significantly higher than those having IOP ≤21mmHg (44.1%). This result is consistent with other studies.3,9,17 It was proposed that the accumulation of PXF material clumps may block normal drainage of aqueous humor, which leads to increment of intraocular pressure.22
As glaucoma has a well-established association with PXF in previous studies,3,9,23 this study also found a significantly higher proportion of glaucoma among study participants with PXF (54.8%) than those without it (45.2%). Early identification of these associated disorders is vital because of the more aggressive nature of this type of glaucoma.
Participants who had outdoor occupations had a high proportion of PXF syndrome as compared to those having indoor work. This finding is in harmony with a study done in south India.24 This might be due to that outdoor occupational activities make them have high exposure to solar radiation which is a probable environmental factor for the development of PXF.25
Participants who were rural residents had a high frequency of PXF syndrome as compared to urban residents. The majority of study participants (almost 57%) highly depend on agricultural work and their routine activities were outdoor that may create a significant risk factor for the occurrence of PXF in this population.
Since this study is conducted in a single hospital and focused on ophthalmic patients, a conclusion for the community at large is impossible. Hence, further large-scale population-based studies are necessary to assess the prevalence of PXF and associated risk factors.
Conclusions
Pseudoexfoliation syndrome is high among adults at Gondar University comprehensive specialized eye hospital. It is evidenced that glaucoma is significantly high among participants with PXF. Age, sex, residence, and occupation were significantly associated with PXF.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
The study was conducted in accordance with the Declaration of Helsinki and approved by the institutional review board of the University of Gondar, college of medicine, and health science school of medicine ethical review committee. Participants were informed that participation is voluntary and were given the right to refuse to take part in the study as well as to withdraw at any time during the interview process. Written informed consent was obtained from every participant. No names or identifying information were indicated on the questionnaires, and all subjects were assured of confidentiality.
Acknowledgments
We would like to thank Light for the World for the financial support for this study. We are also grateful for the kindness of all the staffs who were unduly supportive in all ways throughout the study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Light for the World financially supported the data collection for this study.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Turalba A, Cakiner-Egilmez T, Payal AR, et al. Outcomes after cataract surgery in eyes with pseudoexfoliation: results from the veterans affairs ophthalmic surgery outcomes data project. Can J Ophthalmol. 2017;52(1):61–68. doi:10.1016/j.jcjo.2016.07.019
2. Arakaki Y, Sawaguchi S, Iwase A, Tomidokoro A, Araie M. Pseudoexfoliation syndrome and relating factors in a rural Japanese population: the Kumejima Study. Acta Ophthalmol. 2020;98(7):e888–e894. doi:10.1111/aos.14396
3. Kalaycı M. Pseudoexfoliation syndrome pseudoexfoliation syndrome prevalence in Somali patients with senile cataract. Istanb Med J. 2020;21(5):380. doi:10.4274/imj.galenos.2020.12269
4. Bikbov MM, Zainullin RM, Gilmanshin TR, et al. Prevalence and associated factors of pseudoexfoliation in a Russian population: the Ural Eye and Medical Study. Am J Ophthalmol. 2020;210:158–166. doi:10.1016/j.ajo.2019.10.003
5. Rumelaitienė U, Žaliūnienė D, Špečkauskas M, editors. Prevalence of pseudoexfoliation syndrome and it’s association with cataract and glaucoma in Kaunas, Lithuania.
6. Joshi RS, Singanwad SV. Frequency and surgical difficulties associated with pseudoexfoliation syndrome among Indian rural population scheduled for cataract surgery: hospital-based data. Indian J Ophthalmol. 2019;67(2):221. doi:10.4103/ijo.IJO_931_18
7. Idakwo U, Olawoye O, Ajayi BG, Ritch R. Exfoliation syndrome in northern Nigeria. Clin Ophthalmol. 2018;12:271. doi:10.2147/OPTH.S153298
8. Sherief ST, Kibru E, Shibeshe MA. Prevalence of pseudoexfoliation among adults and its related ophthalmic variables in the Southern Ethiopia: a cross sectional study; 2020. Available from: https://www.researchsquare.com/article/rs-7899/v3. Accessed August 19, 2021.
9. Berhanu YA, Giorgis AT, Alemu AM. Prevalence of ocular pseudoexfoliation in Baso and Worena District, central Ethiopia. Ethiop J Health Dev. 2020;34(1):54–58.
10. Olawoye OO, Ashaye AO, Teng CC, Liebmann JM, Ritch R, Ajayi BG. Exfoliation syndrome in Nigeria. Middle East Afr J Ophthalmol. 2012;19(4):402. doi:10.4103/0974-9233.102759
11. Teshome T, Regassa K. Prevalence of pseudoexfoliation syndrome in Ethiopian patients scheduled for cataract surgery. Acta Ophthalmol Scand. 2004;82(3p1):254–258. doi:10.1111/j.1395-3907.2004.00263.x
12. Al‐Bdour MD, Al‐Till MI, Idrees GM, Abu Samra KM. Pseudoexfoliation syndrome at Jordan University Hospital. Acta Ophthalmol. 2008;86(7):755–757. doi:10.1111/j.1755-3768.2008.01258.x
13. Topouzis F, Wilson MR, Harris A, et al. Risk factors for primary open-angle glaucoma and pseudoexfoliative glaucoma in the Thessaloniki eye study. Am J Ophthalmol. 2011;152(2):219–28. e1. doi:10.1016/j.ajo.2011.01.032
14. Viso E, Rodríguez-Ares MT, Gude F. Prevalence of pseudoexfoliation syndrome among adult Spanish in the Salnés eye Study. Ophthalmic Epidemiol. 2010;17(2):118–124. doi:10.3109/09286581003624970
15. Jammal H, Ameera MA, Al Qudah N, et al. Characteristics of patients with pseudoexfoliation syndrome at a tertiary eye care center in Jordan: a retrospective chart review. Ophthalmol Ther. 2021;10(1):51–61. doi:10.1007/s40123-020-00319-w
16. Oberbrinkmann JP. Prevalence of pseudoexfoliation syndrome in cataract patients in Latvia. Riga Stradins University; 2020. Available from: https://dspace.rsu.lv/jspui/handle/123456789/2747. Accessed August 19, 2021.
17. Gunes A, Yasar C, Tok L, Tok O, editors. Prevalence of Pseudoexfoliation Syndrome in Turkish Patients with Senile Cataract. Seminars in Ophthalmology. Taylor & Francis; 2017.
18. Andrikopoulos G, Mela E, Georgakopoulos C, et al. Pseudoexfoliation syndrome prevalence in Greek patients with cataract and its association to glaucoma and coronary artery disease. Eye. 2009;23(2):442–447. doi:10.1038/sj.eye.6702992
19. Lee S-Y, Kim S, Kim JH, et al. Prevalence of pseudoexfoliation syndrome in an isolated island population of Korea: the Woodo Study. J Glaucoma. 2017;26(8):730–734. doi:10.1097/IJG.0000000000000708
20. Karger RA, Jeng SM, Johnson DH, Hodge DO, Good MS. Estimated incidence of pseudoexfoliation syndrome and pseudoexfoliation glaucoma in Olmsted County, Minnesota. J Glaucoma. 2003;12(3):193–197. doi:10.1097/00061198-200306000-00002
21. Åström S, Lindén C. Incidence and prevalence of pseudoexfoliation and open‐angle glaucoma in northern Sweden: i. Baseline report. Acta Ophthalmol Scand. 2007;85(8):828–831. doi:10.1111/j.1600-0420.2007.00992.x
22. Al-Saleh SA, Al-Dabbagh NM, Al-Shamrani SM, et al. Prevalence of ocular pseudoexfoliation syndrome and associated complications in Riyadh, Saudi Arabia. Saudi Med J. 2015;36(1):108. doi:10.15537/smj.2015.1.9121
23. Rajendran N, Shruthy P, Gopal B, Divya V. A clinical study of glaucoma in pseudoexfoliation syndrome. J Case Rep Sci Images. 2021;3(1):04–07.
24. Thomas R, Nirmalan PK, Krishnaiah S. Pseudoexfoliation in southern India: the Andhra Pradesh eye disease study. Invest Ophthalmol Vis Sci. 2005;46(4):1170–1176. doi:10.1167/iovs.04-1062
25. Jiwani AZ, Pasquale LR. Exfoliation syndrome and solar exposure: new epidemiological insights into the pathophysiology of the disease. Int Ophthalmol Clin. 2015;55(4):13. doi:10.1097/IIO.0000000000000092
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
