Back to Journals » Clinical Interventions in Aging » Volume 13
Prevalence of multimorbidity in subjects aged ≥60 years in a developing country
Authors Islas-Granillo H, Medina-Solís CE , Márquez-Corona ML, de la Rosa-Santillana R, Fernández-Barrera MÁ , Villalobos-Rodelo JJ, Hernández-Martínez CT , Navarrete-Hernández JJ , Mendoza-Rodríguez M
Received 18 October 2017
Accepted for publication 18 April 2018
Published 13 June 2018 Volume 2018:13 Pages 1129—1133
DOI https://doi.org/10.2147/CIA.S154418
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Walker
Horacio Islas-Granillo,1 Carlo Eduardo Medina-Solís,1 María de Lourdes Márquez-Corona,1 Rubén de la Rosa-Santillana,1 Miguel Ángel Fernández-Barrera,1 Juan José Villalobos-Rodelo,2 César Tadeo Hernández-Martínez,1 José de Jesús Navarrete-Hernández,1 Martha Mendoza-Rodríguez1
1Academic Area of Dentistry, Health Sciences Institute at Autonomous University of Hidalgo State, Pachuca, Mexico; 2Department of Epidemiology, ISSSTE Sinaloa, Culiacan, Mexico
Background: Aging is one of the most prominent features in recent population dynamics around the world. As populations age, the prevalence of simultaneous chronic diseases increases, which is known as multimorbidity.
Objective: The aim of the present study was to determine the prevalence of multimorbidity and associated factors in a sample of elderly Mexican subjects.
Materials and methods: A cross-sectional descriptive study was performed on a convenience sample of 139 subjects aged ≥60 years. The dependent variable was the multimorbidity diagnosis performed by a physician, which was categorized as 0 for subjects with no chronic disease or only 1 disease and 1 for subjects with 2 or more chronic diseases. Questionnaires were used to collect the information on the different variables. A statistical analysis was performed in Stata 11.0.
Results: The mean age was 79.06±9.78 years, and 69.1% of the subjects were women. A total of 69.1% (95% confidence interval =61.3–76.8) reported at least 1 morbidity. The mean morbidity by subject was 1.04±1.90. Cardiovascular diseases (25.9%), hypertension (20.1%), musculoskeletal disorders (19.4%), and diabetes (13.7%) were the most frequently reported conditions. The prevalence of multimorbidity (2 or more diseases) was 27.3% (95% confidence interval =19.8–34.8). No significant differences were observed in the independent variables.
Conclusion: In conclusion, the prevalence of multimorbidity in this sample of elderly Mexican subjects was relatively low. The distribution across the included variables was not significantly different. Interventions focused on the health care of older adults with multimorbidity should pay special attention to cardiovascular diseases, hypertension, and musculoskeletal disorders.
Keywords: older adults, multimorbidity, cardiovascular disease, hypertension
Introduction
Aging is one of the most prominent features in recent population dynamics around the world. It is partly a result of a sustained decline in fertility levels, a decline in overall mortality and immigration, and an increase in population life expectancy.1 The aging of the population in Mexico is one of the most important challenges facing the country. In a short time, the elderly population will increase relative to other age groups. People aged ≥65 years accounted for 3.7% of the total population in 1970, 6.3% in 2010, and 10.4% in 2015. However, by 2050, they are expected to account for 22.5%. This implies changes in work and production capacities, as well as in the demand for goods and facilities, health services, social security, and family relations. Thus, one of the main challenges of aging is health and determining the origin of the associated dependencies and vulnerabilities. Chronic, degenerative, and incapacitating diseases that occur at advanced ages require specialized medical attention and are extremely costly, incurring out-of-pocket expenses when health insurance is not available, and even catastrophic expenses leading to impoverishment in some cases.2,20 Additionally, the prevalence of simultaneous chronic diseases increases,2 which is known as multimorbidity. Based on a systematic review of the scientific literature, the European General Practice Research Network identified 132 definitions in 416 papers and established the following definition: “Multimorbidity is defined as any combination of a chronic disease with at least one other disease (acute or chronic) or with a psychosocial factor (associated or not) or with a somatic factor.”3 Increased multimorbidity leads to polypharmacy, which is the greater use of medical and social services as well as restrictions on activity, making it a public health problem.4
From an epidemiological point of view, between 60% and 80% of the elderly now present at least 1 chronic illness as a result of the aging population. The negative consequences include increased risk of disability, frailty, hospitalization, institutionalization, and reduction of quality of life, as well as associations with mortality.5–7 Therefore, aging and chronic diseases represent some of the greatest challenges for health systems because they are also highly expensive. Thus, the planning of health care services at the primary care level should take this phenomenon into account among the elderly.7,8
In several countries, the prevalence of multimorbidity in the elderly population and its impact on health care spending have led health agencies to begin addressing the problem and to explore the ways to improve health and function.9 The percentages of multimorbidity observed in other studies around the world are higher than 60%.4,6,9,12
Studies on the prevalence of multimorbidity in the elderly are scarce in developing countries. In Mexico, there is little epidemiological research on health in the elderly. According to the National Health and Nutrition Survey 2012, in Mexico, 27.8% (95% confidence interval =26.2–29.5) of people aged ≥60 years present multimorbidity.14 The objective of the present study was therefore to determine the prevalence of multimorbidity and associated factors in an elderly Mexican sample.
Materials and methods
Design, population, and study sample
A descriptive cross-sectional study was conducted on subjects aged ≥60 years who were either living in long-term care facilities or living independently and attending an adult day care group in the city of Pachuca, Hidalgo, Mexico. Part of the methodology has been published previously.15–17 After obtaining the corresponding permissions, the candidates were invited to participate in the study and were informed of the objectives of the investigation and the confidentiality about the data management. The inclusion criteria were as follows: 1) subjects of either sex, 2) ≥60 years of age, 3) authorized to participate in the research, and 4) enrollment in the aforementioned groups. No sampling was performed, and the participants were volunteers who agreed to participate in the study. The total initial population consisted of 151 subjects, of whom 139 accepted to participate and met the inclusion criteria.
Variables and data collection
We used questionnaires aimed at the elderly and applied by trained personnel to collect the information on sociodemographic, socioeconomic, and general health variables. The response variable was the self-report of morbidities previously diagnosed by physicians and measured according to the health problems presented in Table 1. Multimorbidity was operationalized by counting the diseases/conditions and the combination of the diseases according to a cutoff point suggested in the literature, with 0 indicating subjects with no chronic disease or only 1 disease and 1 indicating subjects with 2 or more chronic diseases. The independent variables were age, sex, type of location, marital status, health insurance, pension/retirement, education, and smoking.
  | Table 1 Prevalence of morbidity (of chronic diseases) in elderly people aged ≥60 years in Pachuca, Mexico |
Analysis of data
The information collected were analyzed in Stata 11.0® (StataCorp, College Station, TX, USA). A descriptive analysis of the sample was carried out, reporting measures of central tendency and dispersion for quantitative variables, as well as frequency and percentages for qualitative variables. Because all the variables were categorical, we used a χ2 test in the bivariate analysis.
We also used latent class analysis to identify unobserved groups of individuals based on multimorbidity indicators. Latent class analysis empirically locates subgroups of individuals who are likely to provide similar responses.
Ethical considerations
This study complied with the specifications of the general health law in research and with the scientific principles of declaration of Helsinki. All individuals signed informed consent forms. The protocol was approved at the Autonomous University of the State of Hidalgo.
Results
The mean age was 79.06±9.78 years (median =80; Q1 =72 Q3 =87), and 69.1% of the subjects were women. Table 1 presents the prevalences of chronic diseases that were included to perform the calculation of multimorbidity. A total of 69.1% (95% confidence interval =61.3–76.8) reported at least 1 morbidity. The most frequent were cardiovascular diseases (25.9%), followed by hypertension (20.1%) and musculoskeletal disorders (19.4%). The overall prevalence of multimorbidity was 27.3% (95% confidence interval =19.8–34.8). The mean multimorbidity was 1.03±0.90 (median =1; Q1 =0 Q3 =2).
Tables 2 and 3 show the results of the descriptive analysis of the different independent variables and bivariate analysis. The χ2 analysis showed no statistically significant differences in any of the sociodemographic, socioeconomic, or risk variables.
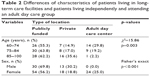  | Table 2 Differences of characteristics of patients living in long-term care facilities and patients living independently and attending an adult day care group |
  | Table 3 Distribution of multimorbidity in elderly people aged ≥60 in Pachuca, Mexico |
Descriptive statistics for latent class analysis variables are shown in Table 4. None of the models provides an adequate fit (p-values were <0.05).
Discussion
In this study, it was not possible to identify the variables associated with the prevalence of multimorbidity, which was 27.3%. This percentage is lower than those observed in other studies around the world, where prevalences of multimorbidity higher than 60% are observed4,6,9,12 but are similar to a previous analysis in Mexico.14 For example, in Brazil, the observed prevalence is 81.3% among people aged ≥60 years.10 In Spain, the prevalence of reported multimorbidity is between 64.1%4 and 67.5% in subjects aged ≥65 years.11 In Burkina Faso, the prevalence was 65% in adults aged ≥60 years.12 In another study, the prevalence of multimorbidity ranged from 24.7% in Switzerland to 51.0% in Hungary among 16 European countries (National representative samples of individuals aged ≥50 years in Austria, Belgium, Switzerland, Germany, Denmark, Spain, France, Italy, the Netherlands, and Slovenia).13 In these studies, the most frequent condition was hypertension. However, there is a lack of consensus on the number and type of health conditions that should be included in the measurement of multimorbidity, which makes it difficult to estimate its prevalence accurately.4 The most prevalent diseases in this Mexican study were cardiovascular problems and hypertension, as in Spain,4 Brazil,6 Burkina Faso,12 and several European countries.16 The comparability of multimorbidity studies is hampered by methodological differences, which are mainly related to the type and number of conditions included in the multimorbidity case definition, the instruments used to measure morbidity, how they were measured, and the population of origin,9–11,18 even within the same country.14 Existing instruments are characterized by their large heterogeneity, ranging from considering only a few (4 diagnoses) to 185 different diseases.19 These discrepancies have been widely discussed in various studies, which suggests a need to standardize the instruments in studies on multimorbidity. In a systematic review, Salive9 mentions that the differences in the prevalences between the studies are probably due to methodological differences rather than actual differences, and it is difficult to find 2 studies that use the same methods. The reported prevalence of multimorbidity is lower in studies with fewer than 10 chronic conditions. However, in studies with 15 conditions, more than 90% may present multimorbidity. Thus, the validity and reliability of the method used to determine a chronic condition affect the prevalence of multimorbidity. In addition, few studies use clinical examination at the time of measurement, and most rely on self-report of clinical diagnosis.9
One of the limitations of the present investigation is that it was a cross-sectional study with self-reported data, so there may be subjects with undiagnosed chronic conditions. This could be the reason for the relatively low prevalence of multimorbidity in this study. Another limitation is the small size of the sample. In addition, the fact that the participants were institutionalized subjects and not community dwelling could introduce some selection bias. Besides, the study used questionnaire to collect data, and this will introduce a recall bias, which is another limitation.
Conclusion
In conclusion, the prevalence of multimorbidity in this sample of elderly Mexican subjects was relatively low. No variables related to the prevalence of the event were detected. Due to the limited information available in Mexico, more studies on the prevalence of multimorbidity are needed to visualize the scenario. It is also necessary to measure the impact that multimorbidity has on the quality of life among the elderly.
Author contributions
Horacio Islas-Granillo and Carlo Eduardo Medina-Solís were involved in the design and development of the study. Carlo Eduardo Medina-Solís designed the study, analyzed the data, and wrote the first draft of the manuscript. María de Lourdes Márquez-Corona, Rubén de la Rosa-Santillana, Miguel Ángel Fernández-Barrera, Juan José Villalobos-Rodelo, César Tadeo Hernández-Martínez, José de Jesús Navarrete-Hernández, and Martha Mendoza-Rodríguez were involved in the conception of the paper, analysis, and interpretation of the results. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All the authors were involved in the critical review and made intellectual contributions, and they also accepted the final version.
Disclosure
The authors report no conflicts of interest in this work.
References
Montoya-Arce J, Montes de Oca-Vargas H. Population aging in the State of Mexico: current situation and future perspectives. Papeles Poblac. 2006;12(50):117–146. | ||
Mendoza-Núñez VM, González-Mantilla F, Correa-Muñoz E, Retana-Ugalde R. Relationship between social support networks and physical functioning in older community-dwelling Mexicans. Int J Environ Res Public Health. 2017;14(9):993. | ||
Fernández-Niño JA, Bustos-Vázquez E. Multimorbidity: conceptual basis, epidemiological models and measurement challenges. Biomédica. 2016;36(2):188–203. | ||
Marventano S, Ayala A, Gonzalez N, Rodríguez-Blázquez C, Garcia-Gutierrez S, Forjaz MJ; Spanish Research Group of Quality of Life and Ageing. Multimorbidity and functional status in community-dwelling older adults. Eur J Intern Med. 2014;25(7):610–616. | ||
Quiñones AR, Markwardt S, Botoseneanu A. Multimorbidity combinations and disability in older adults. J Gerontol A Biol Sci Med Sci. 2016;71(6):823–830. | ||
Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–138. | ||
Kalaiselvi S, Ramachandran N, Nair D, Palanivel C. Prevalence of self-reported morbidities, functional disabilities and access to supportive aids among the elderly of urban Puducherry. West Indian Med J. 2017;66(2):191–196. | ||
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. | ||
Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. | ||
Nunes BP, Thumé E, Facchini LA. Multimorbidity in older adults: magnitude and challenges for the Brazilian health system. BMC Public Health. 2015;15:1172. | ||
Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014;14:75. | ||
Hien H, Berthé A, Drabo MK, et al. Prevalence and patterns of multimorbidity among the elderly in Burkina Faso: cross-sectional study. Trop Med Int Health. 2014;19(11):1328–1333. | ||
Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45(3):431–435. | ||
Bustos-Vázquez E, Fernández-Niño JA, Astudillo-García CI. Self-rated health, multimorbidity and depression in Mexican older adults: proposal and evaluation of a simple conceptual model. Biomedica. 2017;37:92–103. | ||
Islas-Granillo H, Borges-Yáñez A, Fernández-Barrera MA, et al. Relationship of hyposalivation and xerostomia in Mexican elderly with socioeconomic, sociodemographic and dental factors. Sci Rep. 2017;7:40686. | ||
Islas-Granillo H, Borges-Yañez SA, Medina-Solís CE, et al. Tooth loss experience and associated variables among adult Mexicans 60 years and older. P R Health Sci J. 2016;35(2):88–92. | ||
Islas-Granillo H, Borges-Yañez SA, Medina-Solís CE, et al. Dental prosthetic treatment needs in Mexican elders: influence of socioeconomic position. Dent Med Probl. 2017;54(4):383–387. | ||
Ferrer A, Formiga F, Sanz H, Almeda J, Padrós G. Multimorbidity as specific disease combinations, an important predictor factor for mortality in octogenarians: the Octabaix study. Clin Interv Aging. 2017;12:223–231. | ||
Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases – a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2011;66(3):301–311. | ||
Consejo Nacional de Población. Socio-demographic diagnosis of aging in Mexico. Technical Documents Series. México DF: CONAPO; 2011. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

