Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Prereduction traction for the prevention of avascular necrosis before closed reduction for developmental dysplasia of the hip: a meta-analysis
Authors Park KB , Vaidya VN, Shin H , Kwak YH
Received 24 February 2018
Accepted for publication 8 May 2018
Published 24 July 2018 Volume 2018:14 Pages 1253—1260
DOI https://doi.org/10.2147/TCRM.S166531
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Kun-Bo Park,1 Viranchi Narendra Vaidya,2 Hyejung Shin,3 Yoon Hae Kwak4
1Division of Orthopaedic Surgery, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea; 2Division of Orthopaedic Surgery, Kpond Children’s Superspeciality Hospital, Aurangabad, India; 3Biostatistics Collaboration Unit, Medical Research Center, Yonsei University College of Medicine, Seoul, Korea; 4Department of Orthopaedic Surgery, Hallym Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
Background and purpose: Avascular necrosis (AVN) is one of the common complications after closed reduction and hip spica cast for developmental dysplasia of the hip (DDH). Prereduction traction has been used to reduce a dislocated hip or decrease the risk of AVN, but there are conflicting results in prevention effects on AVN. The purpose of this study was to systematically review the current literature and evaluate the effect of prereduction traction in preventing AVN in children with DDH treated by closed reduction through a meta-analysis.
Materials and methods: A systematic review of the literature was performed using PubMed and EMBASE with variations of three major terms: 1) hip dislocation; 2) closed reduction; and 3) avascular necrosis. Seven studies that could compare the incidence of AVN between the traction and no-traction group were included. Methodological quality was assessed, a heterogeneity test was done (p=0.008), and the pooled risk ratios were estimated.
Results: The association between traction and AVN was assessed, using data on 683 hips treated by closed reduction. The incidence of AVN in the traction and no-traction groups ranged from 5% to 47.7% and from 0% to 72.7%, respectively. A meta-analysis with a random effects model indicated no significant difference in the incidence of AVN between traction and no-traction groups (p=0.536).
Conclusion: There was insufficient evidence to decide the efficacy of prereduction traction before closed reduction in reducing the risk of AVN in patients with DDH in this meta-analysis. To recommend prereduction traction for the prevention of AVN, long-term follow-up studies considering age, severity of dislocation, and appropriate traction method are needed.
Keywords: developmental dysplasia of the hip, traction, closed reduction, avascular necrosis
Introduction
The treatment for developmental dysplasia of the hip (DDH) is mainly based on age.1–3 Patients older than 6 months are treated with closed reduction and hip spica cast because the success rate of Pavlik harness is decreased due to the larger and increasingly active child. The success rate after closed reduction and hip spica cast has been reported to be up to 95%; however, the incidence of avascular necrosis (AVN) has been reported to be from 0% to 73%.3,4 AVN has been reported to compromise acetabular development and may result in complications such as abnormal gait, leg length discrepancy, pain, and degenerative joint disease.5–8
The exact etiology of AVN is still unknown and seems to be related to various mechanical and biological factors.9–14 Commonly proposed mechanisms are direct vascular compression and excessive pressure on the femoral head.10 For the prevention of AVN, the presence of the ossific nucleus at the time of reduction, positioning in immobilization, and prereduction traction have been discussed.13,15 Prereduction traction had been recommended with the belief that the traction would stretch the soft tissues that create excessive pressure on the femoral head after reduction, resulting in AVN.2,6
However, there are conflicting results in the literature about the prevention effect of prereduction traction on AVN. Other studies found that traction did not influence the incidence of AVN and requires many accretional resources, such as a longer hospital stay.16 Moreover, Weinstein pointed out that the intraarticular obstacles would not be affected by traction.17 Although there is a trend toward a decreasing use of traction, prereduction traction remains as a treatment tradition or a gesture toward a medico-legal environment.18
Previous studies evaluated AVN with a diverse classification, and the traction method was also variable, so it is difficult to estimate the severity of AVN or compare the effect of variable traction methods. This study focused on the presence of AVN after closed reduction and hip spica cast. The purpose of the study is to determine the efficacy of prereduction traction in reducing the incidence of AVN after closed reduction in DDH through a meta-analysis.
Materials and methods
Search strategy and criteria
We searched PubMed and EMBASE using variations of three key terms: 1) hip dislocation; 2) closed reduction; and 3) avascular necrosis. Search parameters were restricted to English language studies of pediatric populations. Data were extracted from PubMed and EMBASE according to Figure 1. Two authors independently reviewed the title and abstract of each article identified in the literature search. When eligibility was unclear from the title and abstract, the full text of the article was obtained and evaluated for eligibility. At each stage, disagreements were discussed and resolved in a consensus meeting along with the senior reviewers before the next step was carried out.
  | Figure 1 Systematic search strategy results. |
Inclusion and exclusion criteria
All retrospective and prospective studies of DDH where traction was used as a treatment modality and AVN was evaluated as a result or complication of treatment of DDH were included. Articles were excluded based on the following exclusion criteria: 1) studies where neuromuscular or teratologic hip dislocations were present; 2) studies where subluxations had been included in the population and not analyzed separately; 3) studies conducted before 1969, when Salter suggested the criteria for AVN;5 4) studies where AVN had not been evaluated as an independent result; and 5) studies where traction had not been evaluated as an independent effect modifier.
Assessment of study type and quality
The Oxford Centre for Evidence-Based Medicine Levels of Evidence table for the orthopedic literature was used by two authors to independently assess the included studies and assign a level of evidence (I–V).19 The methodological quality of the included studies was assessed using Methodological Index for Nonrandomized Studies (MINORS) checklists.20 According to the MINORS checklist, noncomparative studies were evaluated with eight items, with each rated from 0 to 2 points. The items were study aim, consecutive patients, prospective design, appropriate end points, unbiased assessment, follow-up, dropout rate, and sample size calculation. Additional items, including adequate control group, contemporary groups, baseline group equivalence, and adequate statistical analysis, were used for comparative studies. The maximum possible scores were 16 and 24 for noncomparative and comparative studies, respectively. The quality scoring of studies was directly proportional to their methodological strength with a maximum possible score. No randomized controlled trials were included. All the studies were retrospective and Level III. The median MINORS score for the noncomparative studies was 8 (range 7–8), and the median score for comparative studies was 13 (range 12–16).
Meta-analysis methodology
Treatment effects were reported as the relative risk. The meta-analysis was weighted by the sample size of each study. The hypothesis of statistical heterogeneity was tested using the Cochran’s Q-test, with statistical significance set at the two-tailed 0.10 level, whereas the extent of statistical consistency was measured with I2, defined as 100% × (Q − df)/Q, where Q is Cochran’s heterogeneity statistic and df is the degrees of freedom. Binary outcomes from individual studies were analyzed to compute individual and polled risk ratios, with a pertinent 95% CI, by means of an inverse variance method. A fixed effects model was used in case of low statistical inconsistency (I2<25%) or a random effects model (which better accommodates clinical and statistical variations) was used in case of moderate or high statistical inconsistency (I2>25%). We completed all analyses using Comprehensive Meta-Analysis version 2.0 (Biostat Inc., Englewood, NJ, USA).
Results
Study selection
A total of 785 records were identified. After removal of duplicate citations, 391 and 394 reports were obtained, respectively (Figure 1). A total of 554 articles were obtained after exclusion of 240 overlapping articles, and 487 studies were excluded based on the title and abstract; 67 articles were found to be eligible for initial screening according to the inclusion and exclusion criteria. Of the 60 full texts that were excluded, 21 were nonprimary, 11 had insufficient follow-up data, 22 also included an open reduction procedure, and 6 did not report on osteonecrosis data. This resulted in seven studies3,8,16,21–24 to be included in the present systematic review. Six studies were unanimous selections, and one was selected after a consensus meeting;24 it reported the effect of traction, including both closed reduction and open reduction, but the relevant data were extracted, and hence the paper was included.
Study characteristics and data collection
All seven studies were observational studies in design. They had a no-traction group and traction group; however, there was no random allocation to the groups in any of the studies. The total number of hips included in a study ranged from 36 to 342. The age at the time of surgical reduction ranged from 1 to 55 months. The follow-up duration ranged from 0.5 to 40 years. Although all studies involved traction, the purpose of each study was slightly different. Three studies described the association of traction with AVN.3,16,21 Sibinski et al23 dealt with the clinical course of traction, Brougham et al8 discussed the clinical outcome of closed reduction and focused on AVN of the femoral head, Kutlu et al21 discussed the clinical outcome of closed reduction, and Ishii and Ponseti22 examined the effect of the femoral head ossific nucleus on the incidence of AVN after DDH treatment. The outcome and design of each study are summarized in Table 1. Although the purpose and methods were slightly different, data extraction for analysis was possible, to compare the incidence of AVN between the traction and no-traction groups (Table 2).
  | Table 1 Population characteristics |
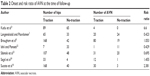  | Table 2 Onset and risk ratio of AVN at the time of follow-up |
Closed reduction was done in 966 hips, of which traction was performed in 683 hips but not in 283 hips. The incidence of AVN in the traction and no-traction groups ranged from 5% to 47.7% and from 0% to 72.7%, respectively. In the diagnosis and classification of AVN, the most commonly used Salter criteria5 for total AVN (Figure S1) was used in four studies. The Gage and Winter classification6 (Figure S2) that provided a definition of partial AVN was used in three studies. The Bucholz and Ogden classification25 (Figure S3) that noted delayed presentation of lateral physeal arrest was used in two studies. However, there was only a short description on the involvement of the epiphysis or metaphysis in the included studies. Radiological criteria were used to assess the adequacy of reduction in two studies and were not clarified in the remaining five. Besides the prereduction traction, we could identify other variables related to AVN; adductor tenotomy was performed in four studies and abduction brace in two.
Meta-analysis
Statistical analysis with the random effects model did not demonstrate a significant difference in the incidence of AVN between the traction and no-traction groups (risk ratio 0.86; 95% CI=0.52–1.40; p=0.536) (Figure 2). The outcomes of the studies included in the meta-analysis demonstrated statistical heterogeneity (Q=17.50, I2=65.72, p=0.008), and the random effects model was used. No publication bias was detected by the funnel plot analysis and Egger’s test (p=0.408).
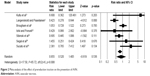  | Figure 2 Meta-analysis of the effect of prereduction traction on the prevention of AVN. |
The factors related to traction are summarized in Table 3. The position of the hip and knee during traction varied, and the duration ranged from 1 to 56 days. The position and duration of the cast after traction also varied. In all studies, there was no indication for termination of traction. Various factors other than preliminary traction were observed, but subgroup analysis could not be performed because common parts were not found. No study utilized statistical adjustments to control for the potential confounders.
  | Table 3 Variables associated with the use of traction |
Discussion
The treatment of choice of DDH has been established and standardized based on long-term follow-up and a large database.26–29 The timing of diagnosis is important, because the treatment of DDH diagnosed in patients over 6 months old is usually done under anesthesia compared to the Pavlik harness in patients under 6 months old.30 Without underlying disease, the most common treatment in children aged 6–24 months with DDH is closed reduction and hip spica cast under general anesthesia.31,32 Despite the standardized method following age groups, the use of prereduction traction for proper reduction and preventing AVN before closed reduction is still controversial.1,33,34 The risk of AVN was reported to be as high as 73% after closed reduction.3 The exact etiology of the high AVN rate after treatment is still unknown but is likely multifactorial.35 Previous studies had focused on various factors related to AVN, including age, sex, hip abduction angle in cast, and prereduction traction. In this meta-analysis, we evaluated whether the prereduction traction can decrease the risk of AVN.
Prereduction traction had been described as a method that might decrease the risk of AVN.3,12,31,36,37 AVN is a multifactorial problem, and prereduction traction is one of the variables associated with AVN. In the previous studies, there were discrepancies in age,12,27 position of traction,7,31 duration of traction,12,24,28 traction weight,25,31 and severity of dislocation.22,26 Besides, although application of traction is relatively simple and performed without anesthesia, there are problems caused by the expense of additional hospitalization or the discomfort of patients. In contrast, there are also many studies that have not found any relationship between prereduction traction and the incidence of AVN.8,16,34,36 Furthermore, a recent study found that the use of prereduction traction was even significantly associated with both the development of AVN and an increased rate of AVN.38 In this meta-analysis, there was no significant difference in the presence of AVN between the prereduction traction and no-traction groups.
Two studies in this meta-analysis showed a significantly lower incidence of AVN in the prereduction traction group. Sibinski et al23 analyzed two groups: in children older than 1 year, the risk of growth disturbances of the proximal femoral epiphysis was significantly reduced in the traction group; however, in children younger than 1 year, physeal arrest occurred in 13/41 patients treated with traction and 4/17 patients treated without traction, which was not statistically significant. Langenskiold and Paavilainen3 described that prereduction traction decreases the incidence of AVN of the femoral head in children aged 6–36 months. However, 86 hips without traction were treated before 1957, and 176 hips with traction were treated after 1957. There may be an improvement in the reduction position or cast technique and quality of radiography. The incidence of AVN was 14.3% in traction group and 33.3% in no-traction group in the study by IIshii and Ponseti.22 However, traction was applied in only seven hips, and we could not confirm whether 15 patients who underwent adductor tenotomy were in the traction or no-traction group.
Meanwhile, three studies of our series confirmed that the relationship between preliminary traction and the occurrence of AVN was not statistically significant. Kutlu et al21 compared two groups similar in age, sex, side, and level of dislocation with consistent method and duration of immobilization and found no significant differences. Brougham et al8 demonstrated that the incidence of AVN was not influenced by traction in average 14 months (1–55 months) of age at reduction and average 12 days (1–28 days) of prereduction traction. Sucato et al16 analyzed a total of 208 hips with DDH and successful closed reduction, which were treated with prereduction Bryant’s traction before closed reduction. They included only patients under 3 years of age at the time of reduction and found that preoperative Bryant’s traction has no protective effect on the development of AVN. In the study of Segal et al24 that evaluated the protective influence of the ossific nucleus in AVN, the incidence of AVN was higher in the traction group (36.4%) than in the no-traction group (25%).
The efficacy of prereduction traction was questioned with strong arguments by Weinstein in 1997.34 He indicated that the incidence of proximal femoral growth disturbance varies widely because of the variety of classification systems (Salter et al,5 Tönnis,39 Bucholz and Ogden,25 and Kalamchi and MacEwen40) and the lack of research about the interobserver and intraobserver reliability. The direction and location of the traction can affect the outcome. There are three main ways to operate the traction: horizontal, vertical overhead (Bryant’s traction), and transitional horizontal-to-vertical with gradual abduction. To stretch the psoas muscle, the major obstacle in closed reduction, the direction of traction is important, and the efficacy may be different between horizontal traction and Bryant’s traction. In addition, because the weight and direction of traction change with time, it is not easy to find the effect of traction on proximal growth disturbance.35 Furthermore, forced abduction or forced abduction with internal rotation is one of the important risk factors for the increased incidence of proximal femoral growth disturbance, but this variable was not considered in many previous studies regarding traction.29
This meta-analysis has several limitations. We included studies conducted after 1969, but traction has been used previously and larger data may be available if we included studies conducted before 1969. However, the most commonly used diagnostic criteria for AVN were established by Salter et al5 in 1969, so we included studies conducted after 1969 for the reliability of meta-analysis. The incidence of AVN depends on the rigor with which the diagnosis is sought and the strictness of adherence to the criteria.27 The Salter criteria5 is used for AVN within 1 year after treatment but is less useful for longer follow-up period. However, type II pattern in Bucholz–Ogden25 is not visible till after 5 years of age. The inconsistency in classification is the limitation of this study; in addition, there is insufficient evidence on the efficacy of prereduction traction for AVN because of this problem. Age at reduction was not uniform across the studies. Three studies8,19,20 did not place age limits on the design itself, and other three3,16,24 were age-restricted to 6–48 months, younger than 12 months, and below 3 years of age. Studies considering age, traction method, severity of dislocation, and secondary procedure are needed to support the efficacy of pre-reduction traction for the prevention of AVN.
Conclusion
This meta-analysis demonstrated that there is insufficient evidence with regard to the efficacy of prereduction traction before closed reduction in reducing the risk of AVN in patients with DDH. Before closed reduction in patients with DDH, pediatric orthopedic surgeons should consider variable factors related to AVN and additional hospital resources or parents’ effort in using the traction. To recommend prereduction traction for the prevention of AVN, long-term follow-up studies considering age, severity of dislocation, and appropriate traction method are needed.
Data-sharing statement
The data sets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors wish to thank Hyun Woo Kim for his advice and Sungmin Kim for his help with the statistical analysis. This study was supported by a faculty research grant of Yonsei University College of Medicine (6-2017-0095).
Author contributions
KBP and YHK conceived and designed this research. VNV and KBP acquired the data. HS did a statistical analysis. KBP revised the manuscript. All authors read and approved the final manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. J Am Acad Orthop Surg. 2001;9(6):401–411. | ||
DeRosa GP, Feller N. Treatment of congenital dislocation of the hip. Management before walking age. Clin Orthop Relat Res. 1987;225:77–85. | ||
Langenskiold A, Paavilainen P. The effect of prereduction traction on the results of closed reduction of developmental dislocation of the hip. J Pediatr Orthop. 2000;20(4):471–474. | ||
Schur MD, Lee C, Arkader A, Catalano A, Choi PD. Risk factors for avascular necrosis after closed reduction for developmental dysplasia of the hip. J Child Orthop. 2016;10(3):185–192. | ||
Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg. 1969;12(1):44–61. | ||
Gage JR, Winter RB. Avascular necrosis of the capital femoral epiphysis as a complication of closed reduction of congenital dislocation of the hip. A critical review of twenty years’ experience at Gillette Children’s Hospital. J Bone Joint Surg Am. 1972;54(2):373–388. | ||
Fogarty EE, Accardo NJ Jr. Incidence of avascular necrosis of the femoral head in congenital hip dislocation related to the degree of abduction during preliminary traction. J Pediatr Orthop. 1981;1(3):307–311. | ||
Brougham DI, Broughton NS, Cole WG, Menelaus MB. Avascular necrosis following closed reduction of congenital dislocation of the hip. Review of influencing factors and long-term follow-up. J Bone Joint Surg Br. 1990;72(4):557–562. | ||
Thomas CL, Gage JR, Odgen JA. Treatment concepts for proximal femoral ischemic necrosis complicating congenital hip disease. J Bone Joint Surg Am. 1982;64(6):817–828. | ||
Cooperman DR, Wallensten R, Stulberg SD. Post-reduction avascular necrosis in congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62(2):247–258. | ||
Law EG, Heistad DD, Marcus ML, Mickelson MR. Effect of hip position on blood flow to the femur in puppies. J Pediatr Orthop. 1982;2(2):133–137. | ||
Weiner DS, Hoyt WA Jr, O’Dell HW. Congenital dislocation of the hip. The relationship of premanipulation traction and age to avascular necrosis of the femoral head. J Bone Joint Surg Am. 1977;59(3):306–311. | ||
Chen C, Doyle S, Green D, et al. Presence of the ossific nucleus and risk of osteonecrosis in the treatment of developmental dysplasia of the hip: a meta-analysis of cohort and case-control studies. J Bone Joint Surg Am. 2017;99(9):760–767. | ||
Gardner RO, Bradley CS, Howard A, Narayanan UG, Wedge JH, Kelley SP. The incidence of avascular necrosis and the radiographic outcome following medial open reduction in children with developmental dysplasia of the hip: a systemic review. Bone Joint J. 2014;96(2):279–286. | ||
Luedtke LM, Flynn JM, Pill SG. A review of avascular necrosis in developmental dysplasia of the hip and contemporary efforts at prevention. Univ Penn Orthop J. 2000;13:22–28. | ||
Sucato DJ, De La Rocha A, Lau K, Ramo BA. Overhead Bryant’s traction does not improve the success of closed reduction or limit AVN in developmental dysplasia of the hip. J Pediatr Orthop. 2017;37(2):e108–e113. | ||
Weinstein SL, Flynn JM. Lovell and Winter’s Pediatric Orthopaedics. 7th ed. Philadelphia: Lippincott Williams & Willkins; 2013:509–510. | ||
Fish DN, Herzenberg JE, Hensinger RN. Current practice in use of prereduction traction for congenital dislocation of the hip. J Pediatr Orthop. 1991;11(2):149–153. | ||
Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–2. | ||
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. | ||
Kutlu A, Ayata C, Ogun TC, Kapicioglu MI, Mutlu M. Preliminary traction as a single determinant of avascular necrosis in developmental dislocation of the hip. J Pediatr Orthop. 2000;20(5):579–584. | ||
Ishii Y, Ponseti IV. Long-term results of closed reduction of complete congenital dislocation of the hip in children under one year of age. Clin Orthop Relat Res. 1978;137:167–174. | ||
Sibinski M, Murnaghan C, Synder M. The value of preliminary overhead traction in the closed management of DDH. Int Orthop. 2006;30(4):268–271. | ||
Segal LS, Boal DK, Borthwick L, Clark MW, Localio AR, Schwentker EP. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop. 1999;19(2):177–184. | ||
Bucholz RW, Ogden JA. Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease. In: The Hip: Proceedings of the Sixth Open Scientific Meeting of the Hip Society. St. Louis: Mosby;1978:43–63. | ||
Forlin E, Choi IH, Guille JT, Bowen JR, Glutting J. Prognostic factors in congenital dislocation of the hip treated with closed reduction. The importance of arthrographic evaluation. J Bone Joint Surg Am. 1992;74(8):1140–1152. | ||
Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76(12):1777–1792. | ||
Schoenecker PL, Dollard PA, Sheridan JJ, Strecker WB. Closed reduction of developmental dislocation of the hip in children older than 18 months. J Pediatr Orthop. 1995;15(6):763–767. | ||
Weinstein SL, Ponseti IV. Congenital dislocation of the hip. J Bone Joint Surg Am. 1979;61(1):119–124. | ||
Gabuzda GM, Renshaw TS. Reduction of congenital dislocation of the hip. J Bone Joint Surg Am. 1992;74(4):624–631. | ||
Daoud A, Saighi-Bououina A. Congenital dislocation of the hip in the older child. The effectiveness of overhead traction. J Bone Joint Surg Am. 1996;78(1):30–40. | ||
Race C, Herring JA. Congenital dislocation of the hip: an evaluation of closed reduction. J Pediatr Orthop. 1983;3(2):166–172. | ||
Kaneko H, Kitoh H, Mishima K, Matsushita M, Ishiguro N. Long-term outcome of gradual reduction using overhead traction for developmental dysplasia of the hip over 6 months of age. J Pediatr Orthop. 2013;33(6):628–634. | ||
Weinstein SL. Traction in developmental dislocation of the hip. Is its use justified? Clin Orthop Relat Res. 1997;338:79–85. | ||
Schoenecker PL, Lesker PA, Ogata K. A dynamic canine model of experimental hip dysplasia. Gross and histological pathology, and the effect of position of immobilization on capital femoral epiphyseal blood flow. J Bone Joint Surg Am. 1984;66(8):1281–1288. | ||
Kahle WK, Anderson MB, Alpert J, Stevens PM, Coleman SS. The value of preliminary traction in the treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1990;72(7):1043–1047. | ||
Tavares JO, Gottwald DH, Rochelle JR. Guided abduction traction in the treatment of congenital hip dislocation. J Pediatr Orthop. 1994;14(5):643–649. | ||
Camp J, Herring JA, Dworezynski C. Comparison of inpatient and outpatient traction in developmental dislocation of the hip. J Pediatr Orthop. 1994;14(1):9–12. | ||
Tönnis D. Ischemic necrosis as a complication of treatment of C.D.H. Acta Orthop Belg. 1990;56(1 Pt A):195–206. | ||
Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62(6):876–888. |
Supplementary materials
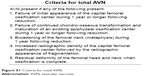  | Figure S1 Criteria for total AVN. |
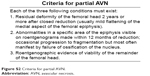  | Figure S2 Criteria for partial AVN. |
  | Figure S3 Bucholz and Ogden1 classification. |
Reference
Bucholz RW, Ogden JA. Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease. In: The Hip: Proceedings of the Sixth Open Scientific Meeting of the Hip Society. St. Louis, MO: Mosby;1978:43–63. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
