Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Preoperative practice of surgical position reduces postoperative pain and discomfort in patients receiving kidney surgeries: a nonrandomized pilot study
Authors Huang J, Zhang D, Li SJ, Xi Y, Cui LY, Gao FL
Received 28 September 2017
Accepted for publication 20 February 2018
Published 13 June 2018 Volume 2018:14 Pages 1111—1114
DOI https://doi.org/10.2147/TCRM.S152836
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Jing Huang,1 Dan Zhang,2 Shu-Jing Li,1 Ying Xi,1 Li-Yan Cui,1 Feng-Li Gao3
1Department of Urology, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Nephrology, Beijing, Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Department of Nursing, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China
Objective: Prolonged maintenance of surgical position often results in postoperative pain and discomfort in patients. The present study aimed to investigate the effect of preoperative practice of surgical position on postoperative pain and general comfort in patients receiving kidney surgeries.
Methods: For this nonrandomized pilot study, 74 patients receiving kidney surgeries were selected using the probability sampling method. Patients from ward 1 were assigned to the practice group (n=35), and those from ward 2 were assigned to the control group (n=39). The practice group were instructed to practice the surgical position for 3 days prior to the surgery. Postoperative pain and comfort were surveyed using two questionnaires for 3 days, respectively. The postoperative pain scores were compared using the Student’s t-test.
Results: The two groups did not differ significantly in wound pain on postoperative days 1–3 (P > 0.05). However, the practice group showed significantly reduced low back pain and contralateral shoulder pain than the control group for 3 postoperative days (P < 0.05). The physical domain score was significantly higher in the practice group than in the control group (P < 0.01).
Conclusion: Preoperative practice of surgical position can effectively reduce postoperative low back pain and contralateral shoulder pain in patients receiving kidney surgeries and improve the physical comfort.
Keywords: surgical position, kidney surgery, postoperative pain, comfort, low back pain, physical comfort
Introduction
A specific surgical position of the patient is often required to expose the operative site. It has been reported that the supine and the lithotomy positions are associated with postoperative low back pain.1 The kidney position is used for kidney surgeries, in which the patient’s abdomen is placed over a lift in the operating table that bends the body to allow access to the retroperitoneal space. However, the kidney position is associated with postoperative peripheral nerve, muscle, and skin injuries. These injuries can result in low back pain, shoulder pain, and general discomfort.
The specific relationships between the surgical position and postoperative low back pain and discomfort are not clear. It might be caused by the additional body strain exerted by the surgical position during operation. The hypothesis of the present study was that preoperative practice of surgical position may help reduce postoperative low back pain. The present study was designed to investigate the effect of preoperative practice of surgical position on postoperative low back pain, shoulder pain, and general comfort in patients receiving kidney surgeries.
Methods
Study design
This is a nonrandomized pilot study.
Ethics approval
The present study was approved by the Institutional Review Board of Beijing Chao-Yang Hospital. All participants provided written informed consent to take part in this study.
Patients
From March 2015 to October 2015, 74 patients receiving kidney surgeries were selected using the probability sampling method (Figure 1). The inclusion criteria were: 1) kidney surgery with the 90° kidney position and 2) good consciousness and intelligence. Patients who refused to participate and those with the following conditions were excluded: 1) mental disorders, 2) diseases of the major organs, 3) vascular diseases of the extremities, and 4) limb deformities.
  | Figure 1 Flowchart of patient selection. |
Patients from ward 1 (n=39) were assigned to the practice group and were instructed to practice the surgical position for 3 days. Patients from ward 2 (n=35) were assigned to the control group.
Practice of the surgical position
Patients of the practice group were instructed to practice the surgical position for 3 days prior to the surgery, twice daily in the morning and in the afternoon, each for 30 min. Patients were shown a diagram of the kidney position (Figure 2). They were instructed to take the 90° lateral position with the ipsilateral side upward. The two arms were straight forward. A 55×35×10–15 cm cushion was placed under the waist near the 11th and 12th ribs. The upper leg was straight, and the lower leg was bent. All patients received laparoscopic surgery under general anesthesia with propofol and remifentanil.
  | Figure 2 Diagram of the kidney position. |
Survey of postoperative pain and comfort
Postoperative pain and comfort were investigated using the Wong-Baker FACES Pain Rating Scale and a Chinese version of the shortened General Comfort Questionnaire.2 The questionnaires were administered for 3 days postoperatively.
Statistical analysis
Categorical data were presented as frequencies or percentages. Continuous data were presented as mean ± SD. Comparisons were made using the Chi-square test or the Student’s t-test. All statistical analyses were carried out using the SPSS 19.0 (SPSS, Chicago, IL, USA). P > 0.05 was considered statistically significant.
Results
General information of the patients
A total of 74 patients were included in the present study. There were 37 males and 37 females with a mean age of 47.5±5.8 years (range, 37–68 years). All surgeries were performed under general anesthesia. The practice and the control groups showed no significant difference in gender, age, body mass index, and preoperative diagnosis (Table 1).
Postoperative pain
The two groups did not differ significantly in wound pain on postoperative days 1–3 (P > 0.05). However, the practice group showed significantly reduced low back pain and contralateral shoulder pain than the control group for 3 postoperative days (all P < 0.05, Table 2).
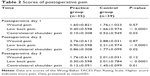  | Table 2 Scores of postoperative pain |
Postoperative comfort
On postoperative days 1–3, there was no significant difference in the general comfort between the two groups (P > 0.05). In the four domains of the shortened General Comfort Questionnaire, the physical domain score was significantly higher in the practice group than in the control group (Table 3). However, the scores of the other three domains (psychospiritual, sociocultural, and environmental) were not significantly different between the two groups.
  | Table 3 Scores of postoperative comfort |
Safety
No practice-related injury or complication was noticed during the present study.
Discussion
The present study found that preoperative practice of the surgical position significantly reduced postoperative low back pain and contralateral shoulder pain in patients receiving kidney surgeries. Practice of the kidney position may strengthen the muscles and tendons of the low-back area and the shoulders. This might help the patients to preemptively adapt to the surgical position and resist fatigue during the surgeries.
According to the comfort theory of Kolcaba, the experience of comfort takes place in four contexts: physical, psychospiritual, sociocultural, and environmental.3–5 One of the aims of nursing is to improve the patient’s experience of comfort. The present study showed that the practice group had significantly higher physical comfort than the control group for 3 postoperative days. Pain is an important aspect of physiology and can cause significant discomfort of the patients.6,7 It was speculated that the reduction in low back pain and shoulder pain resulted in the improvement of the physical comfort. Unsurprisingly, the postoperative scores of the psychospiritual, sociocultural, and environmental comfort were not increased significantly.
The present study is a nonrandomized pilot study with a small sample size. In addition, due to the nature of the practice of surgical position, it is impossible to use blinding or masking. The reduced pain in the practice group may be explained by the placebo effect. Future investigation with a larger sample size and a more reliable study design is needed to confirm the findings of the present study.
Conclusion
In patients receiving kidney surgeries, preoperative practice of the surgical position can significantly reduce the low back pain and the contralateral shoulder pain and significantly improve the physical comfort.
Disclosure
The authors report no conflicts of interest in this study.
References
Clarke AM, Stillwell S, Paterson ME, Getty CJ. Role of the surgical position in the development of postoperative low back pain. J Spinal Disord. 1993;6(3):238–241. | ||
Zhu L, Gao F, Luo H, Deng H, Wang Q. [Reliability and validity of the General Comfort Questionnaire]. Chin J Pract Nurs. 2006;22(5):57–58. | ||
Kolcaba K, Tilton C, Drouin C. Comfort theory: a unifying framework to enhance the practice environment. J Nurs Adm. 2006;36(11):538–544. | ||
Kolcaba K, Wilson L. Comfort care: a framework for perianesthesia nursing. J Perianesth Nurs. 2002;17(2):102–111; quiz 111–113. | ||
Kolcaba KY. A taxonomic structure for the concept comfort. Image J Nurs Sch. 1991;23(4):237–240. | ||
Krenzischek DA, Wilson L, Newhouse R, Mamaril M, Kane HL. Clinical evaluation of the ASPAN Pain and Comfort Clinical Guideline. J Perianesth Nurs. 2004;19(3):150–163. | ||
Pasero C. Pain and comfort issues. J Perianesth Nurs. 2004;19(3):135–137. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

