Back to Journals » Patient Preference and Adherence » Volume 16
Preferences for Attributes of Sodium Oxybate Treatment: A Discrete Choice Experiment in Patients with Narcolepsy
Authors Dubow J, Avidan AY, Corser B, Athavale A, Seiden D, Kushida C
Received 23 December 2021
Accepted for publication 23 March 2022
Published 7 April 2022 Volume 2022:16 Pages 937—947
DOI https://doi.org/10.2147/PPA.S353412
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Jordan Dubow,1 Alon Y Avidan,2 Bruce Corser,3 Amod Athavale,4 David Seiden,1 Clete Kushida5
1Avadel Pharmaceuticals, Chesterfield, MO, USA; 2Department of Neurology, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA; 3Sleep Management Institute, Cincinnati, OH, USA; 4Trinity Life Sciences, Waltham, MA, USA; 5Department of Psychiatry and Behavioral Sciences, Stanford University Medical Center, Stanford Sleep Medicine Center, Redwood City, CA, USA
Correspondence: David Seiden, Tel +1 954 600-4625, Fax +1 636-449-1850, Email [email protected]
Purpose: Current US FDA-approved treatments for narcolepsy include sodium oxybate (SXB) and calcium, magnesium, potassium, and sodium oxybates (mixed-salt oxybates), which require 2 nightly doses, 1 at bedtime and another 2.5 to 4 hours later. Once-nightly SXB (ON-SXB; FT218) is under FDA review to treat adults with narcolepsy. This study quantitatively characterized attributes of SXB treatment preferred by individuals with narcolepsy via a discrete choice experiment (DCE) and evaluated preferences for the product profiles of once-nightly vs twice-nightly SXB treatment.
Patients and Methods: Adults with self-reported physician-diagnosed narcolepsy for ≥ 1 year and current or prior twice-nightly SXB treatment were eligible for this 30-minute, web-based study capturing patient experiences and a DCE. Participants responded to a survey instrument using 9-point scales; higher scores indicated greater severity/preference/satisfaction. In the DCE, hundreds of profiles were generated, each combining attributes of twice-nightly SXB and ON-SXB based on clinical trial data. The DCE was analyzed using a hierarchical Bayesian model.
Results: Seventy-five participants were surveyed (50 current and 25 past twice-nightly SXB users). Dosing frequency was the most important attribute of SXB treatment; once nightly was significantly preferred vs twice nightly. The most common reasons for overall product preference were lack of need to wake up in the middle of the night for a second dose (48%), fewer side effects (46%), and ease of administration (32%). Number of nightly doses was the most important driver of taking the medication exactly as directed and reduced anxiety/stress. Participants were significantly more likely to prefer the blinded product profile of once-nightly SXB over twice-nightly SXB (mean rating, 7.5 vs 4.3; P< 0.05).
Conclusion: Among the choices presented, dosing frequency was the most important attribute for overall product choice, likelihood to take medication exactly as directed, and reducing anxiety/stress. The ON-SXB blinded profile was significantly preferred over twice-nightly SXB.
Keywords: narcolepsy, patient preference, adherence, sodium oxybate, discrete choice experiment, once-nightly
Plain Language Summary
Currently, people with narcolepsy who take sodium oxybate must take 1 dose at bedtime and another 2.5–4 hours later. The US Food and Drug Administration is reviewing a new sodium oxybate that patients would only take once at bedtime. The authors did this study to understand what people with narcolepsy like about sodium oxybate and whether they would prefer once-nightly or twice-nightly treatment.
Participants answered surveys that asked about their disease and sodium oxybate experience. The authors used a method called a discrete choice experiment to understand patient preferences. In this experiment, participants looked at 20 hypothetical product profiles that each combined different characteristics of once-nightly and twice-nightly sodium oxybate. They answered questions about which product they preferred overall, which they would be more likely to take exactly as directed by their doctor, and with which product they would expect to experience less anxiety/stress when thinking about taking it.
Number of nightly doses was the most important driver of overall preference, taking the medication exactly as directed, and reduced anxiety/stress. The most common reasons for overall product preference were not needing to wake up in the middle of the night for a second dose (48%), fewer side effects (46%), and ease of administration (32%). Participants significantly preferred once-nightly vs twice nightly dosing. If approved, a once-nightly form of sodium oxybate may result in better adherence and lower anxiety/stress for patients related to taking their medication.
Introduction
Narcolepsy is a chronic disease that is characterized by severe pathologic hypersomnolence and rapid eye movement sleep intrusion phenomena and is associated with reduced health-related quality of life and increased economic burden.1–4 Sodium oxybate (SXB) is an effective treatment across all narcolepsy symptom domains, including severe excessive daytime sleepiness (EDS), cataplexy, and disrupted nighttime sleep.5–8 Currently approved oxybate treatments are immediate-release solutions including twice-nightly SXB and twice-nightly calcium, magnesium, potassium, and sodium oxybates (mixed-salts oxybate), which require patients to awaken, often to an alarm, for a second dose 2.5 to 4 hours after the first dose.9,10
Although SXB has transformed the management armamentarium for people with narcolepsy,11 some patients may not be able to take SXB or may discontinue treatment with SXB owing to the negative aspects associated with the twice-nightly dosing requirements;11 thus, a once-nightly formulation may be preferable.
For individuals with narcolepsy, adherence with management is often suboptimal.12,13 Suboptimal adherence can result in pervasive symptoms of EDS and persistent cataplexy.14 For many chronic diseases, adherence is enhanced with once-daily dosing compared with twice-daily dosing.15–19 Because twice-nightly dosing is more onerous than twice-daily dosing, patients may be more adherent to a formulation taken once at bedtime. A once-nightly SXB (ON-SXB; FT218) formulation has been evaluated by extensive pharmacokinetic studies and a Phase 3 randomized controlled trial;20 the New Drug Application (NDA) was submitted to the US Food and Drug Administration (FDA) for treatment of EDS and cataplexy in adults with narcolepsy with a target action date of October 15, 2021. At that time, the FDA notified the sponsor that their review of the NDA was still ongoing.
Given that twice-nightly sodium oxybate has been the only oxybate option available for nearly 2 decades, clinicians may have become accustomed to prescribing this regimen. Because narcolepsy is a chronic disorder that typically requires lifelong treatment, understanding patient preference is critical when another option becomes available. Thus, a discrete choice experiment (DCE) was undertaken to assess patient preferences and to quantitatively characterize the attributes of treatment preferred by people with narcolepsy. Following completion of the DCE, a blinded product profile exercise was provided to further evaluate patient preferences for a once-nightly vs twice-nightly narcolepsy treatment.
Materials and Methods
Study Design
This web-based, quantitative study employed a survey that was designed to capture heterogeneous patient perspectives. This study was reviewed and approved by Advarra, an independent Institutional Review Board (Advarra, Columbia, MD), and was performed in accordance with the principles stated in the Declaration of Helsinki. An online patient recruitment agency and the patient advocacy group Wake Up Narcolepsy (Worcester, MA) were used to recruit participants, who were compensated for their participation. All participants provided written informed consent.
Participants
Key Inclusion and Exclusion Criteria
Participants were those with self-reported physician-diagnosed narcolepsy for ≥1 year; eligible participants were required to confirm that they had undergone a sleep study for the diagnosis. To mask the purpose of the study, included respondents selected “narcolepsy” from a list of related and unrelated conditions; dummy conditions were included in the list to further eliminate people who did not have narcolepsy. Additional key inclusion criteria were prior and/or current use of twice-nightly SXB; age ≥18 years; and ability to read and understand English, use a computer, and access the internet. Affiliation with a pharmaceutical company or contract research organization, government agency, or market research/advertising firm was exclusionary.
Survey
The 30-minute, web-based survey included 5 sections: background and patient journey, treatment experience, DCE, static product profile exercise, and closing. All questions within the survey instrument were mandatory for all respondents, and participants could complete the surveys in multiple sittings; if participants did not complete all the assessments, their data were not included in the analysis. The survey instrument included patient demographic data, their narcolepsy symptoms and treatments, and their patient journeys; these surveys were completed before viewing the hypothetical product profiles.
The background and patient journey section included questions that assessed the severity of the participants’ narcolepsy symptoms, rated on a scale from 1 (very mild) through 9 (very severe). Treatment experience questions assessed the perceived importance of aspects of narcolepsy treatment, awareness of existing medications for narcolepsy, overall satisfaction with treatments used, and level of satisfaction with twice-nightly SXB. Preferences were rated on a scale from 1 (not at all satisfied) to 9 (extremely satisfied).
Discrete Choice Experiment
In the DCE section, an orthogonal design was generated; each combined attributes of twice-nightly SXB and ON-SXB from the prescribing information and pivotal trial publications (twice-nightly SXB),9,21–24 and pivotal trial data (ON-SXB)20 (Figure 1).
Participants were shown 10 choice sets each, with 2 hypothetical product profiles presented in each choice set. Participants were asked to make 3 decisions for each choice set:
The first question was intended to evaluate product attributes that were most preferred in overall treatment selection, the second question was intended to identify attributes of narcolepsy treatments to which participants were most likely to be adherent, and the third was intended to identify product attributes that were likely to cause participants less anxiety or stress.
Static Product Profile Exercise
In the static product profile exercise, participants were shown blinded product profiles “Product X” (ON-SXB) and “Product Y” (commercially available twice-nightly SXB) side by side and individually. No comparisons were made with twice-nightly mixed-salts oxybate in this study because when the DCE was designed, the medication was investigational with limited information available. Preference was rated on a scale from 1 (not at all preferred) to 9 (strongly preferred).
In the closing section, participants were asked to rate their level of agreement with statements related to narcolepsy symptoms and treatment experience, and to respond to demographic questions.
Data Collection, Management, and Analysis
To test the overall comprehension of the survey and identify potential sources of response error, particularly for the DCE, 6 patients who met inclusion and exclusion criteria were selected to participate in initial, web-based, cognitive interviews. Minor modifications were incorporated based on these interviews before fielding.
The analyses quantitatively described the treatment attribute preferences in narcolepsy in the overall sample. Differences were compared using either t tests (mean) or chi-squared tests (proportion). Significance was set at an alpha threshold of 0.05. A hierarchical Bayesian model was used to investigate the patient’s preferences of narcolepsy treatment attributes in the DCE. Because of the complexity of DCE studies, traditional statistical-power calculations cannot offer accurate estimates of sample size.25 A hierarchical Bayesian model, as recommended in the International Society for Pharmacoeconomics and Outcomes Research guideline for conjoint analysis,26 can be successfully implemented on a sample size of 75 US adult narcolepsy patients; thus, a sample size of 75 participants was targeted for this study.
Results
Participants
In total, 3200 individuals received an invitation to participate in the study. Of these, 241 recipients completed the screener and 75 participants qualified for the study, which was fielded from June to September 2020. Disqualifications were based on the screening criteria. The 166 disqualified individuals had the following exclusionary characteristics: not adults; did not report a narcolepsy diagnosis; were not diagnosed via a sleep study; had never used twice-nightly SXB; were employed by a pharmaceutical company, contract research organization, government agency, or market research/advertising firm; or participated in narcolepsy research in the past month. Owing to the online nature of the recruitment, the number of individuals who explicitly refused to participate is unknown. Fifty participants were receiving current twice-nightly SXB therapy and 25 were past users of twice-nightly SXB. Of the participants, 77% were non-Hispanic white and 83% were female. The mean age was 39 years, and most participants had private insurance (Table 1). More than 50% of participants were incorrectly diagnosed with another condition before being correctly diagnosed with narcolepsy (depression, 79%; anxiety, 50%; insomnia, 26%).
 |
Table 1 Demographic Characteristics |
Survey: Burden of Narcolepsy and Unmet Need
The most common symptoms of narcolepsy reported by the study population were EDS and poor nighttime sleep, which 93% and 86% of participants, respectively, experienced “fairly often,” “usually,” or “almost always” at diagnosis for narcolepsy. Most participants experienced cataplexy either “rarely” (28% at initial presentation, 25% at diagnosis) or not at all (33% at initial presentation, 24% at diagnosis). The symptoms of tiredness, EDS, and poor nighttime sleep were also the most severe symptoms, with symptom severity rated 8.0, 7.6, and 7.0, respectively.
When rating their level of agreement with statements about the burden of narcolepsy, participants reported that they strongly preferred a treatment administered fewer times (Figure 2). Moreover, participants found waking up to take a second dose stressful and experienced anxiety around taking their second dose. The participants were generally satisfied with the efficacy and safety of treatment with twice-nightly SXB (mean ratings, 5.9–7.9), but were less satisfied with aspects related to taking their medication (frequency of taking the medication, mean rating, 4.8). Efficacy was rated by participants as the most important attribute of a narcolepsy medication (Figure 3). Other important attributes were safety, ability to measure the correct dose, dosing frequency, and unattended prepared medication.
 |
Figure 2 Burden of narcolepsy. Participants indicated their level of agreement or disagreement with each statement on a scale of 1–9, where 1=completely disagree and 9=completely agree. |
Discrete Choice Experiment
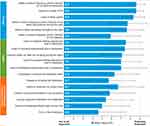
For the participants in the DCE, the number of doses was found to be the most important driver of product choice, taking the medication exactly as directed, and stress/anxiety (Figure 4). Relative preference weight of a once-nightly dosing schedule for likelihood to take the product exactly as described was statistically significantly higher (P<0.001) compared to twice-nightly dosing (relative preference weight, ±119.6) (Figure A1). This trend was also observed with overall preference for once-nightly vs twice-nightly dosing (relative preference weight, ±90.5) and reduced anxiety/stress (relative preference weight, ±92.5) (Figure A1). The most common reasons for overall product preference were lack of need to wake up in the middle of the night to take the second dose (48%), fewer side effects (46%), and ease of taking/handling (32%) (Table 2).
 |
Table 2 Most Common Reasons for Product Preference, Taking Exactly as Directed, and Less Anxiety/Stress |
 |
Figure 4 Drivers of product choice and usage. |
Static Product Profile Exercise
ON-SXB was statistically significantly preferred over twice-nightly SXB owing to its once-nightly dosing schedule (all significant at an α of <0.05). Preference for ON-SXB over twice-nightly SXB was driven by aspects of its efficacy, safety, and dosing schedule (Table 3). The overall level of preference for ON-SXB vs twice-nightly SXB was 7.5 vs 4.3, respectively; likelihood to take as directed was 7.9 vs 5.9, respectively; and likelihood to experience stress/anxiety with taking was 4.5 vs 5.9, respectively. Fewer side effects were frequently mentioned in qualitative responses as a driver of preference for ON-SXB over twice-nightly SXB. ON-SXB was also viewed as more of an advancement in the treatment of narcolepsy than twice-nightly SXB; 27% of respondents rated twice-nightly SXB as “no advancement,” compared with 3% of respondents for ON-SXB, and 24% of patients rated ON-SXB as a “very significant advancement,” compared with 4% for twice-nightly SXB.
 |
Table 3 Expected Satisfaction with ON-SXB and Twice-Nightly SXB |
Discussion
For 2 decades, twice-nightly SXB has been an effective treatment for symptoms of EDS and cataplexy in narcolepsy.21,23,24 Recently, ON-SXB was demonstrated to be highly effective for alleviating symptoms of EDS and cataplexy.20
Patient preferences for twice-nightly or once-nightly formulations of SXB have not previously been investigated because there were no once-nightly options available. This DCE was undertaken to elucidate patient preference for when a once-nightly SXB formulation is available. Of note, the survey completed before the DCE identified that poor nighttime sleep was nearly as common as EDS (85% vs 94%, respectively); both were identified by these participants as among the most severe symptoms they experienced (severity rating, 7.0 and 7.6, respectively). Among the numerous US Food and Drug Administration (FDA)–approved treatments for narcolepsy, only SXB is taken at night and improves nocturnal sleep; however, with the traditional, immediate-release formulations, there is a requisite forced awakening for the consumption of the second dose. In the postmarketing experience for twice-nightly SXB, falls leading to injury have occurred after patients rise from bed.9 Thus, the twice-nightly SXB prescribing information was updated in 2014 to include language advising patients to remain in bed after taking both doses. Given the burden of this chronic condition on patients, reducing the dosing frequency has the potential to improve adherence to the prescribed regimen and decrease the stress and anxiety associated with having to take a second, middle-of-the-night dose. This hypothesis was supported by the results of the DCE, in which the number of doses (1 vs 2) was identified as the most important overall driver of patient preference.
The ability to predict patient compliance with treatment is particularly important in chronic diseases, such as narcolepsy and epilepsy, in which nonadherence to medication can result in poor disease control. For example, for individuals with epilepsy, adherence to medication has been associated with the tolerability of treatment, dosing, interference with everyday life, and patients’ belief that their treatment will be effective.27,28 Because nonadherence leads to poor seizure control,27 understanding patient behavior is necessary to improve treatment compliance. Our findings suggest that the characteristics influencing the management of narcolepsy treatment may be similar to those affecting management of epilepsy. For individuals with narcolepsy, the availability of a once-nightly formulation of SXB may reduce their anxiety about taking their medication, reduce nocturnal adverse events, and increase the perceived benefits of treatment vs the perceived barriers compared with the twice-nightly formulation.
Discordance may exist between healthcare providers’ impressions of what matters to patients in a treatment and what patients report matters to them in a treatment. In particular, regarding SXB, patients may be concerned about losing access to an efficacious treatment, and thus may not be entirely candid with their healthcare provider about their concerns when no other options exist. Thus, a future DCE that assesses healthcare providers’ perceptions of patients’ treatment preference is warranted; it may reveal disconnects between patient and provider perceptions.
Limitations of this study include patient self-reported physician diagnosis of narcolepsy via a sleep study. The sleep study was not defined for the patient, and thus it is unknown whether polysomnography (PSG) and a multiple sleep latency test (MSLT) were included in the diagnosis. However, for a qualified physician to make an appropriate diagnosis of narcolepsy, the “sleep study” must include both PSG and MSLT. Moreover, the screening questions included confounders that were designed to select for and ensure that the participant truly had a diagnosis of narcolepsy. Participants did not differentiate between type 1 and type 2 narcolepsy; given the reported rates of cataplexy, it is probable that the study population included more participants with type 2 than type 1 narcolepsy. The population skewed predominantly non-Hispanic white and female, as do many of the clinical trials, which may limit generalizability. A second immediate-release mixed-salts oxybate was FDA approved after the DCE was designed and thus was not evaluated. This mixed-salts oxybate also requires the same, middle-of-the-night dosing regimen rather than a single bedtime dose, which was identified by participants in this study as the most important driver of overall treatment choice.
Conclusions
SXB dosing frequency (once nightly vs twice nightly) was the most important attribute when considering patient preference for overall product choice, likelihood to take exactly as directed, and decreased anxiety/stress. If approved, FT218, a once-nightly SXB formulation, may result in better adherence and lower anxiety/stress for patients related to taking their medication.
Data Sharing Statement
The data underlying this article will be shared on reasonable request to the corresponding author; data will be stored for a minimum of 10 years after completion of the study.
Ethics Approval and Informed Consent
This study was reviewed and approved by a US Institutional Review Board before study initiation, and all participants provided written informed consent.
Acknowledgments
The authors thank the survey participants and the patient advocacy groups. Trinity Life Sciences collected the data and performed statistical analysis, which was funded by Avadel Pharmaceuticals (Chesterfield, MO). The authors acknowledge Mahaney Sippel, Vijay Abilash, Sumudu Dehipawala, and Lisa Genthner from Trinity Life Sciences for their contributions to the study design, data collection, and data analysis. Medical writing support was provided by Jennifer Fetting, PhD, of The Curry Rockefeller Group, LLC (Tarrytown, NY), and was funded by Avadel Pharmaceuticals (Chesterfield, MO).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Avadel Ireland. Avadel was involved in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Disclosure
J. Dubow is a consultant to and a stockholder and former employee of Avadel Pharmaceuticals. A.Y. Avidan serves on advisory boards for and has received consulting fees from Avadel Pharmaceuticals, Eisai, Harmony Biosciences, Merck Pharmaceuticals, Jazz Pharmaceuticals, and Idorsia Pharmaceuticals; he is a member of the speakers bureaus for and has received honoraria from Eisai and Harmony Biosciences. B. Corser is a member of the speakers bureaus of Jazz Pharmaceuticals, Merck & Co., Inc., Eisai, and Harmony Biosciences. He is an advisor for and has received consulting fees and honoraria from Avadel Pharmaceuticals. A. Athavale is an employee of Trinity Life Sciences. D. Seiden is an employee of Avadel Pharmaceuticals. C. Kushida is a consultant of Avadel Pharmaceuticals and XW Pharma. He reports grants and/or personal fees from XW Pharma, Jazz Pharmaceuticals, NLS Pharmaceuticals, and Avadel Pharmaceuticals, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Daniels E, King MA, Smith IE, Shneerson JM. Health-related quality of life in narcolepsy. J Sleep Res. 2001;10(1):75–81. doi:10.1046/j.1365-2869.2001.00234.x
2. Weaver TE, Mathias SD, Crosby RD, et al. Relationship between sleep efficacy endpoints and measures of functional status and health-related quality of life in participants with narcolepsy or obstructive sleep apnea treated for excessive daytime sleepiness. J Sleep Res. 2021;30(3):e13210. doi:10.1111/jsr.13210
3. Tadrous R, O’Rourke D, Mockler D, Broderick J. Health-related quality of life in narcolepsy: a systematic review and meta-analysis. J Sleep Res. 2021;30(6):e13383. doi:10.1111/jsr.13383
4. Ingravallo F, Gnucci V, Pizza F, et al. The burden of narcolepsy with cataplexy: how disease history and clinical features influence socio-economic outcomes. Sleep Med. 2012;13(10):1293–1300. doi:10.1016/j.sleep.2012.08.002
5. Thorpy MJ. Recently approved and upcoming treatments for narcolepsy. CNS Drugs. 2020;34(1):9–27. doi:10.1007/s40263-019-00689-1
6. Scammell TE. Narcolepsy. N Engl J Med. 2015;373(27):2654–2662. doi:10.1056/NEJMra1500587
7. Maski K, Trotti LM, Kotagal S, et al. Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17(9):1881–1893. doi:10.5664/jcsm.9328
8. Roth T, Dauvilliers Y, Guinta D, Alvarez-Horine S, Dynin E, Black J. Effect of sodium oxybate on disrupted nighttime sleep in patients with narcolepsy. J Sleep Res. 2017;26(4):407–414. doi:10.1111/jsr.12468
9. XYREM (sodium oxybate oral solution, CIII) [prescribing information]. Palo Alto, CA: Jazz Pharmaceuticals; 2020.
10. XYWAV (calcium, magnesium, potassium, and sodium oxybates) [prescribing information]. Palo Alto, CA: Jazz Pharmaceuticals; 2021.
11. Center for Drug Evaluation and Research (CDER). The Voice of the Patient: Narcolepsy. US Food and Drug Administration; 2014.
12. Pérez-Carbonell L, Lyons E, Gnoni V, et al. Adherence to wakefulness promoting medication in patients with narcolepsy. Sleep Med. 2020;70:50–54. doi:10.1016/j.sleep.2020.02.013
13. Rogers AE, Aldrich MS, Berrios AM, Rosenberg RS. Compliance with stimulant medications in patients with narcolepsy. Sleep. 1997;20(1):28–33. doi:10.1093/sleep/20.1.28
14. Mayer G, Plazzi G, Iranzo A, et al. Long-term compliance, safety, and tolerability of sodium oxybate treatment in patients with narcolepsy type 1: a postauthorization, noninterventional surveillance study. Sleep. 2018;41(9):zsy128. doi:10.1093/sleep/zsy128
15. Weeda ER, Coleman CI, McHorney CA, Crivera C, Schein JR, Sobieraj DM. Impact of once- or twice-daily dosing frequency on adherence to chronic cardiovascular disease medications: a meta-regression analysis. Int J Cardiol. 2016;216:104–109. doi:10.1016/j.ijcard.2016.04.082
16. Coleman CI, Limone B, Sobieraj DM, et al. Dosing frequency and medication adherence in chronic disease. J Manag Care Pharm. 2012;18(7):527–539. doi:10.18553/jmcp.2012.18.7.527
17. Coleman CI, Roberts MS, Sobieraj DM, Lee S, Alam T, Kaur R. Effect of dosing frequency on chronic cardiovascular disease medication adherence. Curr Med Res Opin. 2012;28(5):669–680. doi:10.1185/03007995.2012.677419
18. Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22–e33.
19. Laliberte F, Bookhart BK, Nelson WW, et al. Impact of once-daily versus twice-daily dosing frequency on adherence to chronic medications among patients with venous thromboembolism. Patient. 2013;6(3):213–224. doi:10.1007/s40271-013-0020-5
20. Kushida CA, Shapiro CM, Roth T, et al. Once-nightly sodium oxybate (FT218) demonstrated improvement of symptoms in a phase 3 randomized clinical trial in patients with narcolepsy. Sleep.2021;zsab200. doi: 10.1093/sleep/zsab200
21. U. S. Xyrem Multicenter Study Group. A randomized, double blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002;25(1):42–49. doi:10.1093/sleep/25.1.42
22. U. S. Xyrem Multicenter Study Group. Sodium oxybate demonstrates long-term efficacy for the treatment of cataplexy in patients with narcolepsy. Sleep Med. 2004;5(2):119–123. doi:10.1016/j.sleep.2003.11.002
23. Xyrem International Study Group. A double-blind, placebo-controlled study demonstrates sodium oxybate is effective for the treatment of excessive daytime sleepiness in narcolepsy. J Clin Sleep Med. 2005;1(4):391–397. doi:10.5664/jcsm.26368
24. Black J, Houghton WC. Sodium oxybate improves excessive daytime sleepiness in narcolepsy. Sleep. 2006;29(7):939–946. doi:10.1093/sleep/29.7.939
25. Yang JC, Johnson FR, Kilambi V, Mohamed AF. Sample size and utility-difference precision in discrete-choice experiments: a meta-simulation approach. J Choice Model. 2015;16:50–57. doi:10.1016/j.jocm.2015.09.001
26. Hauber AB, Gonzalez JM, Groothuis-Oudshoorn CG, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–315. doi:10.1016/j.jval.2016.04.004
27. Eatock J, Baker GA. Managing patient adherence and quality of life in epilepsy. Neuropsychiatr Dis Treat. 2007;3(1):117–131. doi:10.2147/nedt.2007.3.1.117
28. Sunny AA, Iyer RS, Kumaran SG, Bunshaw NG, Shanmugham K, Govindaraj U. Affordability, availability and tolerability of anti-seizure medications are better predictors of adherence than beliefs: changing paradigms from a low resource setting. Seizure. 2020;83:208–215. doi:10.1016/j.seizure.2020.11.003
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.