Back to Journals » Transplant Research and Risk Management » Volume 14
Predictive Value of Delayed Graft Function Definitions Following Donation After Circulatory Death Renal Transplantation in the United Kingdom
Authors Stirnadel-Farrant HA, Mu G , Cooper-Blenkinsopp S, Schroyer RO, Thorneloe KS, Harrison EM, Andrews SMS
Received 11 September 2021
Accepted for publication 14 April 2022
Published 2 June 2022 Volume 2022:14 Pages 21—33
DOI https://doi.org/10.2147/TRRM.S320221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qing Yi
Heide A Stirnadel-Farrant,1 George Mu,2 Selin Cooper-Blenkinsopp,1 Rosemary O Schroyer,3 Kevin S Thorneloe,4 Ewen M Harrison,5 Susan MS Andrews6
1Department of WorldWide Epidemiology, GlaxoSmithKline, London, UK; 2Department of Data, Methods, and Analytics, GlaxoSmithKline, Collegeville, PA, USA; 3Department of Biostatistics, GlaxoSmithKline, Collegeville, PA, USA; 4Department of Translational Medicine, GlaxoSmithKline, Collegeville, PA, USA; 5Department of Centre for Medical Informatics, Usher Institute, University of Edinburgh, Edinburgh, UK; 6Department of Global Clinical Operations Development R&D, GlaxoSmithKline, Research Triangle Park, NC, USA
Correspondence: Susan MS Andrews, Global Clinical Operations Development R&D GlaxoSmithKline Five Moore Drive, Research Triangle Park, NC, 27709-3398, USA, Tel +1-(919) 649-3944, Email [email protected]
Purpose: A variety of definitions for delayed graft function (DGF) have been proposed, but none has consistently been shown to be superior for predicting long-term graft outcomes for kidney donation after circulatory death (DCD) transplantation. In this study, real-world clinical outcome data following DCD transplantation were explored to determine the value of various DGF definitions for predicting graft survival.
Patients and Methods: Data from 4 centers registered in the UK-based National Health Service Blood and Transplant registry (2010 to mid-2015) were used to assess 4 definitions of DGF in this retrospective chart review study.
Results: Depending on the definition used, the frequency of DGF ranged from 119/362 (32.9%) when DGF was determined with available registry data and based on a requirement for dialysis within 7 days post-transplantation, to 224/315 (71.1%) when based on failure to achieve a 10% fall in serum creatinine (SCr) versus baseline per 24 hours averaged over the first 72 hours. Patients without clinical DGF as determined by a physician upon chart review, or when defined as < 30% reduction in baseline SCr within 7 days post-transplantation with or without dialysis, had significantly better graft survival probability 1 year (hazard ratio 2.08 and 4.48, respectively) and 5 years post-transplant, whereas serum creatinine level over the first 72 hours post-transplant was not predictive of graft survival at 1 year. Patients with clinical DGF upon physician chart review also had higher SCr, lower estimated glomerular filtration rate levels, and were dialyzed more (2.3 days) versus patients without (0.2 days).
Conclusion: Delayed graft function, determined clinically or using a functional definition, is associated with poorer renal function and remains a useful predictor of graft survival at 1 year after DCD kidney transplantation.
Keywords: delayed graft function, DGF, donation after circulatory death, DCD, serum creatinine, SCr
Plain Language Summary
Delayed graft function (DGF) is the failure of a transplanted kidney to function immediately following surgery. Patients with DGF are at an increased risk of long-term kidney failure after their transplant compared to those without DGF. It is helpful to identify this risk as early as possible. There are several ways to define DGF, but it is not yet known which definition is best when the transplanted kidney is received following the cardiac death of a donor (DCD transplantation). This study used available data from a large registry in the UK, together with a review of patient charts, to evaluate several previously described definitions of DGF.
The frequency of DGF varied greatly, ranging from approximately 33% of patients to 71% depending on the definition of DGF that was used. When physicians placed patients into categories upon review of their charts (DGF or non-DGF), the designation of DGF was helpful for predicting kidney failure 1 year after transplant. Patients who had DGF based on kidney function tests (ie, a decrease in serum creatinine levels in the 7 days after their transplant) were also more likely to have kidney failure 1 year later. Patients who did not have DGF by these definitions had better kidney function at 30 days and at 1 year following their transplant. In conclusion, DGF using these definitions may help to predict long-term outcomes after DCD kidney transplantation.
Introduction
Delayed graft function (DGF) is the failure of a transplanted kidney to function immediately following transplantation. The risk of DGF has been reported to be between 24% and 55%, with incidence significantly higher for donation following circulatory death (DCD) than for donation following brain death (DBD).1–3 Depending on other known risk factors such as donor age and cold ischemic time, patients with DGF in DBD cohorts are at an increased risk of graft failure at 1 year and beyond compared to those without DGF.4–6 However, the association between DGF and graft failure in DCD transplantation is less well delineated. With the increasing number of DCD transplants, there is interest in gaining a better understanding of the predictive value of DGF for these patients.1
The diagnosis of DGF is somewhat subjective due to differences among the proposed definitions of DGF. Frequently, DGF is defined clinically as the need for dialysis during the first 7 days post-transplant, excluding dialysis for hyperpotassemia within the first 24 hours postoperatively.3,7,8 A common method for defining DGF functionally is a <10% decline in serum creatinine (SCr) per day for 3 consecutive days in the first week after transplant.9 Numerous other dialysis-, creatinine-, and urine output-based criteria, and combinations thereof have also been proposed,2,8 as well as methods based on creatinine elimination kinetics.10−12 Criticism of the various definitions of DGF is that they are binary and neglect the variability in clinical courses among individuals after transplantation. Therefore, SCr >3 mg/dL on postoperative Day 5 but without a requirement for dialysis has been proposed as a threshold for categorically describing ”intermediate graft function.”13,14
No definition of DGF has consistently been shown to be superior for predicting long-term graft outcomes, particularly with DCD kidney transplantation (vs DBD transplantation).2,8,15 Renal transplantation is a tightly audited activity, with near-complete capture of clinical data by large registries in the peri-operative period and beyond. The rise in DCD kidney transplants has led to the availability of real-world data in the peri-operative period and beyond for the evaluation of outcomes associated with definitions of DGF in this population.16 The aim of the current retrospective chart review study was to provide clinical real-world standard of care data for DGF rates, dialysis events, creatinine levels, and patient and graft survival for 1 year following kidney transplantation. Using these data, clinical dialysis-based definitions and two previously described functional definitions of DGF (based on serum creatinine levels at 3 days and 7 days post-transplantation) were explored to assess the value of each for predicting graft survival after DCD transplantation.
Materials and Methods
Study Design and Patient Population
This was a retrospective, observational chart review study with 1 year of follow-up post DCD kidney transplantation. Data for all patients from sites registered in the UK-based National Health Service Blood and Transplant (NHSBT) registry from 2010 to mid-2015 were included (NHSBT population, N = 3463) (Figure 1). Registry data for patients at 4 of the transplant clinics (Cambridge, Newcastle, Glasgow, and Edinburgh; 4-center NHSBT population, N = 902) were selected based on the availability of patient charts to obtain further detailed data. Of the 902 patients, a subset of 366 patients met the study eligibility criteria (see below) in the 4 centers where real-world longitudinal data on DGF, SCr levels, and dialysis episodes were captured. Data for this subset of patients were entered into GlaxoSmithKline (GSK)-defined electronic case report forms, transmitted electronically to GSK, and combined with laboratory data in a validated data system. Data for 4 patients was dropped due to missing information, for a total of 362 eligible patients in the chart review population.
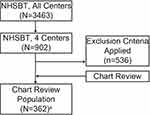 |
Figure 1 Study population flow chart. Abbreviation: NHSBT, National Health Service Blood and Transplant. Note: aData for 4 patients was dropped from a total of 366 due to missing information. |
Patients included in the chart review population were 18 to 79 years of age and first- or second-time transplant recipients of a single kidney donation following DCD, with no history of any other organ transplant (except corneal). Patients who received a kidney allograft with cold ischemic time >36 hours or age <5 years old were excluded. The donor could not have an ABO blood type incompatible with the recipient, T- and/or B-cell positive cross match by complement-dependent cytotoxicity or flow cytometry against the recipient, or an acute or chronic bacterial, viral, or fungal infection that could cause a risk to the recipient. This included serology positive for hepatitis B (except hepatitis B surface antibody and prior vaccination), hepatitis C, human immunodeficiency virus (HIV), or Epstein-Barr virus (EBV)-positive donor allograft with an EBV-negative recipient. Patients were also excluded if normothermic regional machine perfusion organ retrieval techniques were utilized, if surgical damage occurred to the donor allograft during organ procurement, or if the donor was Maastricht Category 1 (dead on arrival), Category 2 (unsuccessful resuscitation), or Category 5 (unexpected cardiac arrest in a critically ill patient).
Patients being treated for acute or chronic infections (hepatitis B, hepatitis C, and HIV), with a history of malignancy in the past 5 years (except for adequately treated basal or squamous cell skin cancer or carcinoma in situ of the uterine cervix), with alanine aminotransferase >2x upper limit of normal (ULN) and bilirubin >1.5 x ULN, or with laboratory evidence of immunodeficiency, were excluded. Additionally, patients could not have any acute cardiovascular syndrome within 6 months before screening, a history of cardiac arrest or malignant ventricular arrhythmia, or single or average QTc >480 msec (for patients with bundle branch block, QTc >500 msec). Patients who had clinical evidence of current drug or alcohol abuse or dependence were not eligible.
Ethical approval was obtained from the UK Institutional Review Board/Independent Ethics Committee. Organs at the 4 centers were donated voluntarily with written informed consent, and the transplant process was conducted in accordance with the Declaration of Istanbul. The NHSBT is a special health authority of the NHS. It is responsible for providing a reliable and efficient supply of blood, organs, tissues, and other services to the NHS. In addition, NHSBT collects information for use in analysis to help make improvements to the transplant service, survival rates and also to help maintain the safety of the transplant service. As such, when subjects agree to join the registry, they consent to having their data shared with other professional organisations which have an interest in improving care for transplant patients and maximising transplant outcomes. All data provided by the NHSBT to GSK, as well as the medical chart review data, remained pseudonymized and individual subject informed consent was therefore not required. Data for this study are reported according to STROBE guidelines for reporting observational studies.
Study Analyses
The requirement for dialysis in the first 7 days post-transplantation, excluding the need for dialysis due to hyperpotassemia within the first 24 hours postoperatively, is commonly considered the gold standard DGF definition. In this study, the frequency of DGF was compared among 4 definitions:
- Physician-assessed clinical DGF upon chart review based on clinical judgment, including patients diagnosed with DGF with no documented dialysis event within 7 days post-transplantation
- Dialysis-based DGF according to available NHSBT registry data (without medical chart review), defined as a requirement for dialysis in the first 7 days post-transplantation, excluding the need for dialysis due to hyperpotassemia within the first 24 hours postoperatively
- Three-day functional DGF defined as a <10% reduction in SCr from baseline (post-transplantation) per 24 hours averaged over the first 72 hours with or without dialysis
- Three-day intermediate graft function defined as a 10% to 20% reduction of SCr from baseline per 24 hours averaged over the first 72 hours without dialysis
- Three-day immediate graft function defined as a >20% reduction of SCr from baseline per 24 hours averaged over the first 72 hours without dialysis
- Seven-day functional DGF defined as a <30% reduction in baseline SCr in the first 7 days with or without dialysis
- Seven-day intermediate graft function defined as a 30% to 70% reduction of SCr from baseline in the first 7 days without dialysis
- Seven-day immediate graft function defined as a >70% reduction in SCr from baseline during the first 7 days without dialysis
Serum creatinine levels post-transplantation in the first 7 days and up to 1 year of follow-up were obtained from patient chart reviews. Serum creatinine area under the curve (AUCSCr, calculated as the average of two SCr measurements × the time difference) from the time of transplant up to Day 7 and Day 30, SCr change from baseline to 1 year, and SCr half-life (t1/2, calculated by adding time on hemodialysis post-transplantation to time for creatinine to fall to half its level immediately after the last hemodialysis session) were derived from reported SCr levels. Estimated glomerular filtration rate (eGFR) was calculated using the modification of diet in renal disease equation,17 and using SCr data from assessments done at least 48 hours after the last day of dialysis. For patients not dialyzed, eGFR values were obtained from 48 hours post-transplant.
The number of dialysis episodes in the first 7 and 30 days post-transplant and duration of dialysis were summarized, excluding patients who underwent dialysis due to hyperpotassemia. Dialysis following a period of 14 days without dialysis was recorded as a new dialysis period. The proportion of dialysis-independent patients at different time points, calculated as whole days from transplant to dialysis and length of time on dialysis (days) within the first year, was also determined.
Additionally, data to determine the frequency of biopsy-proven rejection episodes and graft survival at 1 year, graft survival time, all-cause mortality during the first year post-transplantation, and mortality rate were obtained from NHSBT data. Graft rejection, graft survival time, and mortality across different definitions of DGF were also described within the chart review population when data were available.
Statistical Analyses
The frequency of DGF was summarized for all identified definitions of DGF. Additional analyses were performed both for the overall chart review population and stratified by DGF category, including summary statistics for the number of dialysis episodes, proportion of dialysis-independent patients, graft survival, and all-cause mortality. The longitudinal variations in SCr and eGFR, as well as dialysis duration, were summarized descriptively. One-year graft survival and all-cause mortality were determined using Kaplan–Meier survival estimates. A piecewise autoregressive model was used for SCr levels and to estimate AUCSCr. Values and variations over time were validated. Cox proportional hazard modeling was used for DGF risk in graft survival and mortality. Hazard ratios and their 95% confidence intervals were generated and compared by DGF status for each DGF definition, adjusting for age, SCr at 3 months and 1 year, the number of dialysis events, sex, recipient ethnicity, number of kidney transplants, infection (HIV, hepatitis B, and C), cytomegalovirus, and donor comorbidities. Covariates were selected a priori based on relevant factors available in the NHSBT registry.
Results
Demographic and Transplant Characteristics
In the chart review population (N = 362), patient demographics and transplant characteristics were proportionally similar to the overall NHSBT population (N = 3463) and the 4-center NHSBT population (N = 902), which was limited to the 4 transplant clinics where chart review was performed. There were more males (246/362 [68.0%]) than females, and the majority of transplant recipients were white (351/362 [97.0%]) versus other ethnicities. The mean (standard deviation [SD]) recipient age was 50.9 (12.1) and BMI was 26.8 (4.6) (Table 1).
 |
Table 1 Demographic Characteristics of Recipients and Transplant Characteristics |
At the time of registration for the study, 53.9% of patients were on hemodialysis and 92.8% had no prior kidney transplants. Human leukocyte antigen mismatch was noted for 32.0% for [0 DR and 0/1 B] and 64.1% for [0 DR and 2B] or [1 DR and 0/1 B].
Frequency of DGF
Overall, 148/362 (40.9%) patients had a record of clinical DGF upon chart review, compared with 214 (59.1%) patients who did not (Table 2). When DGF status was determined using only available registry data (according to the dialysis-based DGF definition), only 119/362 (32.9%) of patients met the criteria for DGF.
 |
Table 2 Frequency of DGF by DGF Definition 1 Year Post-Transplantation |
It was possible to define functional status post-transplantation for most patients (315/362 at 3 days and 339/362 at 7 days). Functional status was not defined (23/362) if patients had dialysis within 3 days with a >10% reduction of SCr, or dialysis within 7 days and a >30% reduction of SCr. Based on the 3-day functional definition, 224/315 (71.1%) had DGF. Nineteen (6.0%) had 3-day intermediate graft function and seventy-two (22.9%) had 3-day immediate graft function. Of the 148 patients identified upon chart review with clinical DGF, 110 (74.3%) met criteria for functional DGF based on the 3-day definition (Table 3). Just over half (114/214 [53.3%]) of patients without clinical DGF upon chart review also met the criteria for 3-day functional DGF, showing notable disparity between definitions.
 |
Table 3 Functional DGF Frequency by Frequency of Clinical DGF Upon Chart Review 1 Year Post-Transplantation |
Based on the 7-day functional definition for DGF, nearly two-thirds (217/339 [64.0%]) were classified as having DGF. Eighty-five (25.1%) had 7-day intermediate graft function and 37 (10.9%) had 7-day immediate graft function (Table 2). Almost all patients (135/148 [91.2%]) who had clinical DGF upon chart review were also identified by the 7-day functional definition of DGF, showing substantial overlap between the definitions (Table 3). However, 82/214 (38.3%) patients without clinical DGF upon chart review also met the criteria for 7-day functional DGF.
SCr and eGFR
Mean SCr was higher, as expected, on Day 7, and remained higher on Day 30 versus those without DGF, regardless of whether a dialysis-based (using NHSBT registry data) or a functional definition of DGF was used for categorization (Supplemental Table 1). Geometric mean AUCSCr and increase from baseline (post-transplantation) in AUCSCr values were greater on Days 7 and 30 for patients with clinical DGF upon chart review than for those without (Supplemental Table 2). The difference between mean AUCScr at Day 7 and Day 30 was also greater for patients with clinical DGF versus those without (Supplemental Figure 1). Mean SCr t1/2 was longer (18.0 days) for patients with DGF versus those without (11.6 days) at 1 year post-transplant (Supplemental Table 3). Mean (SD) eGFR over 1 year post-transplant was 39.3 (15.2) mL/min/1.73 m2 in patients without DGF and 30.9 (12.9) mL/min/1.73 m2 in patients with DGF. Patients with DGF upon chart review had a smaller rise in eGFR levels over 1 year post-transplant than patients without (Supplemental Figure 2).
At 7 days post-transplant, 67 (18.5%) patients were categorized as having SCr ≤2.5 mg/dL. No clinical DGF (based on chart review) was reported in these patients; however, 1 acute graft survival event and 4 deaths occurred at 7 days post-transplant. Out of 295 patients with SCr >2.5 mg/dL at 7 days post-transplant, clinical DGF was reported in 148, 25 had an acute graft survival event, and 2 deaths occurred (Supplemental Table 4). At 30 days post-transplant, 268 (74%) patients had SCr ≤2.5 mg/dL. Of those, 86 patients were diagnosed with DGF post-transplant, 12 patients had an acute graft rejection event, and 0 deaths occurred. In patients with SCr >2.5 mg/dL at 30 days post-transplant, there were 61 patients with DGF, 12 acute graft rejection events, and 4 deaths (Supplemental Table 4). Patients who had DGF upon chart review had a higher mean SCr (DGF, 7.1 mg/dL; no DGF, 5.1 mg/dL) and had an average of 2.3 dialysis events versus patients without DGF, who averaged <1 dialysis event (Supplemental Table 5). Most patients without DGF according to chart review were dialysis independent at 7 days and remained so for up to 1 year (178/214 [83.2%]) (Supplemental Table 6), whereas only 11 patients who were categorized with DGF were dialysis independent at 7 days. Eight (5.4%) patients with DGF remained dialysis independent for up to 1 year.
Kidney Allograft Survival and Mortality by DGF Status
One year post-transplant, 346/362 (95.6%) patients had successful kidney allograft survival (Supplemental Table 6). The number of days of survival after the graft was lower in the patients with clinical DGF upon chart review (332.8 days) than for patients without DGF (353.2 days). Additionally, the proportion of patients with graft survival was lower in the patients with clinical DGF upon chart review (92.6%) compared to patients without (97.7%).
Patients in the chart review group without DGF had significantly better graft survival probability than patients with clinical DGF (P<0.05 for both 1 year and 5 years post-transplant) (Figures 2A and B). The adjusted hazard ratio (95% confidence interval [CI]) for those with clinical DGF versus those without was 2.08 (0.63, 6.90). Excluding 2 patients with missing data, there were 6 deaths (2 [1.4%] patients with clinical DGF and 4 [1.9%] without DGF). The difference in mortality in patients with DGF versus those without was not significant up to 1 year post-transplant.
Based on the 7-day functional definition, graft survival probability was also significantly better for patients without DGF versus those with DGF (Figures 3A and B), but there was no significant difference by DGF status based on the 3-day definition (Supplemental Figure 3A and 3B). The adjusted hazard ratio (95% CI) for those with DGF versus those without was 4.48 (0.55, 36.64) for the 7-day definition and 1.79 (0.52, 6.12) for the 3-day definition.
Discussion
This study described DGF rates based on dialysis-based and functional definitions of DGF, dialysis events, SCr levels, and patient and graft survival outcomes within 1 year and 5 years post kidney transplantation. There was variation in the incidence of DGF based on the definition used to categorize patients. When determined with a dialysis-based definition using only available NHSBT data, 32.9% were determined to have DGF whereas 40.9% had clinical DGF according to a physician chart review. Similar to a prior study, functional definitions of DGF identified a greater proportion of patients with DGF than the dialysis-based definition (64.0% and 71.1% based on the 7-day and 3-day definition of functional DGF, respectively).2
When physicians reviewed charts and used clinical judgment to identify patients with DGF, it became apparent that those determined to have DGF may or may not have had a documented dialysis event within the first 7 days post-transplant. Determining DGF with the dialysis-based definition using only available NHSBT registry data identified only 119 of the 148 patients with DGF upon physician chart review. Similar to a previous study, this suggests that dialysis-based definitions for DGF may be more subjective than functional definitions, which are based on a predefined decrease in SCr within a set amount of time and do not rely on the physician’s decision to dialyze.8 It should be noted, however, that there are limitations to retrospective data collection using large registries for comparison with real-world data, including incomplete patient medical histories and the potential for inconsistent application of DGF definitions. In particular, the requirement for dialysis due to hyperpotassemia within the first 24 hours post-transplantation has the potential to contribute to the misinterpretation of data. The last dialysis prior to transplantation, and incidence of hyperphosphatemia and fluid overload were also not available, which could confound results.
There is a lack of consensus as to which definition of DGF has the best predictive value for post-transplant outcomes, particularly following DCD transplants.2,8,15 A previous study showed that DGF by any definition was associated with poorer long-term functional outcomes after DBD kidney transplantation but that only DGF defined by a dialysis-based definition predicted long-term kidney function.2 However, graft survival probability outcomes following DCD transplantation differ from what has previously been reported. In the current study, patients without DGF had significantly better graft survival probability compared with DGF patients at 1 year and 5 years post-transplant when clinical DGF was determined upon chart review or using the 7-day functional definition. While the use of clinical judgment to identify patients with DGF upon chart review may have introduced factors not considered in prior studies, it is unclear why current findings for the 7-day functional definition differ from previous studies. No difference in graft survival probability was shown with the 3-day definition of DGF, and there was less overlap between those determined to have clinical DGF upon chart review and those with DGF by this definition. This is consistent with previous studies that have shown that AUCSCr is a strong predictor of graft rejection and is associated with immunologic events, but only after the initial post-transplant recovery period.18,19 The current results similarly suggest that attempts to diagnose DGF immediately after transplantation may be complicated by the surgical recovery process. However, longer-term kidney function as assessed by serum creatinine and eGFR was worse in patients with DGF (regardless of the definition used) versus those without DGF and patients with DGF experienced 2.3 dialysis events on average in the first 7 days post-transplant, whereas most patients without DGF did not require dialysis. The change in AUCSCr at 7 and 30 days post-transplantation was greater for patients with DGF versus those without.
The inherent subjectivity of determining DGF based on a requirement for dialysis within 7 days post-transplantation may partly explain differences between studies in terms of predicting graft survival. Despite this subjectivity, a dialysis-based definition is likely still of value for predicting functional graft outcomes following DCD transplantation. All but 11 of the 148 patients with DGF upon physician chart review were dialyzed within 7 days post-transplantation, and the current data show that graft survival was significantly worse in this group of patients than for patients without clinical DGF upon chart review. Increased healthcare costs and hospital stays are associated with poorer kidney function and thus, as has been previously reported, DGF may have predictive value following DCD transplantation for this reason alone.2,20
A high proportion (91.2%) of patients with clinical DGF upon chart review also met criteria for DGF according to the 7-day definition. However, the 7-day definition included an additional 82 patients in the DGF group who did not meet clinical DGF criteria, according to chart review. While the predictive value of either definition appears to be useful for functional outcomes, these data suggest that the 7-day functional definition represents a more cautious approach to identifying patients at risk for graft failure.
Conclusion
As with DBD kidney transplantation, both dialysis-based and functional definitions of DGF remain useful for predicting graft survival outcomes after DCD kidney transplantation. The inherent subjectivity of defining DGF may explain differences in predictive value between studies following DCD kidney transplantation but regardless of whether statistical significance can be shown with long-term graft survival, DGF by any definition following DCD kidney transplantation is clinically relevant due to its association with poorer kidney function and consequent treatment and care challenges.
Abbreviations
AUCscr, serum creatinine area under the curve; DBD, brain death; DCD, circulatory death; DGF, delayed graft function; EBV, Epstein-Barr virus; eGFR, estimated glomerular filtration rate; GSK, GlaxoSmithKline; HIV, human immunodeficiency virus; NHSBT, National Health Service Blood and Transplant; SCr, serum creatinine; SD, standard deviation; t1/2, half-life; ULN, upper limit of normal.
Data Sharing Statement
Within 6 months of this publication, anonymized individual participant data, the annotated case report form, protocol, reporting and analysis plan, data set specifications, raw dataset, analysis-ready dataset, and clinical study report will be available for research proposals approved by an independent review committee. Proposals should be submitted to www.clinicalstudydatarequest.com. A data access agreement will be required.
Ethics Approval and Informed Consent
Ethical approval was obtained from the East of England – Cambridge South Research Ethics Committee, Nottingham. The Research Ethics Committee (REC) number is 16/EE/0506.
Consent for Publication
The National Health Service Blood and Transplant (NHSBT) registry is a special health authority of the NHS. It is responsible for providing a reliable and efficient supply of blood, organs, tissues and other services to the NHS. All the data provided by NHSBT to GSK has remained pseudonymised, and individual subject informed consent was therefore not required.
The additional data obtained from the medical CR was limited to existing variables already collected by NHSBT registry. These additional data were an extension of and remained qualitatively similar to the registry data collected, as it was considered that individual retrospective consent would not be required.
Acknowledgments
All listed authors meet the criteria for authorship set forth by the International Committee for Medical Journal Editors. Editorial support (Allyson Lehrman, DPM, assembling tables and figures, collating author comments, copyediting, fact checking, and referencing) and graphic services were provided by AOIC, LLC and were funded by GlaxoSmithKline.
Author Contributions
HAS-F participated in the concept and research design, acquisition of data, data analysis and interpretation, and in writing of the paper. GM participated in the concept and research design, data analysis and interpretation, and in writing of the paper. SC-B participated in the research design and data analysis and interpretation. ROS and KST participated in the concept and research design and data analysis and interpretation. EMH participated in the acquisition of data and data analysis and interpretation. SMSA participated in the concept and research design and data analysis and interpretation. All authors commented critically throughout the development and approved of the final version of the manuscript for submission to Transplant Research and Risk Management. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval for the version to be published, and agree to be accountable for all aspects of the work.
Funding
Funding for this study was provided by GlaxoSmithKline.
Disclosure
HAS-F is a former employee of and holds stock in GlaxoSmithKline (GSK). GM is an employee of and holds stock in GSK. SC-B is a former employee of GSK. ROS is an employee of and holds stock in GSK. KST was an employee of and held stock in GSK. EMH served on the GSK advisory board for this study. SMSA is an employee of and holds stock in GSK. The authors report no other conflicts of interest in this work.
References
1. Summers DM, Johnson RJ, Hudson A, Collett D, Watson CJ, Bradley JA. Effect of donor age and cold storage time on outcome in recipients of kidneys donated after circulatory death in the UK: a cohort study. Lancet. 2013;381(9868):727–734. doi:10.1016/S0140-6736(12)61685-7
2. Moers C, Kornmann NS, Leuvenink HG, Ploeg RJ. The influence of deceased donor age and old-for-old allocation on kidney transplant outcome. Transplantation. 2009;88(4):542–552. doi:10.1097/TP.0b013e3181b0fa8b
3. Tapiawala SN, Tinckam KJ, Cardella CJ, et al. Delayed graft function and the risk for death with a functioning graft. JASN. 2010;21(1):153–161. doi:10.1681/ASN.2009040412
4. Zens TJ, Danobeitia JS, Leverson G, et al. The impact of kidney donor profile index on delayed graft function and transplant outcomes: a single-center analysis. Clin Transplant. 2018;32(3):e13190. doi:10.1111/ctr.13190
5. Mannon RB. Delayed graft function: the AKI of kidney transplantation. Nephron. 2018;140(2):94–98. doi:10.1159/000491558
6. Nicholson ML, Wheatley TJ, Horsburgh T, Edwards CM, Veitch PS, Bell PR. The relative influence of delayed graft function and acute rejection on renal transplant survival. Transp Iint. 1996;9(4):415–419. doi:10.1111/j.1432-2277.1996.tb00901.x
7. Yarlagadda SG, Coca SG, Garg AX, et al. Marked variation in the definition and diagnosis of delayed graft function: a systematic review. Nephrol Dial Transplant. 2008;23(9):2995–3003. doi:10.1093/ndt/gfn158
8. Boom H, Mallat MJ, de Fijter JW, Zwinderman AH, Paul LC. Delayed graft function influences renal function but not survival. Transplant Proc. 2001;33(1–2):1291. doi:10.1016/S0041-1345(00)02482-9
9. Mallon DH, Summers DM, Bradley JA, Pettigrew GJ. Defining delayed graft function after renal transplantation: simplest is best. Transplantation. 2013;96(10):885–889. doi:10.1097/TP.0b013e3182a19348
10. Halloran PF, Aprile MA, Farewell V, et al. Early function as the principal correlate of graft survival. A multivariate analysis of 200 cadaveric renal transplants treated with a protocol incorporating antilymphocyte globulin and cyclosporine. Transplantation. 1988;46(2):223–228. doi:10.1097/00007890-198808000-00007
11. Hariharan S, McBride MA, Cherikh WS, Tolleris CB, Bresnahan BA, Johnson CP. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62(1):311–318. doi:10.1046/j.1523-1755.2002.00424.x
12. Hosgood SA, Barlow AD, Johari Y, Bankart MJ, Nicholson ML. Early graft function defined by area under the curve serum creatinine 7 days post-transplant in a series of live donor kidney transplantation. J Surg Res. 2011;171(2):838–843. doi:10.1016/j.jss.2010.05.063
13. Humar A, Johnson EM, Payne WD, et al. Effect of initial slow graft function on renal allograft rejection and survival. Clin Transplant. 1997;11(6):623–627.
14. Raimundo M, Guerra J, Teixeira C, et al. Intermediate early graft function is associated with increased incidence of graft loss and worse long-term graft function in kidney transplantation. Transplant Proc. 2013;45(3):1070–1072. doi:10.1016/j.transproceed.2013.02.013
15. Moore J, Shabir S, Chand S, et al. Assessing and comparing rival definitions of delayed renal allograft function for predicting subsequent graft failure. Transplantation. 2010;90(10):1113–1116. doi:10.1097/TP.0b013e3181f86966
16. Summers DM, Watson CJ, Pettigrew GJ, et al. Kidney donation after circulatory death (DCD): state of the art. Kidney Int. 2015;88(2):241–249. doi:10.1038/ki.2015.88
17. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470. doi:10.7326/0003-4819-130-6-199903160-00002
18. Setterberg L, Elinder CG, Fored CM, Tyden G, Reinholt FP. Area under the serum creatinine time-curve is a strong predictor of chronic renal allograft rejection. Transplantation. 2000;69(5):964–968. doi:10.1097/00007890-200003150-00050
19. Yilmaz S, Yilmaz A, Häyry P. Chronic renal allograft rejection can be predicted by area under the serum creatinine versus time curve (AUCCr). Kidney Int. 1995;48(1):251–258. doi:10.1038/ki.1995.291
20. Kim DW, Tsapepas D, King KL, et al. Financial impact of delayed graft function in kidney transplantation. Clin Transplant. 2020;34(10):e14022. doi:10.1111/ctr.14022
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


