Back to Journals » Patient Preference and Adherence » Volume 12
Predicting medication nonadherence risk in a Chinese inflammatory rheumatic disease population: development and assessment of a new predictive nomogram
Authors Wang H, Zhang L , Liu Z, Wang X, Geng S, Li J, Li T, Ye S
Received 8 December 2017
Accepted for publication 8 May 2018
Published 10 September 2018 Volume 2018:12 Pages 1757—1765
DOI https://doi.org/10.2147/PPA.S159293
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Huijing Wang,1,* Le Zhang,2,* Zhe Liu,1 Xiaodong Wang,1 Shikai Geng,1 Jiaoyu Li,1 Ting Li,1 Shuang Ye1
1Department of Rheumatology, South Campus, Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China; 2Department of Pharmacy, South Campus, Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
*These authors contributed equally to this work
Purpose: The aim of this study was to develop and internally validate a medication nonadherence risk nomogram in a Chinese population of patients with inflammatory rheumatic diseases.
Patients and methods: We developed a prediction model based on a training dataset of 244 IRD patients, and data were collected from March 2016 to May 2016. Adherence was evaluated using 19-item Compliance Questionnaire Rheumatology. The least absolute shrinkage and selection operator regression model was used to optimize feature selection for the medication nonadherence risk model. Multivariable logistic regression analysis was applied to build a predicting model incorporating the feature selected in the least absolute shrinkage and selection operator regression model. Discrimination, calibration, and clinical usefulness of the predicting model were assessed using the C-index, calibration plot, and decision curve analysis. Internal validation was assessed using the bootstrapping validation.
Results: Predictors contained in the prediction nomogram included use of glucocorticoid (GC), use of nonsteroidal anti-inflammatory drugs, number of medicine-related questions, education level, and the distance to hospital. The model displayed good discrimination with a C-index of 0.857 (95% confidence interval: 0.807–0.907) and good calibration. High C-index value of 0.847 could still be reached in the interval validation. Decision curve analysis showed that the nonadherence nomogram was clinically useful when intervention was decided at the nonadherence possibility threshold of 14%.
Conclusion: This novel nonadherence nomogram incorporating the use of GC, the use of nonsteroidal anti-inflammatory drugs, the number of medicine-related questions, education level, and distance to hospital could be conveniently used to facilitate the individual medication nonadherence risk prediction in IRD patients.
Keywords: noadherence, inflammatory rheumatic diseases, Compliance Questionnaire Rheumatology, predictors, nomogram
Introduction
Medication nonadherence is defined as the act of discontinuing or stopping treatment for the prescribed duration.1 For many chronic diseases including inflammatory rheumatic diseases (IRDs), adherence to long-term therapy in patients is associated with relieving symptoms, decreasing disease flares, and controlling disease progress.2 In addition, the consequences of poor adherence to long-term therapies are poor health outcomes and increased health care cost.3
Poor adherence in chronic diseases is a worldwide problem of striking magnitude.4 Medication adherence in patients with IRDs in the world is relatively low. For example, medication adherence ranged from 30% to 80% in rheumatoid arthritis (RA)5,6 and varied from 3% to 76% in systemic lupus erythematosus (SLE).7 However, medication nonadherence is affected by multiple determinants8 such as socioeconomic factors (eg, practical social support, emotional support, marital status, and family cohesiveness), condition-related factors (eg, health status, work strength, and medical insurance), therapy-related factors (eg, medicine dose, type of medicine, medicine amount, side effects, and medicine-related questions), and patient-related factors (eg, age, sex, employment, income, education level, and distance to hospital).
Considering so many associated risk factors, accurate prediction adherence tools and early intervention may be the most effective actions toward unsatisfactory adherence.9 Furthermore, 19-item Compliance Questionnaire Rheumatology (CQR19) is a suitable adherence measurement and has been developed and identified to assess the effective adherence to medicine in patients with IRDs.10,11 Compliance Questionnaire Rheumatology (CQR) can be used to identify variables related to nonadherence.12,13 Although previous study on RA in China identified many variables associated with adherence,14 no data are available regarding variables related to adherence in IRDs in Chinese patients. Based on CQR, a predictive nomogram might make a difference for IRD patients who might present medication nonadherence. Nevertheless, to our knowledge, there is no study focused on this issue.
The purpose of this study was to develop a valid but simple prediction tool by CQR adherence estimation for IRDs to assess the risk of nonadherence using only characteristics easily available when starting the therapy.
Patients and methods
Patients
Research approval was obtained from Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University’s Ethics Committee (approval no [2016]216K). Patients were recruited from the Shanghai Jiao Tong University of Medicine affiliated Ren Ji Hospital, from March 2016 to May 2016, and they came from all over China. Patients were included if they took rheumatic medicine and fulfilled the American College of Rheumatology (ACR) 1987 or 2012 criteria for ankylosing spondylitis (AS), SLE, RA, and other IRDs. All participating patients provided written informed consent and completed questionnaires assessing adherence to treatment and participated in a 10-minute interview with the specialist pharmacy assistant. Patients who were illiterate, had severe cognitive disorders, or had serious physical constraints were excluded. Data such as demographic, disease, and treatment characteristics of the patients were collected from medical records.
Adherence assessment
CQR19 was used to assess adherence in patients with IRDs. The CQR consists of 19 items about taking medicine, in which patients were asked the degree of agreement with statements. Answers are based on 4-point Likert scales from 4 to 1 (4: agree very much; 3: agree; 2: do not agree; and 1: do not agree at all).10 The final point allows the identification of nonadherent patients (defined as “poor taking compliance” ≤80%) with a small false-positive rate.10 Patients completed the questionnaires with the specialist pharmacy assistant. For each drug, patients were required to report their medication problems face to face and these problems were summarized into the following four dimensions: 1) error on prescription; 2) missing doses; 3) unknown precautions; and 4) stop taking the medicine or adjust dosage by themselves, which explained the number of medication-related problems.
Statistical analysis
All data including demographic, disease, and treatment characteristics were expressed as count (%). Statistical analysis was performed using the R software (Version 3.1.1; https://www.R-project.org).
The least absolute shrinkage and selection operator (LASSO) method, which is suitable for the reduction in high-dimensional data,15,16 was used to select the optimal predictive features in risk factors from the patients with IRDs. Features with nonzero coefficients in the LASSO regression model were selected.17 Then, multivariable logistic regression analysis was used to build a predicting model by incorporating the feature selected in the LASSO regression model. The features were considered as odds ratio (OR) having 95% confidence interval (CI) and as P-value. The statistical significance levels were all two sided. Sociodemographic variables with the P-value of ≤0.05 were included in the model, whereas variables associated with disease and treatment characteristics were all included.18 All potential predictors were applied to develop a predicting model for medication nonadherence risk by using the cohort.19,20
Calibration curves were plotted to assess the calibration of the nonadherence nomogram. A significant test statistic implies that the model does not calibrate perfectly.21 To quantify the discrimination performance of the nonadherence nomogram, Harrell’s C-index was measured. The nonadherence nomogram was subjected to bootstrapping validation (1,000 bootstrap resamples) to calculate a relatively corrected C-index.22 Decision curve analysis was conducted to determine the clinical usefulness of the nonadherence nomogram by quantifying the net benefits at different threshold probabilities in the IRD cohort.23 The net benefit was calculated by subtracting the proportion of all patients who are false positive from the proportion of the patients who are true positive and by weighing the relative harm of forgoing interventions compared with the negative consequences of an unnecessary intervention.24
Results
Patients’ characteristics
A total of 244 patients visiting our clinic from March 2016 to May 2016 completed questionnaires, and the cohort consisted of 99 patients with SLE, 45 patients with AS, 55 patients with RA, and 45 patients with other inflammatory diseases. According to CQR scores, all patients were divided into adherence and nonadherence groups (60 males and 184 females; mean age 41.31±15.52 years [range 15–88 years]). All data of patients including demographic, disease, and treatment features in the two groups are given in Table 1.
Feature selection
Of demographic, disease, and treatment features, 22 features were reduced to five potential predictors on the basis of 244 patients in the cohort (~4:1 ratio; Figure 1A and B) and were with nonzero coefficients in the LASSO regression model.
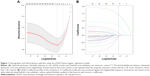  | Figure 1 Demographic and clinical feature selection using the LASSO binary logistic regression model. |
These features included use of glucocorticoid (GC), use of nonsteroidal anti-inflammatory drugs (NSAIDs), number of medicine-related questions, education level, and distance to the hospital (Table 2).
Development of an individualized prediction model
The results of the logistic regression analysis among the use of GC, the use of NSAIDs, the number of medicine-related questions, education level, and distance to hospital are given in Table 2. The model that incorporated the above independent predictors was developed and presented as the nomogram (Figure 2).
Apparent performance of the nonadherence risk nomogram in the cohort
The calibration curve of the nonadherence risk nomogram for the prediction of medication nonadherence risk in IRD patients demonstrated good agreement in this cohort (Figure 3). The C-index for the prediction nomogram was 0.857 (95% CI: 0.807–0.907) for the cohort, and was confirmed to be 0.8472 through bootstrapping validation, which suggested the model’s good discrimination. In the nonadherence risk nomogram, apparent performance addressed a good prediction capability.
Clinical use
The decision curve analysis for the medication nonadherence nomogram is presented in Figure 4. The decision curve showed that if the threshold probability of a patient and a doctor is >14 and <88%, respectively, using this nonadherence nomogram to predict medication nonadherence risk adds more benefit than the scheme. Within this range, net benefit was comparable with several overlaps, on the basis of the nonadherence risk nomogram.
Discussion
Nowadays, nomograms are widely used as prognostic devices in oncology and medicine. Nomograms depended on user-friendly digital interfaces, increased accuracy, and more easily understood prognoses to aid better clinical decision making.25 And our study was the first study that this nomogram was applied in the rheumatic diseases and medication adherence.
We developed and validated a novel prediction tool for nonadherence risk among IRD patients taking rheumatic medicine merely using five easily available variables. Incorporating demographic, disease, and therapy features’ risk factors into an easy-to-use nomogram facilitates the IRD individualized prediction of medicine adherence. This study provided a relatively accurate prediction tool of medication nonadherence for IRD patients. Internal validation in the cohort demonstrated good discrimination and calibration power; especially our high C-index in the interval validation identified that this nomogram can be widely and accurately used for its large sample size.25
In this study, ~46% of the patients did not adhere to their therapy by CQR. In the risk factor analysis, the use of GC, the use of NSAIDs, medicine-related questions, education level, and distance to hospital were associated with medication adherence in IRD patients. This nomogram suggested that using no GC, using NSAIDs, higher education, shorter distance to hospital, and more medicine-related questions may be the key individual factors that determine medication nonadherence risk for IRD patients.
Similar to previous studies,26,27 the use of NSAIDs was also associated with higher nonadherence, which could signify that patients are more likely to discontinue their therapies. This study demonstrated that using GC has better adherence because most patients with adherence to medication were diagnosed with SLE and RA; in other words, GC was their key drug to relieve symptoms.28 Different from previous studies,29,30 higher education may contribute to poorer adherence. Maybe the patients with higher education in the cohort were more worried about rheumatic medication-related questions, such as side effects. Also, different from an other study,31 short distance to hospital may result in poor adherence, which may be associated with our hospital’s rural location. To our surprise, the factor, medicine-related questions, is the most key point to affect medication adherence, which suggested that explaining medicine-related questions especially error in directions and information concerning medicines clearly to patients when starting treatment may enhance medication adherence in IRD patients.25,32,33 Besides, we found that the two questions of missing dose and adjust dosage or stop taking the medicine without doctor’s directions were prominent. Consequently, interventions such as medication reminders and regular follow-up target adherence must be tailored to the particular illness-related demands experienced by the patients.34–36 Disease therapies and personal demographic factors sometimes were difficult to change, but clinicians and pharmacists play a vitally important role in solving medication problems especially at the first time of taking rheumatic medication.32
The IRD patients with better adherence to medication showed better outcomes compared to those with poor adherence,34,36 which demonstrated that developing nonadherence risk prediction tools might improve patient outcomes with individualized risk prediction and interventions. However, there is an effective nonadherence to medication risk prediction tools for patients with IRDs.9 We developed a valid nonadherence risk prediction tool, which assisted clinicians with early identification of patients at high risk of nonadherence to medication. In addition, it may serve as a users’ guide for the optimal selection of IRD patients in clinical research. For example, the developed nomogram will direct investigators to select reliable patients with good adherence to medication by conducting a clinical trial. We can also eliminate some patients with poor adherence when conducting retrospective study, resulting in a more reliable analysis. Moreover, early interventions such as using medication reminders, drug monitoring, and family support will benefit high nonadherence risk patients at the start of their treatment.35,37 Use of reminders as a low-cost aid to enhance adherences should be encouraged in high-risk nonadherent patients.37 Even some occupational therapy is also an acceptable intervention to improve and adopt new medication management behaviors in patients.38
So accurate prognostic assessment will assist physicians with accessing medication nonadherence of patients and taking interventions in time, preventing testing in low-risk situations, and avoiding delays or discontinuity in treatment when there is a high probability of a favorable net benefit. Actually, predicting the nonadherence of individual patients is difficult and suitable measurement and multifaceted interventions may be the most effective answer toward unsatisfactory adherence.9 The limited number of publications assessing determinants of persistence with medication and lack of those providing determinants of adherence to short-term treatment identify areas for future research.8 Most importantly, access to medications is necessary but insufficient in itself for the successful treatment of disease.
Limitations
There are also several limitations of our current study. First, our acquired data collected between March and May might be a low representation of males and a part representation of IRD patients. The cohort was not representative of all Chinese patients with IRDs. Patients without access to treatment were not included. Second, risk factor analysis did not include all potential factors that affected the medication adherence. Some possible aspects of nonadherence were not thoroughly informed such as the social support and other conditions. Third, although the robustness of our nomogram was examined extensively with internal validation using bootstrap testing, external validation could not be conducted and the generalizability was uncertain for other IRD populations in other regions and countries. It needs to be externally evaluated in wider IRD populations.
Conclusion
This study developed a novel nomogram with a relatively good accuracy to help clinicians access the risk of medication nonadherence in IRD patients when starting treatment. With an estimate of individual risk, clinicians and patients can take more necessary measures on life-style monitoring and medical interventions. This nomogram requires external validation, and further research is needed to determine whether individual interventions based on this nomogram will reduce medication nonadherence risk and improve treatment outcome.
Acknowledgments
The study was funded by the National Key Research and Development Program of China (No. 2016YFC0903902), the Shanghai Municipal Commission of Health and Family Planning Committee Scientific Research Project (20174Y0040) and Shanghai Shen Kang Hospital Development Center Clinical Innovation Project (16CR1013A).
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. | ||
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–314. | ||
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52. | ||
Burkhart PV, Sabate E. Adherence to long-term therapies: evidence for action. J Nurs Scholarsh. 2003;35(3):207. | ||
Costedoat-Chalumeau N, Tamirou F, Piette JC. Treatment adherence in systemic lupus erythematosus and rheumatoid arthritis: time to focus on this important issue: treatment adherence in SLE and RA. Rheumatology (Oxford, England). Epub 2017 Sep 11. | ||
van den Bemt BJ, Zwikker HE, van den Ende CH. Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol. 2012;8(4):337–351. | ||
Costedoat-Chalumeau N, Pouchot J, Guettrot-Imbert G, et al. Adherence to treatment in systemic lupus erythematosus patients. Best Pract Res Clin Rheumatol. 2013;27(3):329–340. | ||
Rolnick SJPP, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. | ||
Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: a review of systematic reviews. Front Pharmacol. 2013;4:91. | ||
de Klerk E, van der Heijde D, Landewe R, van der Tempel H, van der Linden S. The compliance-questionnaire-rheumatology compared with electronic medication event monitoring: a validation study. J Rheumatol. 2003;30(11):2469–2475. | ||
de Klerk E, van der Heijde D, van der Tempel H, van der Linden S. Development of a questionnaire to investigate patient compliance with antirheumatic drug therapy. J Rheumatol. 1999;26(12):2635–2641. | ||
van den Bemt BJ, van den Hoogen FH, Benraad B, Hekster YA, van Riel PL, van Lankveld W. Adherence rates and associations with nonadherence in patients with rheumatoid arthritis using disease modifying antirheumatic drugs. J Rheumatol. 2009;36(10):2164–2170. | ||
Garcia-Gonzalez A, Richardson M, Garcia Popa-Lisseanu M, et al. Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol. 2008;27(7):883–889. | ||
Xia Y, Yin R, Fu T, et al. Treatment adherence to disease-modifying antirheumatic drugs in Chinese patients with rheumatoid arthritis. Patient Prefer Adherence. 2016;10:735–742. | ||
Sauerbrei W, Royston P, Binder H. Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med. 2007;26(30):5512–5528. | ||
Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33(1):1–22. | ||
Kidd AC, McGettrick M, Tsim S, Halligan DL, Bylesjo M, Blyth KG. Survival prediction in mesothelioma using a scalable LASSO regression model: instructions for use and initial performance using clinical predictors. BMJ Open Respir Res. 2018;5(1):e000240. | ||
Xing J, Min L, Zhu S, et al. Factors associated with gastric adenocarcinoma and dysplasia in patients with chronic gastritis: a population-based study. Chin J Cancer Res. 2017;29(4):341–350. | ||
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–e180. | ||
Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–1370. | ||
Kramer AA, Zimmerman JE. Assessing the calibration of mortality benchmarks in critical care: the Hosmer-Lemeshow test revisited. Crit Care Med. 2007;35(9):2052–2056. | ||
Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23(13):2109–2123. | ||
Vickers AJ, Cronin AM, Elkin EB, Gonen M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak. 2008;8:53. | ||
Huang YQ, Liang CH, He L, et al. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol. 2016;34(18):2157–2164. | ||
Wei L, Champman S, Li X, et al. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open. 2017;7(10):e017293. | ||
Marras C, Monteagudo I, Salvador G, et al. Identification of patients at risk of non-adherence to oral antirheumatic drugs in rheumatoid arthritis using the Compliance Questionnaire in Rheumatology: an ARCO sub-study. Rheumatol Int. 2017;37(7):1195–1202. | ||
Ahluwalia V, Rampakakis E, Movahedi M, et al. Predictors of patient decision to discontinue anti-rheumatic medication in patients with rheumatoid arthritis: results from the Ontario best practices research initiative. Clin Rheumatol. 2017;36(11):2421–2430. | ||
Saag KG. Glucocorticoid-induced osteoporosis. Endocrinol Metab Clin North Am. 2003;32(1):135–157, vii. | ||
Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;16(7):e172. | ||
Hromadkova L, Soukup T, Vlcek J. Quality of life and drug compliance: their interrelationship in rheumatic patients. J Eval Clin Pract. 2015;21(5):919–924. | ||
Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26(5):331–342. | ||
Bruns T, Stallmach A. Drug monitoring in inflammatory bowel disease: helpful or dispensable? Dig Dis. 2009;27(3):394–403. | ||
Geryk LL, Blalock S, DeVellis RF, Morella K, Carpenter DM. Associations between patient characteristics and the amount of arthritis medication information patients receive. J Health Commun. 2016;21(10):1122–1130. | ||
van Heuckelum M, van den Ende CHM, Houterman AEJ, Heemskerk CPM, van Dulmen S, van den Bemt BJF. The effect of electronic monitoring feedback on medication adherence and clinical outcomes: a systematic review. PLoS One. 2017;12(10):e0185453. | ||
Ji J, Zhang L, Zhang Q, et al. Functional disability associated with disease and quality-of-life parameters in Chinese patients with rheumatoid arthritis. Health Qual Life Outcomes. 2017;15(1):89. | ||
Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;(11):Cd000011. | ||
Bruera S, Barbo AG, Lopez-Olivo MA. Use of medication reminders in patients with rheumatoid arthritis. Rheumatol Int. 2016;36(11):1543–1548. | ||
Schwartz JK, Grogan KA, Mutch MJ, et al. Intervention to improve medication management: qualitative outcomes from a phase I randomized controlled trial. Am J Occup Ther. 2017;71(6). |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





