Back to Journals » Clinical Ophthalmology » Volume 10
Practice patterns in the use of prophylactic antibiotics following nonoperative orbital fractures
Authors Wang JJ, Koterwas JM, Bedrossian EH Jr, Foster WJ
Received 20 July 2016
Accepted for publication 13 August 2016
Published 27 October 2016 Volume 2016:10 Pages 2129—2133
DOI https://doi.org/10.2147/OPTH.S117706
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jijo Jizhou Wang,1 Jennifer M Koterwas,2 Edward H Bedrossian Jr,2 William J Foster2,3
1Lewis Katz School of Medicine, 2Department of Ophthalmology, Lewis Katz School of Medicine, 3Department of Bioengineering, College of Engineering, Temple University, Philadelphia, PA, USA
Purpose: The purpose of this study was to analyze the practice management patterns of the current members of the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) and to determine the use of oral prophylactic antibiotics in an attempt to prevent orbital cellulitis following nonoperative orbital fractures.
Patients and methods: A cross-sectional web-based survey was emailed to all the members of ASOPRS regarding their current management of nonsurgical orbital fractures and their experience with orbital cellulitis following nonoperative orbital fractures.
Results: The majority of practicing oculoplastic surgeon members of ASOPRS do not routinely prescribe prophylactic antibiotics for patients with nonoperative orbital fractures or patients with orbital fractures whom the physicians are observing and who might potentially need surgical intervention. Among the reported cases of orbital cellulitis following a nonoperative orbital fracture in this survey, more than a quarter of the patients had received prophylactic antibiotics. Furthermore, among physicians who have managed orbital cellulitis following nonoperative fracture, 75% (33 out of 44 physicians) report that <1% of patients develop orbital cellulitis.
Conclusion: Despite frequent recommendation for the use of prophylactic antibiotics after orbital fractures in commonly cited ophthalmic references, the majority of oculoplastic surgeons do not use prophylactic antibiotics for orbital fractures, including both nonoperative orbital fractures and orbital fractures that may potentially need surgery.
Keywords: orbital blowout fracture, orbital fracture, antibiotic use, practice patterns, survey
Introduction
The incidence of posttraumatic orbital fractures diagnosed by emergency departments is estimated to be >100,000 per year.1 Majority of these fractures are managed conservatively, without the need for surgical repair.2 At this time, however, there is no clear consensus on the role of antibiotics in nonoperative orbital fractures in the literature, and there are no standards to support prescribing prophylactic antibiotics in closed orbital fractures. Yet, many of the most commonly cited clinical references recommend the use of prophylactic antibiotics. The Wills Eye Manual recommends broad spectrum prophylactic antibiotics and only later acknowledges a controversy in the use of prophylactic antibiotics:
The use of prophylactic antibiotics in orbital fracture is controversial. Antibiotics are recommended if the patient has a history of sinusitis, diabetes, or is otherwise immunocompromised. In all other patients, the decision about antibiotic use is left up to the treating physician.3
Aside from recommending patients to avoid blowing their nose for several weeks after the orbital fracture and prescribing nasal decongestant spray, Joseph and Glavas noted: “Many physicians also use prophylactic antibiotics to prevent possible orbital cellulitis from bacterial spread if a fracture creates a direct orbital communication with the sinuses,” in their 2011 Clinical Ophthalmology review article on orbital fractures.4 The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology states that systemic antibiotics have been advocated by some authors.5 Theoretically, an orbital fracture allows direct communication between the maxillary or ethmoid sinuses and the orbit, allowing for bacteria to spread from the sinuses into the orbit and causing orbital cellulitis.6 However, in the absence of sinusitis, the sinuses are considered to be sterile, thus technically eliminating the risk of orbital cellulitis following an orbital fracture from this proposed mechanism.7
Currently in the literature, there have not been any large, randomized, controlled studies that have looked at the role of prophylactic antibiotics in preventing orbital cellulitis following nonsurgical orbital fractures. The exact incidence of orbital cellulitis following a nonsurgical orbital fracture is also unknown, although estimated to be rare. Only a small number of case reports describing orbital cellulitis following a nonsurgical orbital fracture have been reported.6,8–13 Interestingly, in many of these case reports, prophylactic antibiotics were initially prescribed to the patient who subsequently developed orbital cellulitis, bringing into question the exact role of prophylactic antibiotics and which antibiotic should be administered.8,10
Proponents of antibiotic prophylaxis following orbital fractures stress the importance of preventing orbital cellulitis and its devastating complications, which include optic neuritis, optic atrophy, blindness, cavernous sinus thrombosis, superior orbital fissure syndrome, meningitis, subdural empyema, and death.8–11 However, antibiotics have their own risks including allergic reactions and systemic side effects, and if used unnecessarily, they can promote antimicrobial resistance.14 In addition to these risks, the expense of the antibiotics adds to the overall health-care costs, and therefore, the necessity of the antibiotics should be justified.15 Because of these risks, some physicians are questioning the practice of routinely prescribing prophylactic antibiotics for nonsurgical orbital fractures.9,12,15
Given the high frequency of nonoperative orbital fractures and the lack of research regarding the role of prophylactic antibiotics, the members of the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) were surveyed to understand their current management of nonoperative orbital fractures. The overall objective was to determine whether there is a consensus on the role of prophylactic antibiotics in nonsurgical orbital fractures, to ascertain the frequency of orbital cellulitis following nonsurgical orbital fractures, and to identify the risk factors for orbital cellulitis following nonsurgical orbital fractures.
Materials and methods
A web-based survey was developed and administered using Qualtrics (Qualtrics, Provo, UT, USA), a survey software program. Approval from the Institutional Review Board of Temple University was obtained prior to the start of the study. An invitation was sent to all the 633 ASOPRS members by using the society’s email database. A follow-up reminder email with the survey link was sent to all the members ~4 weeks following the first email. The anonymous survey consisted of a series of questions addressed to current oculoplastic surgeons regarding their management of nonoperative orbital fractures and the role of prophylactic antibiotics. Throughout the survey, there were multiple questions that allowed multiple answer choices to be selected and other open-ended questions. This anonymous survey was analyzed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). Descriptive statistics and analysis of variance were used to analyze the survey results.
Results
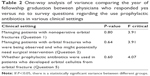
A total of 633 email requests were sent to ASOPRS members, and 164 responses were received. This represented an overall response rate of 25.9%. Of the 164 oculoplastic surgeons surveyed, 104 (63%) did not routinely give prophylactic antibiotics to patients with nonoperative orbital fractures (Table 1). There was no correlation between the year of fellowship graduation and the physician’s practice with regard to the use of prophylactic antibiotic in patients with nonoperative orbital fractures (Table 2). Also, 95 (58%) of oculoplastic surgeons did not routinely give prophylactic antibiotics to patients with orbital fractures whom the physicians were observing and who might potentially need surgical intervention (Table 1). Similarly, there was no correlation between the year of fellowship graduation and physician’s practice with regard to the use of prophylactic antibiotic in patients who might potentially need surgical intervention (Table 2).
  | Table 1 Summary statistics of survey questions |
Fifty-seven percent of current oculoplastic surgeons did not prescribe antibiotics for nonoperative orbital fractures (Table 1). Among those who do (43%), most (28%) preferred to prescribe a cephalosporin; the second most common choice of antibiotics is a penicillin derivative (13%) (Table 1). Among those oculoplastic surgeons who prescribe prophylactic antibiotics (41%), most oculoplastic surgeons prescribe prophylactic antibiotics for a period of 7–10 days (32%); and the second most common duration is 3–5 days (9%) (Table 1).
Seventy-four percent of current oculoplastic surgeons have never managed a case of orbital cellulitis following a nonoperative orbital fracture; among those who have (26%), 22% have done so when prophylactic antibiotics were not given, and 7% have done so when prophylactic antibiotics were given (Table 1). There is no statistically significant difference in the graduation year with regard to whether a given oculoplastic surgeon has used prophylactic antibiotics when managing a case of orbital cellulitis following a nonoperative orbital fracture or not (Table 2). Among the orbital fracture cases that led to orbital cellulitis, most of the fractures were located in the orbital floor (68%), with the medial wall being the second most common location (54%) (Table 1). Lateral wall and orbital roof fracture each comprised of 5% and 7% fracture cases that developed orbital cellulitis; additionally, 16% of the oculoplastic surgeons who were surveyed did not recall the location of the fracture. Among the possible risk factors for developing orbital cellulitis from orbital fracture, sinusitis was the most common (66%) risk factor for orbital cellulitis based on the experience of the oculoplastic surgeon and forceful nose blowing was the second most common (51%) (Table 1). Diabetes and an immunosuppressive state, which were mentioned in The Wills Eye Manual3 as a risk factor for developing orbital cellulitis, were seen as a risk factor by 27% and 20% of oculoplastic surgeons, respectively.
Among those who have managed orbital cellulitis following a nonoperative fracture (44 physicians), 80% of oculoplastic surgeons had patients who developed orbital cellulitis in <1% of fractures and 15% of surgeons had patients who developed orbital cellulitis in 1%–5% of orbital fractures (Table 1).
Discussion
Despite the common recommendation for prophylactic antibiotic use in orbital fractures in commonly cited references,3,5 the present study indicates that the majority of oculoplastic surgeons do not use prophylactic antibiotic in orbital fractures, regardless of whether they are treating a nonoperative orbital fracture or an orbital fracture that may potentially require surgery. The fact that among those who have managed orbital cellulitis following nonoperative fracture (44 physicians), 80% of the physicians have found that <1% of patients develop orbital cellulitis (Table 1) which supports the practice of not using prophylactic antibiotics in all nonoperative orbital fractures.
In one small, prospective trial, Chole and Yee reported no infections following maxillary, zygomatic, or subcondylar mandibular fractures regardless of antibiotic prophylaxis, suggesting that antibiotics are not indicated following these fractures.16 However, the study sample was very small, containing only 22 patients. There have not been any larger, randomized studies investigating the role of prophylactic antibiotics in preventing orbital cellulitis. A survey of British oral and maxillofacial surgeons demonstrated that there was no consensus about the use of prophylactic antibiotics for orbital blowout fractures, and a survey of American plastic surgeons also showed that there was no consensus regarding the use of prophylactic antibiotics for facial fractures.17,18
Finally, the knowledge of current management practices will assist us in determining the need for a large, multicenter study to determine the incidence and role of prophylactic antibiotics in preventing orbital cellulitis in nonoperative orbital fractures.
Given the inherent risks of antibiotics and the rare incidence of orbital cellulitis following an orbital fracture, it is reasonable to question the necessity of prophylactic antibiotics for nonoperative orbital fractures. Recall bias,19 which is inherent to this type of survey research, is one possible limitation of this study.
Conclusion
In summary, our study suggests that oral antibiotics are not necessary in the management of many patients with orbital fractures. In the posttreatment care of patients after an intravitreal injection, now the standard of care is to not give antibiotics.20 Likewise, perhaps the standard of care for the management of closed orbital fractures, as determined by the practice patterns of members of ASOPRS, should be to not give oral antibiotics.
Disclosure
The authors report no conflicts of interest in this work.
References
Yadav K, Cowan E, Wall S, Gennis P. Orbital fracture clinical decision rule development: burden of disease and use of a mandatory electronic survey instrument. Acad Emerg Med. 2011;18(3):313–316. | ||
Ko MJ, Morris CK, Kim JW, Lad SP, Arrigo RT, Lad EM. Orbital fractures: national inpatient trends and complications. Ophthal Plast Reconstr Surg. 2013;29(4):298–303. | ||
Gerstenblith AT, Rabinowitz MP. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 5th ed. Baltimore: Lippincott Williams & Wilkins; 2012:36. | ||
Joseph JM, Glavas IP. Orbital fractures: a review. Clin Ophthalmol. 2011;5:95–100. | ||
Kaiser PK, Friedman NJ, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 4th ed. New York, NY: Elsevier Health Sciences; 2014. | ||
Silver HS, Fucci MJ, Flanagan JC, Lowry LD. Severe orbital infection as a complication of orbital fracture. Arch Otolaryngol Head Neck Surg. 1992;118(8):845–848. | ||
Goroll AH, Mulley AG. Primary Care Medicine: Office Evaluation and Management of the Adult Patient. Philadelphia: Lippincott Williams & Wilkins; 2009. | ||
BenSimon GJ, Bush S, Selva D, McNab AA. Orbital cellulitis: a rare complication after orbital blowout fracture. Ophthalmology. 2005;112(11):2030–2034. | ||
Paterson AW, Barnard NA, Irvine GH. Naso-orbital fracture leading to orbital cellulitis, and visual loss as a complication of chronic sinusitis. Br J Oral Maxillofac Surg. 1994;32(2):80–82. | ||
Dhariwal DK, Kittur MA, Farrier JN, Sugar AW, Aird DW, Laws DE. Post-traumatic orbital cellulitis. Br J Oral Maxillofac Surg. 2003;41(1):21–28. | ||
Jayamanne DG, Bell RW, Allen ED. Orbital cellulitis – an unusual presentation and late complication of severe facial trauma. Br J Oral Maxillofac Surg. 1994;32(3):187–189. | ||
Shuttleworth GN, David DB, Potts MJ, Bell CN, Guest PG. Lesson of the week: Orbital trauma: do not blow your nose. BMJ. 1999;318(7190):1054–1055. | ||
Newlands C, Baggs PR, Kendrick R. Orbital trauma: antibiotic prophylaxis needs to be given only in certain circumstances. BMJ. 1999;319(7208):516. | ||
Davies J, Davies J. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74:417–433. | ||
Westfall CT, Shore JW. Isolated fractures of the orbital floor: risk of infection and the role of antibiotic prophylaxis. Ophthalmic Surg. 1991;22(7):409. | ||
Chole RA, Yee J. Antibiotic prophylaxis for facial fractures: a prospective, randomized clinical trial. Arch Otolaryngol Head Neck Surg. 1987;113(10):1055–1057. | ||
Courtney DJ, Thomas S, Whitfield PH. Isolated orbital blowout fractures: survey and review. Br J Oral Maxillofac Surg. 2000;38.5:496–503. | ||
Hauck RM, Nogan S. The use of prophylactic antibiotics in plastic surgery: update in 2010. Ann Plast Surg. 2013;70(1):91–97. | ||
Last JM. A Dictionary of Epidemiology. New York: Oxford University Press; 2000:153. | ||
Cheung CS, Wong AW, Lui A, Kertes PJ, Devenyl RG, Lam WC. Incidence of endophthalmitis and use of antibiotic prophylaxis after intravitreal injections. Ophthalmology. 2012;119:1609–1614. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.