Back to Journals » Integrated Blood Pressure Control » Volume 11
Potential use of a “Blood Pressure Action Sheet” for Indonesian patients with hypertension living in rural villages: a qualitative study
Authors Rahmawati R, Bajorek B
Received 20 September 2017
Accepted for publication 6 July 2018
Published 10 December 2018 Volume 2018:11 Pages 93—103
DOI https://doi.org/10.2147/IBPC.S152157
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Turgay Celik
Riana Rahmawati,1,2 Beata Bajorek1
1Graduate School of Health, Discipline of Pharmacy, The University of Technology Sydney, NSW, Australia; 2Pharmacology Department, Faculty of Medicine, Universitas Islam Indonesia, Yogyakarta, Indonesia
Purpose: The aim of the study was to obtain feedback on the layout, content, and potential use of a blood pressure (BP) action sheet, a purpose-designed written resource for Indonesian patients with hypertension.
Methods: Telephone interviews were conducted with 13 health professionals, 12 community health workers, and 12 patients in rural Yogyakarta, Indonesia, to explore their impressions of the BP action sheet, how the sheet might affect management of hypertension, and suggestions for improvement.
Results: Participants felt that the sheet presented useful information about achieving the target BP and managing hypertension. The use of the sheet could be optimized by engaging community health workers to help explain the information and to provide assistance around the stated actions for hypertension management. A more attractive design and inclusion of more details were suggested. Both patients and health care workers expressed interest in using the sheet.
Conclusion: The BP action sheet has potential as a useful resource for patients with hypertension by providing information, recording target BP, and facilitating patient-centered communication. Use of the BP action sheet might provide an effective low-cost way for health professionals and community health workers to encourage patients to achieve their target BP.
Keywords: hypertension, rural health, patient education, Posyandu lansia, Prolanis
Introduction
Hypertension has become a significant public health epidemic worldwide and is associated with an increased risk of numerous complications such as stroke, kidney disease, coronary heart disease and heart failure.1,2 In Indonesia, data from a national survey show that the prevalence of hypertension has increased from 8.3% in 1995 to 26.7% in 2013.3
Despite concerted efforts to improve the treatment of hypertension, less than 50% of patients with hypertension achieve their blood pressure (BP) target.1 The lack of adherence to a recommended treatment regimen is often reported as the main reason for poor control of BP in patients with hypertension.4,5 Studies have shown that patients’ inadequate knowledge and misbeliefs about hypertension underpin non-adherence to anti-hypertensive medications.6,7 Our previous study in rural villages in Yogyakarta province, Indonesia, demonstrated that patients with a good level of knowledge about hypertension are seven times more likely to adhere to their hypertension medication, compared to those with a low level of knowledge.8 To improve the patients’ knowledge, health care professionals (HCPs) should provide adequate information to their patients at each clinical encounter;9 however, HCPs’ workloads and time constraints often preclude effective verbal communication with patients.10 Furthermore, over time, patients tend to forget the information provided to them during consultations.11 Therefore, patients may be better informed through the provision of tangible resources, eg, written educational materials (eg, leaflets, brochures), as well as videos, mobile phones, and internet applications.12–14
Despite the advantages of using written educational resources to improve patients’ knowledge, a review of 19 non-internet-based leaflets on hypertension in the UK reported a lack of complete information within these leaflets; for instance, only seven clearly stated the importance of BP monitoring.15 To be effective, the development of written resources requires input and feedback from potential end-users (including patients) before distribution of the resources in clinical practice.16 In response to the findings of our previous studies,8,10,17 we have developed a purpose-designed written resource, the BP action sheet, to help Indonesian patients with hypertension. The aim of this study was to obtain feedback about the layout, content, and potential use of the sheet. Feedback was sought from a range of people who were likely to use the sheet: Indonesian people who have hypertension and who live in rural villages, HCPs in community health centers and community health workers in the villages.
Methods
Study design and setting
A qualitative study using telephone interviews was undertaken in two rural villages in the Bantul District of Yogyakarta province in Indonesia from December 2016 to January 2017. These villages were purposely selected because they are categorized as underdeveloped villages by the Bantul district government18 and because a survey of medication-taking practices had been previously undertaken in these rural villages. Two community health centers that provide health care services for people in the selected villages were also included in this study.
BP action sheet
Information and recommendations provided in the BP action sheet were developed based on our previous findings that identified some knowledge gaps among rural patients with hypertension and highlighted the need to improve patients’ access to information.8,17 The development of the sheet also considered both the Indonesian and international guidelines for hypertension,19,20 and the principles of designing effective written health education materials for patients.21–24 As a simplified informational leaflet, the BP action sheet was purpose-designed to:
- Convey the target BP for each patient;
- Present key information about hypertension;
- Describe the actions for patients to take to manage their hypertension; and
- Identify sources of support in the local setting to help patients manage their hypertension.
The BP action sheet comprises four A5-size pages in black and white print (available from the researchers on request). The first page includes the title “High blood pressure (Hypertension)”, the patient’s details (name, address, contact number), and a picture of an elderly couple saying “What should I know?” and “What should I do?” The second page provides space to record the patient’s BP readings and any actions to be taken (Figure S2). Space to record the patient’s BP target is located in the top right corner of this page. The third page provides key facts about hypertension as well as information about where patients can obtain support related to the specific actions described. The last page provides a flow chart describing the actions patients should take to achieve and maintain the target BP. The flow chart starts with the question “Have you achieved your target BP?” Based on the answer (Yes or No), a specific action is described (Figure S3).
Recruitment of participants
Three groups of participants took part in this study: patients, HCPs in the community health centers, and community health workers in the rural villages. Using purposive sampling, people who fulfilled the inclusion criteria (Table 1) were recruited. Participants’ contact details were obtained with consent via the local contact people (a dedicated person in each community health center, appointed by the head of the center). The local contact person distributed the invitation letter, provided a participant information sheet , and collated written consent from participants. Based on the expected number required to achieve theme saturation,25 it was estimated that 12 participants for each group (36 participants overall) were required.
  | Table 1 Inclusion criteria for study participants Abbreviation: HCP, health care professional. |
Data collection
The interviews were conducted in the Indonesian language by the lead researcher (an Indonesian) using a script for telephone interviews and a purpose-designed interview guide (Figure S1). The set of questions in the interview guide were pilot-tested prior to interviewing the main study participants. Before posing open-ended questions about participants’ perspectives on the BP action sheet, the researcher confirmed that each participant had reviewed the resource and was ready to provide feedback. The interview guide focused on participants’ first impression of the sheet, how the sheet might affect their management of hypertension and any suggestions for improvement to the sheet. Telephone interviews lasted 15–20 minutes per participant.
Data analysis
A pragmatic approach was applied in this study as it allows researchers to choose the technique that best addresses the central research question (ie, feedback on the BP action sheet for patients).26 The interview responses were digitally recorded (audio), transcribed verbatim (de-identified), and translated into English by an independent Indonesian translator; the translations were verified by the lead researcher. The data were then manually coded by two researchers using standard thematic analysis techniques.27 Each researcher independently coded and themed the data before a joint discussion among the researchers to ensure consensus. Inter-researcher theme validation was conducted by two independent researchers.
Ethical approval
Approval from the University of Technology Sydney Human Research Ethics Committee was granted to conduct this study (Ref. no. ETH16-0769). Approval from the Bantul District Government was also received (Ref. no. 070/Reg/3961/S3/2016).
Results
Characteristics of participants
Data saturation in each group was achieved after 8–10 interviews. However, all recruited participants were interviewed: 13 HCPs (three doctors, four nurses, four midwives, one pharmacy technician and one dietician); 12 community health workers; and 12 patients. The participants’ characteristics are presented in Table 2.
Themes
The following four themes emerged from the interviews:
- Benefits of the BP action sheet;
- Potential use of the BP action sheet;
- Optimizing the use of the sheet; and
- Suggestions for improvement.
Theme 1. Benefits of the BP action sheet
All participants regarded positively the potential benefits of the BP action sheet for improving patients’ knowledge of hypertension and its management. Compared with other written resources they had previously read, participants noted the strengths of the BP action sheet.
This (BP action sheet) is simple, but it’s interesting. There are so many leaflets with much content, but it’s difficult for us to read [them]. This one […] is easy to understand. [Patient 8]
There are some leaflets in Puskesmas [that are] quite similar, but they do not have the scheme as shown in this sheet. This scheme [on page 4] is easily understood [in terms of] what a patient should do. The other leaflets explain the information only in general. [HCP 5]
Patients will bring it home, right? The other leaflet is not usually used after being read. Some people may throw it [away], and the patients forget their previous BP level. [HCP 13]
Key facts and information, such as “Hypertension is treatable”, “Hypertension can cause stroke, heart attack, kidney and eye problems”, and “What patients should do”, were regarded by patients as the most important and interesting aspects of the sheet.
I feel happy, for being informed about hypertension so that I do not need to worry. It mentions [here], “hypertension is treatable.” [Patient 8]
This one [is the most interesting]: hypertension can cause stroke [or] heart attack. I am afraid of these risks. [Patient 3]
Certain information, such as the need to take medications routinely over the long term, was considered to be new information and provided new insights for patients and community health workers.
[…] What I previously believed was that, I need to take medications after visiting the clinic or only when feeling sick. Now I know more about taking the medication, which means that I need to make friends with [hypertension] medications. [Patient 3]
‘Taking medication at the same time each day’ – we did not know this before. My husband has high BP, and he usually takes the medication in the morning or in the evening. So, after reading this leaflet, I know that taking medication should be at the same time. [Community health worker 8]
Some HCPs appreciated that the BP action sheet addressed common misconceptions about hypertension medications among their patients and emphasized the importance of this information.
Well, I like this one: “Hypertension often shows no signs or symptoms.” This is good, to raise the patient’s awareness that the BP check does not need to wait for symptoms [to appear]. Because many of our patients do that. They wait for the symptoms to occur or worsen. If the symptoms do not occur, they think that they are healthy. [HCP 1]
So, they [patient] think that all kinds of medicines can damage the kidneys. In fact, [as mentioned in the BP Action Sheet] hypertension can cause kidney problems if it’s not well treated [but] lay people often think the opposite. [HCP 12]
The HCPs and community health workers also agreed that the sheet would help them explain hypertension to patients.
In my opinion, we can use it for health education. It will be very useful since many people are recently diagnosed with hypertension. Most older people who visit Posyandu lansia [Integrated Health Service Post for Elderly) have high blood pressure. [Community health worker 1]
I think HCPs need to explain it, well […] for example, explain the [“What should I do?”] schemes. [HCP 2]
Patients, HCPs, and community health workers agreed that the content on the second page (presenting an individualized target BP, recording BP readings and actions to be taken) enabled the BP action sheet to function as a personal health record. In addition, they mentioned that the BP action sheet is user-friendly, and this was perceived as a strength of the sheet.
It is good […] because it mentions the target blood pressure. I think most of the leaflets do not include this information, so this leaflet [BP action sheet] is much better […] more real […] more functional […] and more personal, because each patient is different. [HCP 8]
We have a health card for the elderly, but we do not use it. We record the result of each patient’s blood pressure check in our book [because] the font in the card is too small, a lot of columns […]. It is not simple. On the other hand, this sheet can be filled in easily. [Community health worker 8]
Theme 2. Potential use of the BP action sheet
Both patients and health care workers mentioned the importance of patients bringing the BP action sheet to their HCP appointments or when having their BP checked by community health workers. They also agreed that both HCPs and community health workers could record important information on the sheet. For this reason, there was much interest in making copies of the sheet available for their immediate use in practice.
This sheet will be brought [in] by patients. It can be used as a follow-up […]. For further steps, I think it can become a program [for Puskesmas]. It is probably beneficial in Puskesmas. We can copy this sheet to be distributed to patients. [HCP 13]
I can copy the sheet and distribute it to patients with high blood pressure. We will tell them that they must bring the sheet to every Posyandu meeting. [Community health worker 4]
Can I copy this by myself? I will also copy it for my neighbors because there are some people with hypertension around here […] let me give this to them. [Patient 9]
Both HCPs and community health workers believed that the Posyandu lansia (Integrated Health Service Post for the Elderly, a community health worker-based program for the elderly) would be an ideal place for distributing the sheet to patients because this program is well established in all villages (in the study location). As confirmed by participants, the Posyandu lansia uses local villagers as community health workers who provide BP checks for the elderly at least once every 1–3 months.
I really believe that, in my Posyandu lansia, patients will be happy to bring this [BP action] sheet to the Posyandu. [Community health worker 7]
To use this sheet […] patients will bring this […] but, most of them are the elderly, and they need assistance. This is done best by community health workers in the Posyandu lansia [where] they can check [the patient’s] BP. They can also read the information to the patients. I think if we do not read this to elderly patients, they will not read [it themselves]. [HCP 9]
HCPs also explicitly mentioned the Prolanis program, a newer program for patients with hypertension and/or diabetes mellitus treated in the community health centers, as another portal for disseminating the BP action sheet.
We monitor patients [in the Prolanis program], primarily using medical records, so, for me, this sheet will help the patients [members of Prolanis] to see how, after getting a medication, they [can] achieve their target BP. [HCP 12]
Theme 3. Optimizing the use of the BP action sheet
Although most participants noted that the information in the sheet is easily understood, a few suggested the need for additional verbal explanations of the content and how the sheet should be used. The HCPs expressed the need for assistance from community health workers, not only in distributing the sheet but also in helping HCPs to explain to patients the information contained within it. The HCPs conveyed their appreciation of the ability of community health workers to provide information using lay language so that is easily understood by patients, particularly older persons with limited reading skills. It was also agreed that community health workers could support BP checking and recording of results on the sheet.
For this sheet, we will ask community health workers to provide information to patients about it. The main point is information […] the community health workers have important roles because they are in the front line. I usually ask for their help for health education. […] So, they will inform the patients, […] they know the local language better than we do. [HCP 11]
First, we need to give […] general information about hypertension. So, when we distribute the sheet, we start the explanation from the first page, followed by filling in the personal identity, and then going to the next page to write down their BP reading. [Community health worker 10]
In addition, the community health workers noted that verbal explanations also can be provided by family members to help patients understand the information contained in the sheet.
We will ask for help from their family. When we explain it [the sheet], their children are there. It is hoped that they can also explain the information to their parents when they are at home. [Community health worker 11]
Theme 4. Suggestions for improvement
Most participants stated that the design of the sheet was satisfactory, although others suggested using a colored version of the BP action sheet to attract more attention, and adding arrows in the flowchart for clarity.
It is cool […] really cool […] and interesting. The pictures are also interesting […]. Although it has black and white pictures, it is [still] interesting […]. The recent KMS [health card] is colorful, but when we copy it, it becomes less interesting. [HCP 5]
I think colorful leaflet will be much better […] just to make it [the sheet] more interesting […] because older persons usually have sight problem […] [Community health worker 11]
Overall, the responses regarding the content within the sheet were positive. Most patients felt that the information in the sheet was comprehensive. However, some HCPs and community health workers suggested that information about the role of traditional medicines and diet in the management of hypertension should be added to the BP action sheet. Other suggestions were to include information about symptoms, risk factors, and classification of hypertension (Table 3). In addition, half of the HCPs suggested clarifying the information about access to medication (free-of-charge) through the Prolanis program, requesting that eligibility criteria be briefly described.
  | Table 3 Selected quotes expressing patients’ suggestions about items that could be added to the Blood Pressure Action Sheet Abbreviation: HCP, health care professional. |
Discussion
This study describes the feedback obtained about a new written educational resource for Indonesian patients titled the BP action sheet. Overall, the sheet was perceived positively as both a source of information for patients with hypertension and as a tool for monitoring their progress toward achieving the target BP.
To encourage people to become actively involved in the self-management of their high BP, they need adequate and appropriate information addressing issues such as monitoring of BP, taking medication, managing diet, undertaking physical activity, and controlling stress.28 Although systematic reviews29,30 have reported the potential of mobile phone messaging to improve patients’ adherence to medications, people living in low-resource settings have experienced difficulties in adopting and using such technology-based information services.31 In one study involving 75 Indonesian patients with hypertension, short message service reminders were reported to have no significant impact on medication adherence.32 Despite technological advances, written educational resources remain a primary modality for information provision and are considered to be an effective and efficient method in providing information to literate patients and as a complement to information delivered directly by HCPs.33 Nevertheless, it is essential that the information in the resources is suited to the target patients and is written in understandable language.21,22 To improve its readability, a written educational resource should be presented at a literacy level that is no higher than eighth-grade school level or at the sixth-grade level for patients with low health literacy.34 However, the current instruments for assessing readability, such as the Flesch–Kincaid grade,35 were developed primarily for English language resources.36 Therefore, in our study, we used qualitative feedback from potential end users, including patients, to assess the perceived suitability of the information sheet for the target recipients (ie, rural Indonesian patients). As a source of information, the sheet was perceived as being accurate, comprehensive, and easily understood by patients in this study. The strength of the BP action sheet is that the information contained therein is a response to the findings from previous studies in a similar study setting.8,10,17 In addition, as a four-page A5-size leaflet, it is simple and inexpensive to reproduce; it costs less than USD$0.2 to print a paper copy of the sheet.
The BP action sheet also has potential as a BP monitoring tool for patients. It is a concern that patients often rely on the appearance of symptoms rather than objective BP readings as an indicator of the need to take treatment.7,10 Therefore, each patient’s target BP should be recorded and documented.37 The BP action sheet includes space to record the patient’s BP which is intended to provide timely information for both the patient and HCP about the patient’s progress in achieving the target BP. Requiring each patient to bring the BP action sheet to each visit to the HCP will hopefully trigger discussions about whether the target BP has been met and, if not, strategies to address this. The written recommendation in terms of action needed to achieve the target BP can be provided individually for each patient, which means that the sheet may facilitate communication between HCPs and patients. In addition, as a BP monitoring tool, patients will need to regularly interact with the BP action sheet and they will be less inclined to discard the sheet. This is important because a written resource such as a leaflet is often thrown away after reading.38
This study found that there is potential for involving community health workers and family members in optimizing the use of a written educational resource such as the BP action sheet. Support from community health workers in providing accessible BP checks and information for rural Indonesian people with hypertension has been reported.39,40 It is expected that community health workers would distribute the BP action sheet to rural patients in the study setting, explain the information contained in the sheet, record the BP reading, give advice to patients, and refer them to an HCP when necessary. To improve patients’ adherence to the hypertension treatment plan, previous studies have also reported the importance of functional support from family members.41 Family members may help patients to understand the information contained in the resource and to put into practice the recommendations provided by the HCPs. The opportunity to re-read the information contained in the BP action sheet, including written recommendations from HCPs and community health workers, might improve patients’ understandings about their condition and encourage them to have their BP adequately treated. Because the community health workers can also access the HCPs’ recommendations and refer patients to HCPs, the sheet also may enhance patient-centered communication involving HCPs, community health workers, family members, and patients.
This study suggests that it may be feasible to implement the BP action sheet in programs for rural Indonesian patients, particularly through the existing hypertension programs in the community such as the Posyandu lansia or Prolanis. The Prolanis program is integrated into routine primary health care and offers comprehensive approaches to managing hypertension such as monthly BP checks, health education, physical exercise, medication (free-of-charge), home visits, and referrals to specialists.42 As a simplified information resource and personal BP record, the BP action sheet has potential benefits for members of Prolanis that could complement its existing approaches. Integrated interventions comprising patient education, behavioral support and case management that are offered in this program might lead to greater improvements in medication adherence, a cornerstone of achieving BP control.43 Further studies are needed to evaluate the impact of the BP action sheet in objective, quantitative measures (eg, BP reading, level of adherence to medication), and there are opportunities to do so through the existing hypertension programs in Indonesia.
Conclusion
Positive feedback from patients and health care workers in rural villages indicates that the BP action sheet has the potential to improve patients’ knowledge about hypertension and to facilitate better monitoring of BP toward achievement of the target range. The BP action sheet may serve as an affordable and practical tool for patients, HCPs, and community health workers alike in supporting efforts to manage hypertension among people in low-resource settings. Support from HCPs, family members, and community health workers is required to optimize the practical use of the BP action sheet by patients. Further refinement is required before the sheet can be piloted in the clinical practice setting.
Providing the BP action sheet to patients would require them to bring the sheet to each health care visit. This tailored sheet is not only an information source for patients; but also may be used as a BP monitoring tool and an enabler of communication between HCPs, patients and community health workers. Further studies are needed to assess how these functions may improve patients’ adherence to hypertension treatment and the achievement of BP target. As a low-cost strategy, the sheet has the potential to support hypertension programs for patients in low-resource settings. Because patients in such settings often present challenges to visiting HCPs, providing accessible and affordable health care services is crucial for encouraging patients to have their BP checked and treated.
Acknowledgments
The authors would like to thank the Bantul district government and the head of participating community health centers for the opportunity to perform this study. Our special gratitude goes to the rural villagers, community health workers and health care professionals in the community health centers who participated in the study. We also would like to thank Erna Andriyanti and Haira Rizka for translating the interviews.
Author contributions
RR collected the data, analyzed and interpreted the findings, wrote and organized manuscript. BB contributed to the idea, manuscript drafting, interpretation of findings, and critical review of the manuscript. Both authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The first author was supported by the Directorate General of Higher Education (DIKTI) Indonesia (Grant number 2925/E4.4/K/2013) for her PhD study at the University of Technology Sydney. The second author reports no conflicts of interest in this work.
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. | ||
World Health Organization (WHO). Global health risks: mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization; 2009. | ||
Ministry of Health Republic of Indonesia. Riset Kesehatan Dasar (Basic Health Research). National Board of Health Research and Development. Indonesia: Ministry of Health Republic of Indonesia; 2013. | ||
Sabate E. Adherence to Long-term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. | ||
Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. | ||
Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: A review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–286. | ||
Marshall IJ, Wolfe CD, Mckevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ. 2012;345:e3953. | ||
Rahmawati R, Bajorek B. Factors affecting self-reported medication adherence and hypertension knowledge: A cross sectional study in underdeveloped villages, Yogyakarta province, Indonesia. Chronic Illn. 2018;14(3):212–227. | ||
Bastable S, Gramet P, Jacobs K, Sopczyk DL. Health Professional as Educator: Principles of Teaching and Learning. Burlington, MA: Jones & Bartlett Learning; 2010:42–45. | ||
Rahmawati R, Bajorek B. Perspectives on antihypertensive medication: a qualitative study in a rural Yogyakarta province in Indonesia. Drug Ther Perspect. 2016;32(2):76–83. | ||
Kessels RP. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–222. | ||
Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(Suppl 3):30–54. | ||
Sun N, Rau P-LP, Li Y, Owen T, Thimbleby H. Design and evaluation of a mobile phone-based health intervention for patients with hypertensive condition. Comput Human Behav. 2016;63:98–105. | ||
Ajay VS, Jindal D, Roy A, et al. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: The mPower Heart Project. J Am Heart Assoc. 2016;5(12): e004343. | ||
Fitzmaurice DA, Adams JL. A systematic review of patient information leaflets for hypertension. J Hum Hypertens. 2000;14(4):259–262. | ||
Raynor DK, Blenkinsopp A, Knapp P, et al. A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines. Health Technol Assess. 2007;11(5):1–160. | ||
Rahmawati R, Bajorek B. Understanding untreated hypertension from patients’ point of view: A qualitative study in rural Yogyakarta province, Indonesia. Chronic Illn. 2018;14(3)228–240. | ||
Bantul District Government. Bantul – The Harmony of Nature and Culture (Database Profile of the Bantul District). Regional Planning Body, Government of Bantul District, Yogyakarta, Indonesia: 2013. | ||
Ministry of Health Republic of Indonesia. Technical Guideline of Screening and Management of Hypertension (Pedoman Teknis Penemuan Tatalaksana Penyakit Hipertensi). Jakarta, Indonesia: Ministry of Health; 2013. | ||
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. | ||
Stonecypher K. Creating a patient education tool. J Contin Educ Nurs. 2009;40(10):462–467. | ||
Shoemaker SJ, Wolf MS, Brach C. Development of the Patient Education Materials Assessment Tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns. 2014;96(3):395–403. | ||
Hoffmann T, Worrall L. Designing effective written health education materials: considerations for health professionals. Disabil Rehabil. 2004;26(19):1166–1173. | ||
van Beusekom MM, Grootens-Wiegers P, Bos MJ, Guchelaar HJ, van den Broek JM. Low literacy and written drug information: information-seeking, leaflet evaluation and preferences, and roles for images. Int J Clin Pharm. 2016;38(6):1372–1379. | ||
Trotter RT 2nd. Qualitative research sample design and sample size: resolving and unresolved issues and inferential imperatives. Prev Med. 2012;55(5):398–400. | ||
Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage Publications; 2013:9–11. | ||
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. | ||
Bosworth HB, Powers BJ, Oddone EZ. Patient self-management sup-port: novel strategies in hypertension and heart disease. Cardiol Clin. 2010;28(4):655–663. | ||
Adler AJ, Martin N, Mariani J, et al. Mobile phone text messaging to improve medication adherence in secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;4:CD011851. | ||
Ershad Sarabi R, Sadoughi F, Jamshidi Orak R, Bahaadinbeigy K. The effectiveness of mobile phone text messaging in improving medication adherence for patients with chronic diseases: a systematic review. Iran Red Crescent Med J. 2016;18(5):e25183. | ||
Salemink K, Strijker D, Bosworth G. Rural development in the digital age: A systematic literature review on unequal ICT availability, adoption, and use in rural areas. J Rural Stud. 2017;54:360–371. | ||
Nur’aeni MA, Fungie G. The effect of giving short message service reminder on adherence and the effectiveness of treatment on patients with hypertension in District Health Centre Sumbang Banyumas (in Bahasa). Media Farmasi. 2016;13(1):100–109. | ||
Wilson EA, Makoul G, Bojarski EA, et al. Comparative analysis of print and multimedia health materials: a review of the literature. Patient Educ Couns. 2012;89(1):7–14. | ||
Institute of Medicine (US) Committee on Health Literacy. A prescription to end confusion. Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Washington, DC: National Academies Press; 2004. | ||
Friedman DB, Hoffman-Goetz L. A systematic review of readability and comprehension instruments used for print and web-based cancer information. Health Educ Behav. 2006;33(3):352–373. | ||
Badarudeen S, Sabharwal S. Assessing readability of patient education materials: current role in orthopaedics. Clin Orthop Relat Res. 2010;468(10):2572–2580. | ||
Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289(19):2560–2572. | ||
Raynor D, Knapp P. Do patients see, read and retain the new mandatory medicines information leaflets? Pharm J. 2000;264(7083):268–270. | ||
Rahmawati R, Bajorek B. A community health worker-based program for elderly people with hypertension in Indonesia: A qualitative study, 2013. Prev Chronic Dis. 2015;12:140530. | ||
Krishnan A, Ekowati R, Baridalyne N, et al. Evaluation of community-based interventions for non-communicable diseases: experiences from India and Indonesia. Health Promot Int. 2011;26(3):276–289. | ||
Magrin ME, D’Addario M, Greco A, et al. Social support and adherence to treatment in hypertensive patients: a meta-analysis. Ann Behav Med. 2015;49(3):307–318. | ||
Badan Penyelenggara Jaminan Sosial. Practical Guideline of Prolanis (in Bahasa). Jakarta, Indonesia; 2015. Available from: https://bpjs-kesehatan.go.id/bpjs/dmdocuments/06-PROLANIS.pdf. Accessed March 15, 2017. | ||
Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper PS. Interventions to improve medication adherence in hypertensive patients: Systematic review and meta-analysis. Curr Hypertens Rep. 2015;17(12):94. |
Supplementary materials
  | Figure S1 Interview guide. |
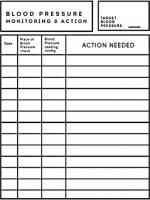  | Figure S2 The Blood Pressure Action Sheet (page 2). |
  | Figure S3 The Blood Pressure Action Sheet (page 4). |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

