Back to Journals » Clinical Ophthalmology » Volume 12
Postoperative outcomes following trabeculectomy and nonpenetrating surgical procedures: a 5-year longitudinal study
Authors Jiang L, Eaves S, Dhillon N, Ranjit P
Received 20 January 2018
Accepted for publication 15 March 2018
Published 25 May 2018 Volume 2018:12 Pages 995—1002
DOI https://doi.org/10.2147/OPTH.S163247
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Li Jiang, Scott Eaves, Navpreet Dhillon, Punithawathy Ranjit
Ophthalmology Department, University Hospitals of North Midlands NHS Trust, Stoke-on-Trent, UK
Purpose: To assess and compare the long-term postoperative outcomes of trabeculectomy (TE), phacotrabeculectomy (PTE), and viscocanalostomy (VC) and to correlate postoperative intraocular pressure (IOP) with visual outcome.
Patients and methods: This retrospective cohort observational study included 520 eyes which underwent TE with mitomycin C (MMC) (n=205), PTE with MMC (n=189), and VC ± combined cataract surgery and MMC (n=126) to control IOP between June 2010 and June 2014 by a single surgeon. Complete success was defined as postoperative IOP <20 mmHg, and qualified success with IOP <20 mmHg with single topical agent. Cases requiring more than one topical agent and/or repeat surgery were considered as failure. Mixed linear regression models were constructed to determine estimated predictive values of demographic data, topical prescriptions, baseline and postoperative IOP, and optical assessment (ie, best-corrected visual acuity and mean deviation) profile.
Results: Follow-up ranged from 12 to 66 months (mean 26 months). At last follow-up, 139 (93.9%), 118 (91.5%), and 98 (94.2%) eyes achieved complete success in TE, PTE, and VC groups, respectively (p=0.0007). Failure rates were 2.7%, 3.9%, and 2.9% following TE, PTE, and VC, respectively (p=0.0052). The between-group difference of mean IOP reduction was greater in the short term (p=0.0002). Good postoperative IOP control correlates to optical outcomes reflected by best-corrected visual acuity and mean deviation following TE (β = -4.7577, p=0.0384) and PTE (β = -4.5083, p=0.02741).
Conclusion: Significant association was observed between good postoperative IOP control and optical outcome. TE remains the more effective surgical intervention for sustained lowering of IOP. Most complications were transient and self-limiting.
Keywords: traveculectomy, viscocanalostomy, intraocular pressure, postoperative outcome
Introduction
Cataract and glaucoma are leading causes of blindness in Western developed countries1,2 and may frequently coexist in the same eye.3 In the UK, 30% of people over the age of 65 were found to have a visually impairing cataract in one or both eyes.4 The overall prevalence of glaucoma is 2% in people over the age of 40 and is estimated to rise to almost 10% in people over 75.5 The population aged over 40 in England is 24.4 million, and it is estimated that 489,000 people are affected with chronic open-angle glaucoma in England.6
Glaucoma treatments are directed at the pharmacological or surgical reduction of intraocular pressure (IOP).7,8 Surgery is performed when IOP medication and laser treatment cease to control IOP.9 Trabeculectomy (TE) provides excellent reduction of IOP and is the reference technique in the surgical treatment of glaucoma.10 Treatment for patients with concurrent cataract and glaucoma includes sequential surgery and combined phacotrabeculectomy (PTE).11 Combined surgery reduces the risk of an additional intraocular surgery that is associated with postoperative progression of lens opacities12 and reduces the risk of TE failure associated with sequential cataract surgery.13
Nonpenetrating glaucoma surgeries (NPSs) such as viscocanalostomy (VC) have been developed as a safer and more acceptable surgical intervention to patients compared to conventional procedures. This relatively new surgical procedure aims to restore the natural outflow pathway of aqueous humor through Descemet’s membrane into Schlemm’s canal with viscoelastic augmentation.14 Currently, there is some evidence to demonstrate that TE offers more effective IOP control than nonpenetrating filtration surgery.15
TE is associated with a higher incidence of complications when compared with NPS procedures.16 However, long-term comparative data for TE alone, combined PTE with or without intraoperative mitomycin C (MMC), and VC beyond 6 month are still lacking. The success rate and information on incidence of postoperative complications are also unclear.
This study aims to assess and compare the long-term postoperative outcomes of TE, PTE, and VC with or without combined cataract surgery in a multiethnic British population, and to evaluate the success rate of each procedure. Further analysis was performed on the correlation between the success rate of each procedure and postoperative IOP, best-corrected visual acuity (BCVA, logMAR), and mean deviation (MD) on standard Humphrey visual field testing 24-2.
Patients and methods
This was a retrospective case note review of 520 eyes from 438 patients who had undergone TE with MMC (205 eyes; group 1), PTE with MMC (189 eyes; group 2), and VC with or without combined cataract extraction and MMC augmentation (126 eyes; group 3) to control IOP at University Hospital of North Midlands NHS Trust in the United Kingdom between June 1, 2010, and June 30, 2014 (60-month period). All surgeries were performed by a single surgeon. This study has been approved by the review board at the University Hospital North Midlands Clinical Audit Team. Potential participants are presented (either verbally or in writing) with the same information required in a written consent document, but documentation of the process (signing of the consent form) was waived by the Institutional Review Board. The use of protected health information when conducting this research is in accordance with the Privacy Rule of the Health Insurance Portability and Accountability Act.
The inclusion criteria for our study were as follows:
Diagnosis of primary open-angle glaucoma and primary angle closure glaucoma (PACG).
No previous glaucoma surgery.
IOP measured with Goldmann applanation tonometry.
Completed at least 1 year of follow-up duration postoperatively.
The exclusion criteria were secondary etiology such as traumatic, neovascular, exfoliative, pigmentary, congenital, and uveitic glaucoma.
All surgeries were performed by a single surgeon. The type of anesthetic was determined by patient suitability, and the procedure(s) were carried out under general or local anesthesia. TE with MMC was performed with a fornix-based conjunctival flap, followed by application of MMC (0.2 mg/mL) for 3 minutes under the conjunctiva posteriorly. The wound was then irrigated with balanced salt solution. A 4×4 mm2 scleral flap was made and extended up to the clear cornea. Two releasable 10-0 nylon sutures were placed before entering the anterior chamber. TE was done using a diamond blade followed by closure of the scleral flap and conjunctiva with 10-0 monofilament nylon sutures. Postoperatively, all patients received topical 0.5% chloramphenicol, 1% prednisolone acetate, and 1% cyclopentolate. In combined PTE, phacoemulsification and intraocular lens implant was performed through a separate corneal tunnel incision.
In VC, a fornix-based conjunctival flap was fashioned followed by application of MMC (0.2 mg/mL) for 3 minutes under the conjunctiva posteriorly. A one-third thickness scleral flap was raised extending the clear cornea. A deep scleral flap was made 1 mm inside this flap and extended to the scleral spur. Schlemms canal was deroofed while extending the deep flap and further extended through the clear cornea leaving a window of Descemet’s membrane. Dilatation of cut ends of Schlemms canal was performed with Healon GV after the deep sclerectomy. The superficial flap was sutured with 10/0 Vicryl or 10/0 nylon and viscoelastic was then injected into the subscleral space. In the combined procedure, phacoemulsification of cataract with implantation of intraocular lens was completed through a separate corneal tunnel.
Medical records were retrospectively reviewed and relevant data were transferred to a standardized form which included patient demographic information, type of glaucoma, and intraoperative information. Preoperative and postoperative data were collected for change in IOP, BCVA (logMAR), stabilization of MD on visual field testing, number of topical medications, incidence of postoperative complications, and additional surgical interventions required.
The main outcome measure was success rate of procedure, as determined by IOP goals, postoperative number of topical medications, and further surgery. Complete success was defined as postoperative IOP control of <20 mmHg and/or 20% reduction from baseline, whereas qualified success was defined as postoperative IOP control of <20 mmHg with single topical agent. Cases requiring more than one topical agent and/or repeat surgery were considered as failure. Statistical differences across all three surgical subgroups were calculated using the one-way analysis of variance.
Postoperative complications were stratified into early (<1 month), late (>1 month), or recurrent (occurring more than once after surgery). Hypotony was defined as shallow anterior chamber with choroidal effusion on one or more occasions after surgery, and considered prolonged if it persisted for more than or equal to 2 weeks. Bleb leak was defined as either a positive Siedel’s test or visible conjunctival leak after surgery.
Statistical analysis
Statistical analysis was performed using MATLAB R2013b (The Mathwork, Natick, MA, USA). Between-group comparisons were performed using independent t-tests for normally distributed continuous variables, while a corresponding nonparametric test was used for nonnormally distributed samples. For categorical variables, Pearson’s χ2 test or Fisher’s exact test was performed. Multivariate logistic regression (including demographic information, use of topical medication, preoperative variance) was performed for postoperative profiles that included three factors, IOP, BCVA, and MD. A similar model was constructed for comparing TE, PTE, and VC groups. Kaplan–Meier survival analysis and the log-rank test were performed for the time to complete and qualified and failed success rates. A p-value of <0.05 was considered statistically significant. Mixed linear regression models were constructed to determine estimated predictive values of demographic data, use of topical agents, baseline and postoperative IOP, and optical (ie, BCVA and MD) profile.
Results
A total of 520 operations were performed on 438 patients between June 1, 2010, and June 30, 2014 (60-month period). Of these, 139 (26.7%) were excluded due to the following reasons: postoperative follow-up duration of <1 year (n=114, 21.9%), previous glaucoma surgery (n=1, 0.2%), and secondary glaucoma (n=24, 4.6%). Table 1 presents comparable baseline demographic data and duration of follow-up. The mean follow-up was 2 years (12–60 months). Among the 13 patients who underwent TE with a diagnosis of PACG, 10 were narrow angles with or without preceding cataract surgery.
Table 2 compares the success rates after TE, PTE, and VC as determined by IOP threshold (20 mmHg), need of postoperative topical agents, and necessity for redo surgery. Complete success rate at last follow-up was significantly higher in both TE and VC groups, compared with PTE. Likewise, the rate of cases requiring single topical agent to achieve target IOP threshold (20 mmHg) was significantly higher in the PTE group compared to TE and VC groups (p=0.0012). Results on the subgroup of PACG patients were nonsignificant. Kaplan–Meier survival analysis was performed to assess the success rates of all three groups. There was limited difference (p=0.0052) between the cumulative incidence of failure between TE (2.7%), PTE (3.9%), and VC (2.9%).
Presenting mean IOP did not differ significantly (Table 1). Preoperative baseline mean IOP was lower in VC group (20.2 mmHg) compared to TE (23.2 mmHg) and PTE (23.4 mmHg) groups (p=0.0199). Postoperatively, IOP values reduced significantly in all three surgical groups (Table 3). After TE surgery, patients showed stable IOP values spanning year 1 (12.8 mmHg, p=0.0002) to year 4 (13 mmHg, p=0.0134). The between-group difference of reduction in mean IOP was more significant in the short term compared to long term. Patients undergoing PTE and VC surgeries also demonstrated sustained, but less IOP-lowering effects, when compared to TE group in both the short term (r[PTE] = −1.8 mmHg, r[VC] = −2.5 mmHg at 1-year follow-up; p=0.0021) and long term (r[PTE] = −1.9 mmHg, r[VC] = −3.6 mmHg at 4-year follow-up; p=0.0134).
There was significant difference in baseline BCVA between the three groups (p=0.0009). Postoperatively, the TE group demonstrated stable BCVA up to 2 years after the surgery, and advancing profile thereafter likely due to accelerated cataract formation, corresponding to worsening of MD measurement beyond 3 years (Table 3). As expected, patients demonstrated stable optical performance following PTE in the long term, with immediate transient reduction postoperatively (p=0.0289). VC was also associated with significant stabilization of BCVA in the long term.
The difference in preoperative visual field performance may be attributed to cataracts in PTE group (p=0.0176). Table 4 presents descriptive information on MD values following surgery. Changes in MD from preoperative baseline to 3-year postoperatively were −1.69 following TE, −2.48 following PTE, and +0.57 following VC (p=0.0302).
Hypotony was observed in all three surgical groups, in association with other simultaneous complications such as temporary choroidal effusion, but no persistent choroidal detachment was observed. Laser suture lysis was performed as necessitated by IOP and condition of bleb. For eyes that required operations to reduce the IOP after the initial TE with MMC, alternatives such as subconjunctival needle revision with 5-fluororacil was performed in 24 cases, with five cases requiring more than one subconjunctival needle revision with 5-fluororacil. 19 (12.8%), 8 (6.2%), and 4 (3.9%) patients required at least one surgical intervention postoperatively following TE, PTE, and VC, respectively. One phacoemulsification-related intervention was performed (lens repositioning, 0.8%). Four patients (3.9%) required YAG laser goniopuncture following VC surgery. One case of endogenous endophthalmitis was observed following TE surgery, with complete recovery postvitrectomy and satisfactory visual outcome.
Within the VC group, 20 underwent VC alone and 106 combined phacoviscocanalostomies. Baseline visual acuity was poorer in combined phacoviscocanalostomies group (mean 0.73 LogMAR) compared to VC alone.
Mixed linear regression models were constructed to determine estimated predictive values of attributes including age, use of topical medication, and preoperative baseline and postoperative IOP profile and outcome of optical assessments (ie, BCVA and MD). Presenting demographic (age, gender) and ocular characteristics (use of topical agents, profile of IOP, BCVA, and MD) were not statistically significant, likely due to immense variability. Calculated data beyond 1-year follow-up were unreliable, and thus discarded due to insufficient follow-up for time series analysis. Estimates of meaningful effect based on the β values from regression indicates that good postoperative IOP control was associated with BCVA postoperatively in TE group (β = −4.7577, p=0.0384) and PTE group (β = −4.5083, p=0.02741) (Table 4). No significant correlation was demonstrated in VC group. T-statistic for each coefficient and p-value for the F statistic were calculated to test the null hypothesis that the corresponding coefficient was 0 against the alternative that it is different from 0, given the other predictors in the model.
Discussion
TE, combined PTE, and VC are commonly performed surgeries in patients with glaucoma with or without concurrent cataract. Patients in this study achieved better IOP control following TE surgery with fewer topical medications and superior visual field performance during the first 5 years. We found that TE surgery carries a higher risk of immediate postoperative complications and more frequent subsequent surgical interventions. In our study, the commonest postoperative complications up to 5 years were transient hypotony without persistent choroidal detachment, hyphema, and shallow anterior chamber, respectively (Table 5).
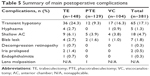  | Table 5 Summary of main postoperative complications |
As “regression to the mean” may account for the supposed IOP reduction, linear regression of first and second postoperative data points were considered to avoid making incorrect inferences. The variance of efficacy estimates is reduced by practice effect, as this study was performed at a single center and all operations were carried out by the same experienced surgeon. While this increases the sensitivity of the study to between-group differences, it may also limit the extrapolation of the results, and so further multicenter studies are required.
The results of this study are comparable with other large studies, Broadway et al17 reported success rate at 6 years after TE of 93%, comparable to our finding of 93.9%. Lochhead et al18 and Chang et al19 both observed better IOP control with TE alone compared to PTE, similar to our study. From a biological plausibility perspective, anterior chamber inflammation that is associated with cataract extraction may be associated with inflammatory material (eg, lens proteins, etc) could immediately pass through sclerostomy and into subtenon space causing early postoperative fibrosis.20 Furthermore, Cheng et al21 observed primary VC to significantly lower IOP with fewer complications than TE. However, they also report VC to be less effective than TE, with comparative figures to our study. Husain et al22 observed worsening of their lens opacities (by LOCS III units) in 66% of subjects at 3 years follow-up TE, in keeping with our finding of significant deterioration in BCVA and MD beyond year 3 postoperatively in our cohort of patients undergoing TE.
IOP control and visual improvement were persistently superior in TE group when compared with PTE and VC over a 5-year period. The difference between TE and PTE groups may be explained by TE patients receiving more topical medication preoperatively and some having undergone previous cataract extraction. Postoperative IOP values were independent of preoperative baseline values in all three surgical groups suggesting that even severe cases with deviated preoperative baseline profile could benefit from such treatment and achieve target IOP control in the long term. Bleb features vary considerably over the first 6 months postoperatively, and hence the variability was noted in the remodeling phases when the bleb retains some degree of plasticity. This correlates well with clinical experience in which the first 3–6 months, patients are monitored frequently and bleb manipulations are frequently carried out. There is significant worsening of both BCVA and MD performance beyond 3-year follow-up in the TE group which may be due to a combination of accelerated cataract formation and attrition bias.
Sample size was not evenly distributed across three surgical groups. Some variability was observed in baseline IOP in groups. Patients undergoing VC with or without concurrent cataract extraction and intraocular lens implant were grouped together due to the number of cases and groups. The possible chemical cyclodestructive effect of MMC may account for some IOP reduction in the VC subgroup. IOP measurements were not standardized with repeat measurements at each visit. As most patients were operated on one eye only, it is difficult to completely exclude systemic effect from topical agent into the nonoperated eye. In addition, postoperative outcomes may be influenced by angle morphology and ethnic features such as increased risks of scarring and fibrosis. Postoperative outcome may be further categorized based on IOP into <21 mmHg, <18 mmHg, and <16 mmHg if applied to a more substantial cohort. Albeit, glaucoma being a common ophthalmic diagnosis, the retrospective design subjects this study to differential losses to follow-up. Further research is required in the form of a multicenter, randomized clinical trial for broader population interferences.
Conclusion
Controlling IOP in the management of patients with glaucoma has been the principal element of glaucoma treatment throughout time. Results from this study demonstrate superior average IOP effects over follow-up time in association with optical outcome between primary penetrating and NPS procedures. TE carries high immediate postoperative complication rates that necessitate more frequent follow-up and more additional surgical intervention.
Disclosure
The authors report no conflicts of interest in this work.
References
Henson DB, Thampy R. Preventing blindness from glaucoma. BMJ. 2005;331(7509):120–121. | ||
Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004;82(11):887–888. | ||
Quigley HA. Glaucoma. Lancet. 2007;377(9774):1367–1377. | ||
Royal College of Ophthalmologists. Cataract Surgery Guidelines. London, UK: Royal College of Ophthalmologists; 2010. | ||
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. | ||
Burr JM, Mowatt G, Hernández R, et al. The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation. Health Technol Assess. 2007;11(41):iii–iv, ix–x, 1–190. | ||
Caprioli J, Coleman AL. Intraocular pressure fluctuation a risk factor for visual field progression at low intraocular pressures in the Advanced Glaucoma Intervention Study. Ophthalmology. 2008;115(7):1123–1129. | ||
Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714–720. | ||
European Glaucoma Society. Terminology and Guidelines for Glaucoma. 4th ed; 2014. Available from: http://www.icoph.org/dynamic/attachments/resources/egs_guidelines_4_english.pdf. Accessed April 24, 2018. | ||
Mantravadi AV, Myers JS. Reconsidering trabeculectomy’s strengths and weaknesses. Clin Exp Ophthalmol. 2010;38(9):827–828. | ||
Casson RJ, Salmon JF. Combined surgery in the treatment of patients with cataract and primary open-angle glaucoma. J Cataract Refract Surg. 2001;27(11):1854–1863. | ||
AGIS Investigators. The Advanced Glaucoma Intervention Study: risk of cataract formation after trabeculectomy. Arch Ophthalmol. 2001;119(12):1771–1779. | ||
Husain R, Liang S, Foster PJ, et al. Cataract surgery after trabeculectomy: the effect on trabeculectomy function. Arch Ophthalmol. 2012;130(2):165–170. | ||
Dietlein TS, Widder RA, Jordan JF, Jonescu-Cuypers C, Rosentreter A. Kombinierte katarakt-glaukom-chirurgie [Combined cataract and glaucoma surgery. Current options]. Ophthalmologe. 2013;110(4):310–315. German. | ||
Eldaly MA, Bunce C, Elsheikha OZ, Wormald R. Non-penetrating filtration surgery versus trabeculectomy for open-angle glaucoma. Cochrane Database Syst Rev. 2014;2:CD007059. | ||
Rulli E, Biagioli E, Riva I, et al. Efficacy and safety of trabeculectomy vs nonpenetrating surgical procedures: a systematic review and meta-analysis. JAMA Ophthalmol. 2013;131(12):1573–1582. | ||
Broadway DC, Grierson I, Hitchings RA. Local effects of previous conjunctival incisional surgery and the subsequent outcome of filtration surgery. Am J Ophthalmol. 1998;125(6):805–818. | ||
Lochhead J, Casson RJ, Salmon JF. Long term effect on intraocular pressure of phacotrabeculectomy compared to trabeculectomy. Br J Ophthalmol. 2003;87(7):850–852. | ||
Chang L, Thiagarajan M, Moseley M, et al. Intraocular pressure outcome in primary 5FU phacotrabeculectomies compared with 5FU trabeculectomies. J Glaucoma. 2006;15(6):475–481. | ||
Siriwardena D, Kotecha A, Minassian D, Dart JK, Khaw PT. Anterior chamber flare after trabeculectomy and after phacoemulsification. Br J Ophthalmol. 2000;84(9):1056–1057. | ||
Cheng JW, Cheng SW, Cai JP, Li Y, Wei RL. Systematic overview of the efficacy of nonpenetrating glaucoma surgery in the treatment of open angle glaucoma. Med Sci Monit. 2011;17(7):RA155–RA163. | ||
Husain R, Aung T, Gazzard G, et al. Effect of trabeculectomy on lens opacities in an East Asian population. Arch Ophthalmol. 2006;124(6):787–792. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




