Back to Journals » Clinical Interventions in Aging » Volume 18
Postoperative C-Reactive Protein Predicts Postoperative Delirium in Colorectal Cancer Following Surgery
Received 22 August 2022
Accepted for publication 30 March 2023
Published 4 April 2023 Volume 2023:18 Pages 559—570
DOI https://doi.org/10.2147/CIA.S387117
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Yan Sun, Hui-Ping Peng, Ting-Ting Wu
Department of Anesthesiology, First Affiliated Hospital of Soochow University, Suzhou, Jiangsu, People’s Republic of China
Correspondence: Ting-Ting Wu; Hui-Ping Peng, Email [email protected]; [email protected]
Background: Postoperative delirium (POD) is a common complication in operative patients. Neuroinflammation has been reported to be a potential mechanism associated with the development of POD. Identifying available inflammatory markers such as C-reactive protein (CRP) would aid clinicians in early detection of POD. Previous studies have demonstrated that CRP may be a promising predictive marker for POD. Thus, this study aimed to explore the association between CRP and POD among those elderly colorectal cancer (CRC) patients.
Methods: 643 patients with CRC were included in this study. CRP levels were measured before operation and on postoperative day 1. The univariate and multivariate regression analyses were used to identify risk factors for POD.
Results: Of 643 patients with CRC, 112 cases (17.4%) had POD. CRC patients with POD showed older age, higher CRP level on postoperative day 1, and higher percentage of smoking, diabetes mellitus, and chronic obstructive pulmonary disease (COPD) than CRC patients without POD. Preoperative CRP level was not associated with the POD. Univariate and multivariate regression analyses showed that older age (> 70 years), diabetes mellitus, COPD, and higher CRP level on postoperative day 1 (> 48 mg/L) were risk factors for POD in CRC patients.
Conclusion: Postoperative CRP level is an independent indicator for POD among CRC patients, suggesting the predictive role of postoperative CRP levels for POD in elderly CRC patients undergoing surgery.
Keywords: postoperative delirium, C-reactive protein, colorectal cancer
Introduction
Delirium, an acute brain dysfunction, is characterized by inattention and fluctuating levels of consciousness.1 It is primarily triggered by multiple factors, including drug use or withdrawal, acute medical illness, surgery, or trauma.2 Postoperative delirium (POD) is a common complication in operative patients, which affects nearly 15 to 50% of older patients undergoing major surgery.3 A host of studies have demonstrated that age, poor nutritional status, cognitive impairment, alcohol use, acute medical illness, trauma, and surgery were risk factor for delirium.3–6 POD was associated with longer hospital stay time, long-term cognitive impairment, more postoperative complications, and overall prognosis for patients.7–11
Up to date, pharmacological treatments for POD are not effective, suggesting that substantial gaps in the understanding of its pathophysiology existed.12 Studies indicated that immune activation, oxidative stress and inflammation may involve in the pathogenesis of delirium.12,13 Identifying useful biomarkers to screen out high-risk individuals may help to the early diagnosis of POD and understanding its pathophysiology of POD. Inflammation was a well-established trigger of POD.14–17 C-reactive protein (CRP), an acute-phase protein, is used to indicate acute systemic inflammation for clinicians. CRP was shown to be related to the development of mental disorders.18,19 A host of studies showed that elevated CRP level was associated with the risk of dementia.20–23 In addition, increased CRP level could predict delirium in critically ill patients,24 elderly patients,25 and surgical patients.26,27 CRP was reported to be associated with the risk of POD.28–30 Several studies explored the association between CRP level and the risk of POD, but with contradictory results. For patients receiving orthopedic surgery, three studies found that postoperative CRP could predict POD,28,30,31 while two studies indicated that preoperative CRP could not.32,33 For non-orthopedic surgeries, CRP could predict POD in patients receiving esophagectomy,34 vascular surgery,35 laparoscopic surgery for colon carcinoma.36 No association was observed between CRP and the risk of POD among oncological patients37 or patients after cardiac surgery.38 However, no studies investigated the relationship between preoperative and postoperative CRP levels and the risk of POD among patients with colorectal cancer (CRC) after surgery in Suzhou city. In this study, we aimed to explore the association of CRP levels with the risk of POD in CRC patients following surgery.
Patients and Methods
Participants
643 patients with CRC were included in this study from our hospital from July 2021 to July 2022 (Supplementary Figure 1). All included participants were elderly patients with CRC receiving surgery. The baseline characteristics and clinical data were collected. General characteristics of the participants included age, sex, drinking, smoking, hypertension, diabetes mellitus, chronic obstructive pulmonary disease (COPD), types of CRC, body mass index (BMI), education, intestinal stoma, Mini-mental State Examination (MMSE) score, and anemia. Operation-related characteristics including surgical methods, blood loss, ASA score, operation time, anesthesia time, and narcotic drugs were recorded. The CRP levels were measured before operation (admission to our hospital within 24h) and on postoperative day 1. All individuals provided the signed informed consent. This study was approved by the Ethics Committee of First Affiliated Hospital of Soochow University. This study conformed to the Helsinki declaration.
Inclusion and Exclusion Criteria
The inclusion criteria for CRC should include: (1) aged ≥ 60 years; (2) CRC patients received surgery; (3) ASA score ranged from I to III. Exclusion criteria were as follows: (1) patients without complete data; (2) patients with preexisting cognitive impairment or a history of delirium or dementia before surgery; (3) patients took antipsychotic drugs before surgery which may induce delirium; (4) patients had history of stoke or Alzheimer’s disease; (5) patients had infection before operation or after operation; (5) patients had autoimmune diseases or myocardial infarction or other diseases could result in the increase of CRP level.
Diagnosis of POD
The diagnosis of POD was according to the Confusion Assessment Method (CAM).39 Delirium had the following features: (a) fluctuating course or acute change of mental status; (b) inattention; (c) confused thinking; (d) change in status of consciousness. The diagnosis of POD required the presence of feature (a) and (b), and either (c) or (d). POD in CRC patients was evaluated from postoperative day 1 to 7. POD was evaluated at the same time everyday once a day.
Statistical Analysis
Categorical variables were presented as number (percentage) and analyzed by Fisher exact test or Chi-square test. Continuous variables were shown as means (± standard deviations) or median (with interquartile range) and analyzed by the Student’s t-test or Mann–Whitney U-test. Receiver operating characteristic (ROC) curve was utilized to identify the optimal CRP level for POD. The risk factors for POD were identified using univariate and multivariate logistic regression analyses. Odds ratio (OR) and 95% confidence interval (CI) were calculated. P < 0.05 was considered significant. SPSS (version 21.0, Chicago, IL, USA), and GraphPad Prism (version 8.0, La Jolla, CA, USA) software, MedCalc 20, and R software (version 4.1.3) were used to perform statistical analyses.
Results
Characteristics of the Participants
General characteristics and operation-related characteristics are shown in Table 1. A total of 643 patients with CRC were included; among them, 112 cases (17.4%) had POD. The association between POD and participants characteristics was investigated in this study. We found that CRC patients with POD showed older age, higher CRP level on postoperative day 1, and higher percentage of smoking, diabetes mellitus, and COPD than CRC patients without POD (Table 2). However, no significant differences were shown in sex, drinking, hypertension, types of CRC, anemia, surgical methods, blood loss, ASA score, education, BMI, MMSE score, operation time, anesthesia time, narcotic drugs, and CRP level before operation between POD and non-POD group.
 |
Table 1 The Demographic Characteristics of All CRC Patients |
 |
Table 2 The Demographic Characteristics of CRC Patients in Patients with or Without Delirium |
Diagnostic Value of CRP for POD
The diagnostic value of CRP levels for POD was investigated. ROC curve analysis presented high accuracy for CRP level on postoperative day 1 to predict POD with AUC of 0.755 (Figure 1), and the sensitivity and specificity were 79.46 and 60.83, respectively. However, the AUC of preoperative CRP level was 0.545 (Figure 2). To sum up, the diagnostic ability of CRP level on postoperative day 1 for POD was good.
 |
Figure 1 ROC curve of preoperative CRP with postoperative delirium. |
 |
Figure 2 ROC curve of CRP on postoperative day 1 with postoperative delirium. |
Risk Factors for POD
Univariate and multivariate analyses were used to identify risk factors for POD among CRC patients. The univariate analysis showed that older age (> 70 years), smoking, diabetes mellitus, COPD, and higher CRP level on postoperative day 1 (> 48 mg/L) were associated with POD (Table 3). The multivariate analysis indicated that older age (> 70 years), diabetes mellitus, COPD, and higher CRP level on postoperative day 1 (> 48 mg/L) were risk factors for POD (Figure 3, and Table 4). In addition, we found that older age (> 70 years), smoking, diabetes mellitus, COPD, and higher CRP level on postoperative day 1 (> 48 mg/L) were risk factors for POD among CRC patients following laparoscopic surgery (Supplementary Tables 1 and 2).
 |
Table 3 Univariate Logistic Regression Analyses to Identify the Risk Factors for Postoperative Delirium |
 |
Table 4 Multivariate Logistic Regression Analyses to Identify the Risk Factors for Postoperative Delirium |
 |
Figure 3 The multivariate logistic regression analyses of the factors of postoperative delirium. |
Last, a nomogram model was built to predict POD according to the results of multivariate logistic regression analysis (Figure 4). This nomogram showed a good predictive ability for POD, which was shown by the C-index value of 0.762 (95% CI= 0.710–0.815). In addition, the calibration curve suggested that this nomogram model showed a good consistency between the predicted probability and actual results (Figure 5).
 |
Figure 4 A diagnostic nomogram for the prediction of postoperative delirium. |
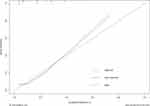 |
Figure 5 Calibration curve of the diagnostic nomogram for the prediction of postoperative delirium. |
Discussion
Herein, this study found that serum CRP level on postoperative day 1 was associated with the risk of POD in CRC patients following surgery, suggesting that postoperative CRP was an independent indicator for POD for CRC patients.
POD is an important issue for patients receiving surgery, especially for the elderly patients.40 POD could increase the hospital stay time, and was related with survival of patients.9 Identifying helpful biomarkers for early diagnosis of POD in high-risk patients is necessary for clinicians. Recently, CRP has been regarded as a good predictor for POD in many studies. Lee et al found that CRP levels on postoperative day 1 and 3 were significantly higher in the delirium group than in the non-POD group in elderly patients after hip surgery.28 Two studies showed that postoperative CRP level predicted POD among patients receiving cervical or lumbar surgery31 and older patients after hip surgery.30 Neerland et al indicated that preoperative cerebrospinal fluid level of CRP was associated with delirium.26 However, Lemstra et al32 and Pan et al33 showed that preoperative CRP level was not an independent predictor for POD among orthopedic patients after surgery.
Except for orthopedic surgery, previous studies investigated the association between POD and preoperative and postoperative CRP levels in other major elective surgery. Two studies found a significant association between preoperative and postoperative CRP levels and the risk of POD,27,41 while Hasegawa et al revealed that preoperative and postoperative CRP levels were not associated with the risk of POD after surgery for oral cancer.42 In addition, preoperative CRP level was a risk factor for POD;43,44 however, Çinar et al showed that it was not associated with the risk of POD.45 In addition, postoperative CRP level was an independent risk factor for POD following vascular surgery35 or esophagectomy.34
In line with most of abovementioned studies, no association between preoperative CRP level and POD in patients with CRC following surgery was observed in this study. However, we found that serum CRP level on postoperative day 1 was associated with the risk of POD in these CRC patients. In contrast to our study, Xiang et al showed that preoperative CRP was an independent predicator for POD in patients with colon carcinoma undergoing laparoscopic surgery.36 Obviously, the study by Xiang et al and our study yielded inconsistent results. We thought the following factors may explain it. One, different sample sizes could affect the final results. Our study and the study by Xiang et al36 included 643 and 160, respectively. Two, the studied populations differed. Xiang et al36 did not include the patients with rectal cancer. Three, different definitions of POD and/or clinical heterogeneity may also be potential reasons. Collectively, this study showed that postoperative CRP level was a good predictor for POD in CRC patients, which was in consistent with the results by previous meta-analyses.15,17
Age was a well-established risk factor for delirium, and was an independent predictor for delirium.46–49 As expected, we found that older age (> 70 years) was a risk factor for POD in patients with CRC by multivariate analysis, which was not shown in the study by Xiang et al.36 They showed that the age was a risk factor for POD in univariate analysis, but not in multivariate analysis,36, which might be due to limited sample size or clinical heterogeneity. Additionally, we observed that diabetes mellitus, and COPD were also risk factors for POD in this study. According to the results of multivariate logistic regression analysis, a nomogram model was generated to predict POD for CRC patients. This nomogram model showed a good predictive ability for POD with a C-index value of 0.762. It is of note that the AUC of CRP level on postoperative day 1 to predict POD was 0.755. It seems that the nomogram model with multi-factors did not significantly increase predictive ability than that of the CRP level on postoperative day 1 (0.762 vs 0.755). On one hand, it indicated that the ability of CRP level on postoperative day 1 to predict POD was good. On the other hand, it may suggest the nomogram model may not include important factors, which may remarkedly increase the predictive ability of this nomogram model. Therefore, a nomogram model with more factors is needed to verify it in the future. Furthermore, the calibration curve found that this nomogram model showed a good consistency between the predicted results and actual observations.
Several limitations were summarized in this study. First, this study was a single-center study with moderate sample size. Second, the younger CRC patients (age< 60 years) should be investigated. Third, some potential confounding factors might exert effects on the final results. Fourth, the CRP levels on postoperative day 2 or longer were measured incompletely, which prevented further analysis. Fifth, there were only a few open cases and the majority were laparoscopic. Therefore, the sample size of open cases was limited. Sixth, controlling for anesthetized medications on the BEERs criteria was not performed in this study. In the future, it is necessary to utilize the BEERs criteria. Last, the underlying mechanisms why CRP could predict POD should be explored in future.
Conclusion
In conclusion, this study shows that postoperative CRP is associated with the risk of POD in CRC patients. Postoperative CRP is an independent indicator for POD for CRC patients.
Funding
This study was not funded.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wilcox ME, Girard TD, Hough CL. Delirium and long term cognition in critically ill patients. BMJ. 2021;373:n1007. doi:10.1136/bmj.n1007
2. Mattison MLP. Delirium. Ann Intern Med. 2020;173(7):ITC49–ITC64. doi:10.7326/AITC202010060
3. Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377(15):1456–1466. doi:10.1056/NEJMcp1605501
4. Gosselt AN, Slooter AJ, Boere PR, Zaal IJ. Risk factors for delirium after on-pump cardiac surgery: a systematic review. Crit Care. 2015;19:346. doi:10.1186/s13054-015-1060-0
5. Thom RP, Levy-Carrick NC, Bui M, Silbersweig D. Delirium. Am J Psychiatry. 2019;176(10):785–793. doi:10.1176/appi.ajp.2018.18070893
6. Zaal IJ, Devlin JW, Peelen LM, Slooter AJ. A systematic review of risk factors for delirium in the ICU. Crit Care Med. 2015;43(1):40–47. doi:10.1097/CCM.0000000000000625
7. Van der Wulp K, van Wely MH, Schoon Y, et al. Geriatric assessment in the prediction of delirium and long-term survival after transcatheter aortic valve implantation. J Thorac Cardiovasc Surg. 2021;161(6):2095–2102 e2093. doi:10.1016/j.jtcvs.2020.02.076
8. Huang H, Li H, Zhang X, et al. Association of postoperative delirium with cognitive outcomes: a meta-analysis. J Clin Anesth. 2021;75:110496. doi:10.1016/j.jclinane.2021.110496
9. Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125(4):492–504. doi:10.1016/j.bja.2020.06.063
10. Huang H, Han J, Li Y, et al. Early serum metabolism profile of post-operative delirium in elderly patients following cardiac surgery with cardiopulmonary bypass. Front Aging Neurosci. 2022;14:857902. doi:10.3389/fnagi.2022.857902
11. Dubiel C, Hiebert BM, Stammers AN, et al. Delirium definition influences prediction of functional survival in patients one-year postcardiac surgery. J Thorac Cardiovasc Surg. 2022;163(2):725–734. doi:10.1016/j.jtcvs.2020.07.028
12. Wilson JE, Mart MF, Cunningham C, et al. Delirium. Nat Rev Dis Primers. 2020;6(1):90. doi:10.1038/s41572-020-00223-4
13. Mashour GA, Woodrum DT, Avidan MS. Neurological complications of surgery and anaesthesia. Br J Anaesth. 2015;114(2):194–203. doi:10.1093/bja/aeu296
14. Taylor J, Parker M, Casey CP, et al. Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: a prospective cohort study. Br J Anaesth. 2022;129(2):219–230. doi:10.1016/j.bja.2022.01.005
15. Wang S, Greene R, Song Y, et al. Postoperative delirium and its relationship with biomarkers for dementia: a meta-analysis. Int Psychogeriatr. 2022:1–14. doi:10.1017/S104161022100274X
16. Zhang W, Wang T, Wang G, Yang M, Zhou Y, Yuan Y. Effects of dexmedetomidine on postoperative delirium and expression of IL-1beta, IL-6, and TNF-alpha in elderly patients after hip fracture operation. Front Pharmacol. 2020;11:678. doi:10.3389/fphar.2020.00678
17. Liu X, Yu Y, Zhu S. Inflammatory markers in postoperative delirium (POD) and cognitive dysfunction (POCD): a meta-analysis of observational studies. PLoS One. 2018;13(4):e0195659. doi:10.1371/journal.pone.0195659
18. Chen S, Chen G, Li Y, et al. Predicting the diagnosis of various mental disorders in a mixed cohort using blood-based multi-protein model: a machine learning approach. Eur Arch Psychiatry Clin Neurosci. 2022. doi:10.1007/s00406-022-01540-3
19. Werner MCF, Wirgenes KV, Shadrin A, et al. Immune marker levels in severe mental disorders: associations with polygenic risk scores of related mental phenotypes and psoriasis. Transl Psychiatry. 2022;12(1):38. doi:10.1038/s41398-022-01811-6
20. Cooper J, Pastorello Y, Slevin M. A meta-analysis investigating the relationship between inflammation in autoimmune disease, elevated CRP, and the risk of dementia. Front Immunol. 2023;14:1087571. doi:10.3389/fimmu.2023.1087571
21. Feng L, Wang Y, Zeng D, Wang M, Duan X. Predictors of cognitive decline in older individuals without dementia: an updated meta-analysis. Ann Clin Transl Neurol. 2023. doi:10.1002/acn3.51740
22. Hsu PF, Pan WH, Yip BS, Chen RC, Cheng HM, Chuang S-Y. C-reactive protein predicts incidence of dementia in an elderly Asian community cohort. J Am Med Dir Assoc. 2017;18(3):277e277–277e211. doi:10.1016/j.jamda.2016.12.006
23. Long S, Chen Y, Meng Y, et al. Peripheral high levels of CRP predict progression from normal cognition to dementia: a systematic review and meta-analysis. J Clin Neurosci. 2023;107:54–63. doi:10.1016/j.jocn.2022.11.016
24. Zhang Z, Pan L, Deng H, Ni H, Xu X. Prediction of delirium in critically ill patients with elevated C-reactive protein. J Crit Care. 2014;29(1):88–92. doi:10.1016/j.jcrc.2013.09.002
25. Ritchie CW, Newman TH, Leurent B, Sampson EL. The association between C-reactive protein and delirium in 710 acute elderly hospital admissions. Int Psychogeriatr. 2014;26(5):717–724. doi:10.1017/S1041610213002433
26. Neerland BE, Hall RJ, Seljeflot I, et al. Associations between delirium and preoperative cerebrospinal fluid C-reactive protein, interleukin-6, and interleukin-6 receptor in individuals with acute hip fracture. J Am Geriatr Soc. 2016;64(7):1456–1463. doi:10.1111/jgs.14238
27. Vasunilashorn SM, Dillon ST, Inouye SK, et al. High C-reactive protein predicts delirium incidence, duration, and feature severity after major noncardiac surgery. J Am Geriatr Soc. 2017;65(8):e109–e116. doi:10.1111/jgs.14913
28. Lee HJ, Hwang DS, Wang SK, Chee IS, Baeg S, Kim JL. Early assessment of delirium in elderly patients after hip surgery. Psychiatry Investig. 2011;8(4):340–347. doi:10.4306/pi.2011.8.4.340
29. Ayob F, Lam E, Ho G, Chung F, El-Beheiry H, Wong J. Pre-operative biomarkers and imaging tests as predictors of post-operative delirium in non-cardiac surgical patients: a systematic review. BMC Anesthesiol. 2019;19(1):25. doi:10.1186/s12871-019-0693-y
30. Slor CJ, Witlox J, Adamis D, et al. The trajectory of C-reactive protein serum levels in older Hip fracture patients with postoperative delirium. Int J Geriatr Psychiatry. 2019;34(10):1438–1446. doi:10.1002/gps.5139
31. Ren Q, Wen YZ, Wang J, et al. Elevated level of serum C-reactive protein predicts postoperative delirium among patients receiving cervical or lumbar surgery. Biomed Res Int. 2020;2020:5480148. doi:10.1155/2020/5480148
32. Lemstra AW, Kalisvaart KJ, Vreeswijk R, van Gool WA, Eikelenboom P. Pre-operative inflammatory markers and the risk of postoperative delirium in elderly patients. Int J Geriatr Psychiatry. 2008;23(9):943–948. doi:10.1002/gps.2015
33. Pan Z, Huang K, Huang W, et al. The risk factors associated with delirium after lumbar spine surgery in elderly patients. Quant Imaging Med Surg. 2019;9(4):700–710. doi:10.21037/qims.2019.04.09
34. Khan SH, Lindroth H, Jawed Y, et al. Serum biomarkers in postoperative delirium after esophagectomy. Ann Thorac Surg. 2022;113(3):1000–1007. doi:10.1016/j.athoracsur.2021.03.035
35. Pol RA, Van Leeuwen BL, Izaks GJ, et al. C-reactive protein predicts postoperative delirium following vascular surgery. Ann Vasc Surg. 2014;28(8):1923–1930. doi:10.1016/j.avsg.2014.07.004
36. Xiang D, Xing H, Tai H, Xie G. Preoperative C-reactive protein as a risk factor for postoperative delirium in elderly patients undergoing laparoscopic surgery for colon carcinoma. Biomed Res Int. 2017;2017:5635640. doi:10.1155/2017/5635640
37. Brattinga B, Plas M, Spikman JM, et al. The association between the inflammatory response following surgery and post-operative delirium in older oncological patients: a prospective cohort study. Age Ageing. 2022;51(2). doi:10.1093/ageing/afab237
38. Kotfis K, Slozowska J, Safranow K, Szylinska A, Listewnik M. The practical use of white cell inflammatory biomarkers in prediction of postoperative delirium after cardiac surgery. Brain Sci. 2019;9(11):308. doi:10.3390/brainsci9110308
39. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–948. doi:10.7326/0003-4819-113-12-941
40. Liu B, Huang D, Guo Y, et al. Recent advances and perspectives of postoperative neurological disorders in the elderly surgical patients. CNS Neurosci Ther. 2022;28(4):470–483. doi:10.1111/cns.13763
41. Dillon ST, Vasunilashorn SM, Ngo L, et al. Higher C-reactive protein levels predict postoperative delirium in older patients undergoing major elective surgery: a longitudinal nested case-control study. Biol Psychiatry. 2017;81(2):145–153. doi:10.1016/j.biopsych.2016.03.2098
42. Hasegawa T, Saito I, Takeda D, et al. Risk factors associated with postoperative delirium after surgery for oral cancer. J Craniomaxillofac Surg. 2015;43(7):1094–1098. doi:10.1016/j.jcms.2015.06.011
43. Knaak C, Vorderwulbecke G, Spies C, et al. C-reactive protein for risk prediction of post-operative delirium and post-operative neurocognitive disorder. Acta Anaesthesiol Scand. 2019;63(10):1282–1289. doi:10.1111/aas.13441
44. Hindiskere S, Kim HS, Han I. Postoperative delirium in patients undergoing surgery for bone metastases. Medicine. 2020;99(20):e20159. doi:10.1097/MD.0000000000020159
45. Cinar MA, Balikci A, Sertoglu E, Mehmet AK, Serdar MA, Ozmenler KN. Role of CRP, TNF-a, and IGF-1 in delirium pathophysiology. Noro Psikiyatr Ars. 2014;51(4):376–382. doi:10.5152/npa.2014.6999
46. Ulsa MC, Xi Z, Li P, et al. Association of poor sleep burden in middle age and older adults with risk for delirium during hospitalization. J Gerontol a Biol Sci Med Sci. 2022;77(3):507–516. doi:10.1093/gerona/glab272
47. Connell J, Kim A, Brummel NE, et al. Advanced age is associated with catatonia in critical illness: results from the delirium and catatonia prospective cohort investigation. Front Psychiatry. 2021;12:673166. doi:10.3389/fpsyt.2021.673166
48. LaHue SC, Escueta DP, Guterman EL, et al. COVID-19 severity and age increase the odds of delirium in hospitalized adults with confirmed SARS-CoV-2 infection: a cohort study. BMC Psychiatry. 2022;22(1):151. doi:10.1186/s12888-022-03809-2
49. Pinho C, Cruz S, Santos A, Abelha FJ. Postoperative delirium: age and low functional reserve as independent risk factors. J Clin Anesth. 2016;33:507–513. doi:10.1016/j.jclinane.2015.09.002
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
