Back to Journals » Patient Preference and Adherence » Volume 14
Post-Arthroscopic Rotator Cuff Repair Rehabilitation Booklet: A Patient-Based Evaluation
Authors Zhang C, Li Q, Li F, Zhang Y, Tang Y, Hou J , Yang R
Received 20 May 2020
Accepted for publication 6 August 2020
Published 24 August 2020 Volume 2020:14 Pages 1493—1500
DOI https://doi.org/10.2147/PPA.S263645
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Congda Zhang, Qingyue Li, Fangqi Li, Yuanhao Zhang, Yiyong Tang, Jingyi Hou, Rui Yang
Department of Orthopedics, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, People’s Republic of China
Correspondence: Rui Yang; Jingyi Hou Tel +86 13694200667
; +86 18102769380
Fax +86 81332199
Email [email protected]; [email protected]
Background: Lack of physical therapists has led to increment of self-managed rehabilitations in post-arthroscopic rotator cuff repair (ARCR) in the forms of booklets or leaflets.
Purpose: The aim of study is to investigate 1) the acceptance of post-ARCR patients towards an education booklet, and 2) whether it could be a timesaving and laborsaving tool to physical therapists.
Methods: An education booklet was established through a systematic review. Patients who underwent ARCR in our hospital were included and randomly assigned to the intervention or control group (27 women, 21 men, mean age= 57.06 years old). Patients in the intervention group received educational booklets, and an evaluation was also obtained after they finished reading. Patients’ understanding of the booklet was determined by asking patients to re-enact training presented in the booklet. Then, a therapist blinded to allocations would personally demonstrate training to patients until patients fully understood the protocol. For the control group, the same therapist coached patients until the whole protocol was clearly understood. The coaching time for patients in both groups was recorded.
Results: Out of 48 patients, 24 (50%) were randomly assigned to the intervention group, and 21 (87.50%) completed their questionnaire. Out of these 21 patients, 20 (95.24%) rated the booklet as “excellent and easy to read”, and 17 (80.95%) felt that the booklet was helpful. The re-enaction accuracy was for strengthening training and specific training (71.43% and 61.90%, respectively). As compared to the control group, the time of coaching for the patients to fully master the protocol in the intervention group was significantly less (P< 0.01).
Conclusion: Patients highly applauded this booklet, and they cherished the information and support it contained. Nevertheless, the re-enaction accuracy was not high, suggesting that the high level of acceptance does not guarantee full understanding of information sent to patients.
Keywords: rotator cuff injuries, arthroscopy, rehabilitation, pamphlets, evaluation studies
Introduction
Rotator cuff tears are one of the main causes of shoulder pain and dysfunction, accounting for about 20% of all shoulder injuries.1 Rotator cuff tears are associated with increasing age, with 25.6% of individuals in their 60s having a tear, which increased up to 50% of individuals in their 80s.2 Arthroscopic rotator cuff repair (ARCR) is one of the most commonly performed treatments for rotator cuff tears.3 It is imperative that patients not only have extremely skilled surgical care but a knowledgeable and experienced physical therapist to help guide their post-operative progression.4 Physical therapy is an important factor in the clinical success of rotator cuff repair.5 A good rehabilitation program is required to increase the likelihood of successful outcome after surgery, to ensure that the patient returns to functional activities, and to improve the patient’s quality-of-life after surgery. However, in order to allow tendon–bone healing, many reports advised against passive shoulder movements for about 1–2 weeks, and active shoulder movements for up to about 6–8 weeks,6–8 which would cause inconvenience to patients. Apart from this, patients need to go back and forth to the clinic frequently to do early rehabilitation training, which is troublesome and leads to a decline in patience compliance. Patient’s poor compliance to rehabilitation postoperatively is a significant independent prognostic factor that determines cuff re-tearing after surgery.9
Especially in developing country, the demand of rehabilitative services for the post-operation patients is increasing by the year, yet rehabilitation organization construction and resource allocation are seriously lacking, leading to low quantity and quality of rehabilitation physicians. The number of therapists in developing countries is significantly lower compared to rehabilitation personnel in developed country. For example, in the US, there are over 50 therapists per 100,000 population; which is about 50-times more than the number in a developing country like China.10 Therefore, a timesaving and laborsaving tool is necessary to account for the lack of therapists.
The American Society of Shoulder and Elbow Therapists (ASSET) offered a consensus rehabilitation guideline following arthroscopic rotator cuff repair.11 The German Society of Shoulder and Elbow Surgery (GSSES) shoulder experts also provided a protocol of rehabilitation after rotator cuff repair by referring to existing scientific literature.12 However, many protocols including the above stated ones did not recommend treatment to patients, but were aimed to provide surgeons and therapists with the support of clinical information. Therefore, these protocols could result in confusion among patients. Recently with the increasing use of social media and technology, there is a trend towards self-management through self-directed education, which facilitates patients taking an active role in identifying their problems, actively seeking professional help, and the experts would provide techniques and skills to aid them in making decisions and take appropriate actions.13 Common self-managed formats are educational materials such as booklets and leaflets, or educational classes on websites.14 Modern patients are active partners in their own healthcare, for which they need and demand accurate, practical information and advice.15
The main purpose of this study is to investigate 1) the acceptance of post-ARCR patients towards an education booklet and 2) whether it could be a timesaving and laborsaving tool to physical therapists. The hypothesis was that this booklet could be proved to be extremely helpful for patients who were uncertain of what they should or should not do after surgery; which simultaneously could act as a timesaving and laborsaving tool for therapists.
Methods
Trial Design
Aimed to validate the booklet’s acceptability in ARCR patients, this study was actually a pilot study of a prospective randomized controlled trial registered in the Chinese Clinical Trial Registry (ChiCTR2000030150). This trial was approved by the Ethics Committees of Sun Yat-sen Memorial Hospital, Sun Yat-Sen Memorial Hospital ethics approval number (2019- KY-095), and all participants were required to sign an informed consent form and agree to this study. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Inclusion and Exclusion Criteria
Inclusion criteria were as follows: 1) aged between 16 and 64 years, 2) agreed to receive arthroscopic repair of rotator cuff, 3) diagnosed as small to large full-thickness rotator cuff tear (less than 5 cm), with imaging support, and 4) signed the informed consent form. Patients were excluded if 1) they were diagnosed with tuberculosis, shoulder joint infection, and tumor patients, 2) they had previous or upcoming scheduled shoulder surgery before this trial, 3) they had a massive rotator cuff tear (more than 5 cm) or other shoulder joint injury such as SLAP injury or Bankart injury, 4) they had shoulder dyskinesia because of neurological diseases, and 5) those who could not complete the rehabilitation training because of mental retardation or other reasons.
Sample Size
In our pilot study of 20 patients (10 patients in each group), the mean of coaching time in the control groups and the intervention (booklet) group were 45 minutes and 30 minutes, and the standard deviations were 12 minutes and 13 minutes. In a previous study of exercise instruction following arthroscopic full-thickness rotator cuff repair surgery, the mean of the coaching time was approximately 15 minutes in each phase, approaching the coaching time of the control group in our pilot study (three phases in our protocol, in total 45 minutes).16 Therefore, based on the previous studies and our pilot study, we predicted the mean coaching time in the control group as 45 minutes and standard deviation as 12 minutes. In a study of home-based exercises, patients who received an exercise guide booklet with detailed instructions following rotator cuff tear, had a mean time of 30 minutes of coaching, which was close to the coaching time of the booklet group in our prior study.17 Therefore, according to the previous and our pilot study, the mean coaching time and standard deviation in the intervention group were predicted as 30 minutes and 13 minutes. Then the sample sizes were calculated by PASS 15.0 software using Two-sample T-tests to detect a significant difference in coaching time. A sample size of 20 patients in each group was required for a power of 90% at a two-sided alpha of 0.05, which allowed for loss to follow-up of 20%.
Intervention
Patient randomization was determined by a nurse opening a randomly selected envelope immediately after the surgery. Patients who were randomly classified into the intervention group received the paper education (booklet) before surgery. After the patients finished reading the booklet, one researcher would confirm patients’ understanding of the booklet by asking patients to re-enact the training presented in the booklet, and the accuracies would be recorded. After the re-enaction, an instructor (physiotherapist) who was blinded to the allocation would coach the patients in all training until they fully understood the protocol.
In the control group, the same instructor would coach the patients by oral instruction or personal demonstration until they could fully understand the protocol. All surgeons were fully briefed on the study and endorsed and supported the trial interventions. All the surgical procedures were performed by the same surgeon, using the same double-row repair surgical method. Both groups received standard pre- and post-surgical physical therapy based on the same protocol.
Systematic Review
An electronic search of CENTRAL, MEDLINE, PubMed, PEDro, and FMJS was undertaken by two independent researchers. We searched the following key terms: “supraspinatus” OR “infraspinatus” OR “subscapularis” OR “teres minor” OR “rotator cuff” OR “cuff muscles”, “repair” OR “surg” OR “surgery” OR “surgical treatment”, “rehabilitation” OR “rehab” OR “physical therapy” OR “physiotherapy”. Literatures that were published between September 1993 and September 2018 were included and resulted in 471 articles. After a systematic review of the abstracts, 430 articles were eliminated as they were either (i) non-related articles that did not meet the inclusion criteria or (ii) were duplicates from different databases. After reviewing the full text of the remaining 41 articles, 23 articles were eliminated (13 studies were review articles and 10 studies did not contain post-operative rehabilitation data), 18 articles remained and were extracted (full details are given in Appendix S2).
Educational Booklet
After systematic review, 18 articles remained and were extracted to develop the major principle and time frames guiding rehabilitation. Building on the themes and evidence statements from database searches, appropriate patient-centered messages were developed, and a booklet text was written from a patient’s point-of-view. After the development of major principles and time frames guiding rehabilitation, the recommendations were sent to two independent arthroscopic surgeons to review, provide feedback, and develop a consensus (immobilization time frames, when to initiate active ROM, time to restore normal ROM, and so on). Finally, a surgeon with extensive experience performing arthroscopic RCR reviewed the recommendation to provide a surgeon’s perspective. The booklet is intended to foster matched expectations among patients to provide a patient-centered rehabilitation strategy.
Patients randomized to the intervention group would receive a copy of “Rehabilitation following Arthroscopic Rotator Cuff Repair (ARCR)” (Appendix S1) from the therapists before surgery. The particular development process of the booklet is contained in Appendix S2.
Outcome Measures
To investigate patient’s acceptability of the booklet in the intervention group, a questionnaire (Appendix S3) was used to determine the patients’ acceptance of the booklet after their first reading, which rated the booklet with regard to helpfulness, content, length, usability, etc. To investigate the understandability of the booklet, a researcher asked the patients to re-enact the training presented in the booklet after their first reading, and the accuracies of re-enaction were recorded.
To determine the time and labor-saving potential of the booklet, the “coaching time” of the two groups were compared. In the intervention group, after the patients finished reading the booklet and re-enaction, a physiotherapist who was blinded to the allocation would instruct the required training to the patient by oral instruction or personal demonstration until the patient fully understood the rehabilitation protocol, the time of instruction was recorded and defined as the “coaching time”. In the control group, the same physiotherapist also coached the patients with all the required training and the time for patients to fully master the protocol was recorded and defined as the “coaching time” for the control group. In order to reduce bias, one other researcher who was also blinded to the allocation measured all the “coaching time” using the same chronograph.
Statistical Methods
Student’s t-test was used to assess the difference of “coaching time”, age, education in the booklet group, and control group. The Chi-Square test was used to compare discrete variables (gender, tear size) between the two groups. Among the booklet group, difference of acceptance and accuracies between age ≥60 and age <60 were analyzed using the Chi-Square test. Analyses were performed using the SPSS software package (version 21.0, SPSS), and P<0.05 was considered statistically significant.
Results
Sixty patients underwent ARCR between February 2020 and April 2020 in our hospital. Out of 60 patients, 48 met the inclusion criteria and were included in this study and were randomly divided into two groups: (a) the control (n=24) and (b) the intervention groups (n=24). Out of the 24 patients in the intervention group, 14 were female and 10 were male, aged between 44–64 years old. Twenty-four participants were also selected to participate in the control (without “booklet”) group and fourteen (n = 13) of these participants were female, and ten (n = 11) were males, aged between 44–64 years old. As listed in Table 1, no significant differences were observed between the two groups in regards to age, gender, education level, or tear size (P>0.05).
 |
Table 1 Demographic Characteristics of Participants in This Study |
Booklet evaluations (Appendix S3) were sent to 24 (10 men, 14 women) patients in the intervention group and 21 (eight men, 13 women) returned the evaluation (87.50%) (Table 2). Of the responders, 20 patients (95.24%) reported that they found the booklet easy to read, 17 (80.95%) stated that they felt the booklet was helpful, and 19 (90.48%) felt it was the right length, while two felt it was too long. Fourteen (66.67%) said that the contents were interesting, though that number may be depressed because seven of the other patients felt these were just normal. Four of the patients offered practical tips from their own experience and they thought that not everything was covered. Two patients felt they could not train alone and three felt it was not easy to follow. Many patients read the booklet more than once, with 14 referring to it occasionally and six frequently referring to it during their recovery. The majority (19 patients) took at least 10 minutes to read the booklet, among them, eight patients took more than 30 minutes. The booklet was overall welcomed by patients (mean rating=8.33±1.04, 10 as the best). No significant differences were observed between the age ≥60 group and age <60 group in regards to the content (P>0.05).
 |
Table 2 Evaluation of the Booklet |
When subjects were presented with the booklet after the first reading, most subjects understood the important messages from the booklet (Table 3). Out of these 21 patients, 19 (90.48%) fully understood the meaning of immobilization and the training in the active ROM part. However, a few trainings were difficult to understand such as the strengthening (Appendix S1, Phase 2, section 9–12) and specific training (Appendix S1, Phase 3, section 11–13). The re-enaction accuracies of strengthening training and specific training were 71.43% and 61.90%, respectively. No significant differences were observed between the age ≥60 group and age <60 group in regards to the accuracy (P>0.05). As compared to the control group (no prior education with the booklet), the “coaching time” for patients in the intervention group to fully master the protocol of rehabilitation after ARCR was significantly less (P<0.01) (Table 4).
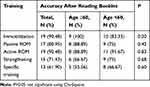 |
Table 3 Patient’s Understanding Ability After Reading the Booklet for the First Time |
 |
Table 4 Time of Coaching for Patient to Fully Master the Protocol (minutes) |
Discussion
In this study, the booklet proved to be extremely helpful for post-ARCR patients who were uncertain of what they should or should not do after surgery; while it simultaneously could act as a timesaving and laborsaving tool for therapists. We established a rehabilitation booklet for patients based on a systematic review and combined with clinical experience in rehabilitation programs following ARCR. The most important finding of our study is that, although patients had a high acceptance of the booklet, the accuracy of patients to follow the booklet’s instruction was lower than expected. Furthermore, the time required to demonstrate the training was greatly reduced after the patients completed the booklet, which indicated that the booklet could be a timesaving and laborsaving tool to physical therapists. However, the ability of patients to follow the booklet’s instruction was lower than expected, suggesting that proper improvement of the booklet education should be done and could be incorporated with oral instruction or personal demonstration, especially for those who were new to rehabilitation.
Shoulder rehabilitation after ARCR presents unique challenges, such as balancing protection of the repair with the desire to initiate early range of motion to prevent long-term stiffness and pain. By concentrating on scientific and academic rigor, the booklet (Appendix S1) was developed based on a systemic review of the current literature combined with our clinical experience. In the articles which were extracted, eight of the studies investigated the effects of early postoperative ROM exercise compared with delayed rehabilitation protocols18–25 and two of them reported that patients in the group who were treated with early ROM exercise had a quicker recovery of ROM than the delayed group.18,21 However, two of the studies reported that there was a slightly higher rotator cuff healing rate in the delayed passive range of motion group compared with the early passive range of motion group.19,24 The remaining literature examining early rehabilitation post-ARCR found no significant differences between groups.20,22,23,25 These findings suggest that early rehabilitation post-ARCR may not be the best rehabilitation protocol. After the development of major principles and time frames guiding rehabilitation, the recommendations were sent to two independent arthroscopic surgeons to review, provide feedback, and develop a consensus. Therefore, the booklet is a gentle rehabilitation protocol with limits in ROM and exercise times after arthroscopic rotator cuff repair which would be better for tendon healing without taking any substantial risks, which balanced protection of the repair and risk of the stiffness.
Due to severe shortage of rehabilitation resources in China,10 maximum utilization of rehabilitation resources is very important. Booklets are a simple, affordable, and well accepted method of providing rehabilitation-related information to patients.26 Although ASSET offers a consensus rehabilitation guideline following arthroscopic RCR, this guideline did not clearly explain the specific rehabilitation exercises that the patient should do.11 In the evaluations of our booklet, it was clear that patients needed precise explanation regarding specific exercises and stretches, favoring a clear regime rather than simple and general open advice.27 The booklet is intended to be handed out to patients by surgeons and therapists as a clinical tool to supplement and reinforce verbal communication between healthcare provider and patients. In our evaluation, the booklet was welcomed by patients as they can obtain specific instruction, easily learning the information and executing the content at their own pace and time. However, as it is with the development of every learning material, developing an acceptable and effective informational material is hard even for the apparently simple medium of booklets or leaflets.26 Our study also showed that the high level of acceptance does not guarantee the full understanding of the message sent to the patients.
In some of the studies,28,29 although hospitalized patients with an educational booklet valued the information and rated it useful, their results showed the information was not fully understood by patients. Similarly, our booklet was highly regarded by most patients, but the accuracies of re-enaction in some training were not high. However, receipt of a booklet or even rating it useful does not necessarily mean that the patient comprehended, or followed what was stated in the booklet. This result could be related to an allegiance effect, which implies that participants’ responses are shaped in the direction of the experimenter’s expectations.30 It shows that a high level of acceptance does not necessarily mean that the patient really fully understands the message being sent to them. Depending on the level of the patient’s personal educational background, understanding a simple instruction might prove to be difficult.31,32 Some feedbacks from patients also suggested that these educational materials could be uploaded on websites or as applications on mobile phones to have more accessibility for the patients, which may also improve the accuracy. Some studies showed that website-based delivery of preoperative education for surgery is feasible and has similar patient satisfaction compared to traditional paper-based methods.31,33 This study was actually a pilot study of a clinic trial aimed to develop a mobile phone telerehabilitation exercise system for ARCR patients and compare it with outpatient and booklet rehabilitation, registered in the Chinese Clinical Trial Registry (ChiCTR2000030150). Through this study, we can determine the acceptability of the booklet and lay the foundation for future study.
However, we do acknowledge the limitations of this study. First, the double-blind design was not appliable in our study. As this is a study focused on comparison of booklet based and personal instruction based rehabilitation, it was difficult to blind the allocation to the patients, which is also the case for most rehabilitation-related studies.27,31 However, the outcome between the two groups involved in this study is the coaching time, which is an objective index and measured by a third researcher blind to the allocation. Thus, the measuring bias could be reasonably reduced. Furthermore, we found that the patients in the intervention group asked similar questions, which means that the booklet has some common defects. To improve the booklet, we can add some explanations to the questions which patients asked most frequently such as the criteria of discharge and back to work. To the trainings which were difficult to understand, such as the strengthening (Appendix S1, Phase 2, section 9–12) and specific training (Appendix S1, Phase 3, section 11–13), we can give more detailed motion instructions and pictures.
Conclusion
Herein, we designed a patient-based rehabilitation booklet that was established after an extensive systematic review in combination with clinical expertise. Patients’ feedback showed that this booklet was welcomed, as the booklet contained valued information and support for their recovery. Considering the negative feedback from patients, it is suggested that a high level of acceptance does not guarantee full understanding of the message sent to the patients. We would revise this booklet and address these issues to present a clearer educational material for patients after RCR, and would also widen the scope of the material to educational videos to be uploaded on social media and applications on mobile phones to reach more patients in the future.
Abbreviations
ARCR, arthroscopic rotator cuff repair; ASSET, The American Society of Shoulder and Elbow Therapists; GSSES, German Society of Shoulder and Elbow Surgery; MDT, multi-disciplinary team; ROM, range of motion; PFF, passive forward flexion; PER, passive external rotation; RCT, randomized controlled trial; PCS, prospective study; CPM, continuous passive motion CPM.
Data Sharing Statement
All the data presented in this paper are freely available upon request from the corresponding authors.
Acknowledgment
We would like to thank all participants for their time and willingness to participate in this study.
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Lo IKY, Burkhart SS. Current concepts in arthroscopic rotator cuff repair. Am J Sports Med. 2003;31(2):308–324. doi:10.1177/03635465030310022701
2. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604. doi:10.1016/j.csm.2012.07.001
3. Shibata Y. Arthroscopic rotator cuff repair. Advan Shoulder Surg. 2016;129–143.
4. Sgroi TA, Cilenti M. Rotator cuff repair: post-operative rehabilitation concepts. Curr Rev Musculoskelet Med. 2018;11(1):86–91. doi:10.1007/s12178-018-9462-7
5. Ross D, Maerz T, Lynch J, Norris S, Baker K, Anderson K. Rehabilitation following arthroscopic rotator cuff repair: a review of current literature. J Am Acad Orthop Surg. 2014;22(1):1–9. doi:10.5435/JAAOS-22-01-1
6. Cohen BB, Romeo AA, Bach B. Rehabilitation of the shoulder after rotator-cuff repair. Oper Tech Orthop. 2002;12(3):218–224. doi:10.1053/otor.2002.36289
7. Hayes K, Ginn KA, Walton JR, Szomor ZL, Murrell GAC. A randomised clinical trial evaluating the efficacy of physiotherapy after rotator cuff repair. Austr J Physiother. 2004;50(2):77–83. doi:10.1016/S0004-9514(14)60099-4
8. Grueninger P, Nikolic N, Schneider J, et al. Arthroscopic repair of traumatic isolated subscapularis tendon lesions (Lafosse Type III or IV): a prospective magnetic resonance imagingecontrolled case series with 1 year of follow-up. Arthroscopy. 2014;1–8.
9. Ahmad S, Haber M, Bokor DJ. The influence of intraoperative factors and postoperative rehabilitation compliance on the integrity of the rotator cuff after arthroscopic repair. J Shoulder Elbow Surg. 2015;24(2):229–235. doi:10.1016/j.jse.2014.06.050
10. Zhang H, Shen Q. The current situation of rehabilitation medical service system in china: problems and challenges. Business Manage Res. 2014;3:2. doi:10.5430/bmr.v3n2p42
11. Thigpen CA, Shaffer MA, Gaunt BW, Leggin BG, Williams GR, Wilcox RB. The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(4):521–535. doi:10.1016/j.jse.2015.12.018
12. Jung C, Tepohl L, Tholen R, et al. Rehabilitation following rotator cuff repair. Obere Extremitat. 2018;13:45–61(13):45–61. doi:10.1007/s11678-018-0448-2
13. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self management of chronic disease in primary care. JAMA. 2002;288:2469.
14. Engers AJ, Jellema P, Wensing M, Dawm VDW, Grol R, van Tulder MW. Individual patient education for low back. Cochrane Database Syst Rev. 2008;1:CD004057.
15. Entwistle VA, Watt IS. Disseminating information about healthcare effectiveness a survey of consumer health information services. Qual Health Care. 1998;7::124–129. doi:10.1136/qshc.7.3.124
16. Roddey TS, Olson SL, Gartsman GM, Hanten WP, Cook KF. A randomized controlled trial comparing 2 instructional approaches to home exercise instruction following arthroscopic full-thickness rotator cuff repair surgery. J Orthopaedic Sports Phys Ther. 2002;32(11):548–559. doi:10.2519/jospt.2002.32.11.548
17. Krischak G, Gebhard F, Reichel H, et al. A prospective randomized controlled trial comparing occupational therapy with home-based exercises in conservative treatment of rotator cuff tears. J Shoulder Elbow Surg. 2013;22(9):1173–1179. doi:10.1016/j.jse.2013.01.008
18. Duzgun I, Baltaci G, Atay OA. Comparison of slow and accelerated rehabilitation protocol after arthroscopic rotator cuff repair: pain and functional activity. Acta Orthop Traumatol Turc. 2011;45(1):23–33. doi:10.3944/AOTT.2011.2386
19. Lee BG, Cho NS, Rhee YG. Effect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: aggressive versus limited early passive exercises. Arthroscopy. 2012;28(1):34–42. doi:10.1016/j.arthro.2011.07.012
20. Duzgun I, Baltaci G, Turgut E, Atay OA. Effects of slow and accelerated rehabilitation protocols on range of motion after arthroscopic rotator cuff repair. Acta Orthop Traumatol Turc. 2014;48(6):642–648. doi:10.3944/AOTT.2014.13.0125
21. Arndt J, Clavert P, Mielcarek P, et al. Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: a prospective randomized study. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S131–138. doi:10.1016/j.otsr.2012.05.003
22. Kim YS, Chung SW, Kim JY, Ok JH, Park I, Oh JH. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am J Sports Med. 2012;40(4):815–821. doi:10.1177/0363546511434287
23. Roo P-JD, Muermans S, Maroy M, Linden P, Daelen L. Passive mobilization after arthroscopic rotator cuff repair is not detrimental in the early postoperative period. Acta orthopaedica Belgica. 2015;81(3):485–492.
24. Cuff DJ, Pupello DR. Prospective randomized study of arthroscopic rotator cuff repair using an early versus delayed postoperative physical therapy protocol. J Shoulder Elbow Surg. 2012;21(11):1450–1455. doi:10.1016/j.jse.2012.01.025
25. Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014;96(1):11–19. doi:10.2106/JBJS.M.00034
26. McGregor AH, Burton AK, Sell P, Waddell G. The development of an evidence-based patient booklet for patients undergoing lumbar discectomy and un-instrumented decompression. Eur Spine J. 2007;16(3):339–346. doi:10.1007/s00586-006-0141-9
27. McGregor AH, Henley A, Morris TP, Dore CJ. Patients’ views on an education booklet following spinal surgery. Eur Spine J. 2012;21(8):1609–1615. doi:10.1007/s00586-012-2242-y
28. Bjornnes AK, Parry M, Lie I, et al. The impact of an educational pain management booklet intervention on postoperative pain control after cardiac surgery. Eur J Cardiovasc Nurs. 2017;16(1):18–27. doi:10.1177/1474515116631680
29. Ergen WF, Pasricha T, Hubbard FJ, et al. Providing hospitalized patients with an educational booklet increases the quality of colonoscopy bowel preparation. Clin Gastroenterol Hepatol. 2016;14(6):858–864. doi:10.1016/j.cgh.2015.11.015
30. T S, GJ. A. Internal and external validity in clinical research. In: Michael C. Roberts and Stephen S. Ilardi. Handbook of Research Methods in Abnormal and Clinical Psychology. Los Angeles, CA: Sage Publications; 2008:23–34.
31. Dayucos A, French LA, Kelemen A, Liang Y, Sik Lanyi C. Creation and evaluation of a preoperative education website for hip and knee replacement patients-a pilot study. Medicina (Kaunas). 2019;55:2.
32. Johnson HM, LaMantia JN, Brown CM, et al. My Hypertension Education and Reaching Target (MyHEART): development and dissemination of a patient-centered website for young adults with hypertension. JMIR Cardio. 2017;1:2. doi:10.2196/cardio.8025
33. Heikkinen K, Leino-Kilpi H, Salanterä S. Ambulatory orthopaedic surgery patient’s knowledge with internet based education. Methods Inf Med. 2012;51:295–300. doi:10.3414/ME11-02-0004
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
