Back to Journals » Nature and Science of Sleep » Volume 12
Positional Sleep Apnea Among Regional and Remote Australian Population and Simulated Positional Treatment Effects
Authors Garg H, Er XY, Howarth T , Heraganahally SS
Received 20 October 2020
Accepted for publication 19 November 2020
Published 4 December 2020 Volume 2020:12 Pages 1123—1135
DOI https://doi.org/10.2147/NSS.S286403
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Himanshu Garg,1 Xin Yi Er,1 Timothy Howarth,2,3 Subash S Heraganahally1,3,4
1Department of Respiratory and Sleep Medicine, Royal Darwin Hospital, Darwin, Northern Territory, Australia; 2College of Health and Human Sciences, Charles Darwin University, Darwin, Northern Territory, Australia; 3Darwin Respiratory and Sleep Health, Darwin Private Hospital, Tiwi, Darwin, Northern Territory, Australia; 4Flinders University – College of Medicine and Public Health, Adelaide, South Australia
Correspondence: Subash S Heraganahally
Department of Respiratory and Sleep Medicine, Royal Darwin Hospital, 105, Rocklands Drive, Tiwi, Darwin, NT, Australia
Tel +61-8-89228888
Fax +61-8-89206309
Email [email protected]
Purpose: To assess the prevalence of positional sleep apnea (POSA) and its predictors in patients diagnosed to have obstructive sleep apnea (OSA) in the regional and remote population of the Northern Territory of Australia over a two-year study period (2018 and 2019).
Patients and Methods: Of the total 1463 adult patients who underwent a diagnostic polysomnography (PSG), 946 patients were eligible to be included in the study, of them, 810 consecutive patients with OSA (Apnea-Hypopnea Index (AHI) ≥ 5) who slept > 4 h and had ≥ 30 min sleep in both supine and lateral positions were assessed. Patients were considered to have POSA if supine AHI to lateral AHI ratio ≥ 2. The likely comparative impact of use of continuous positive airway therapy (CPAP) or positional therapy (PT) on disease severity was evaluated using model simulation.
Results: A total of 495/810 (61%) patients had POSA, the majority were males (68% vs 60%, p=0.013) and non-Indigenous Australians (93% vs 87%, p=0.004). POSA patients were younger (mean difference 2.23 years (95% CI 0.27, 4.19)), less obese (BMI mean difference 3.06 (95% CI 2.11, 4.01)), demonstrated less severe OSA (p < 0.001) and a greater proportion reported alcohol consumption (72% vs 62%, p=0.001) as compared to those with non-POSA. Using the simulation model, if patients with POSA use PT two-thirds (323/495, 65%) would obtain significant improvement of their OSA severity, with one in five (92/495, 19%) displaying complete resolution. Comparing this to simulated CPAP therapy, where the majority (444/495, 90%) will show significant improvement, and one-third (162/495, 33%) will display complete resolution.
Conclusion: POSA needs to be routinely recognised and positional therapy integrated in practice especially in the remote regions and in the developing world when effective methods are in place to monitor positional therapy.
Keywords: adherence: apnea hypopnea index, body mass index, continuous positive airway pressure, obstructive sleep apnea, positional therapy
Introduction
The global prevalence of obstructive sleep apnea (OSA) is estimated to be between 6 and 17% across various populations, particularly affecting those who are ageing or have a higher body mass index (BMI).1,2 OSA is known to interact with and predisposes to cardiovascular diseases leading to reduced quality of life and higher mortality.3–6 A growing body of literature exists to define the determinants and phenotypes of sleep apnea to better develop personalised treatment options for patients diagnosed with OSA.7,8 Body position is known to impact the severity of OSA and supine sleep is observed to be associated with higher apnea-hypopnea index (AHI)9, moreover, body position parameters are recommended to be measured routinely among patients undergoing polysomnography (PSG) testing.10
A distinct clinical type of OSA, “positional sleep apnea” (POSA) is considered when respiratory events occur predominantly in certain body position during sleep.9,11 There are currently multiple clinical definitions of POSA; however, regardless of which definition is used, prevalence of POSA typically exceeds 50% among patients undergoing a PSG and diagnosed to have OSA.12–15 It is also observed that in supine sleep, apneas and arousals are longer, desaturations are deeper, snoring is louder, and occurrence of tachy-bradycardia following an apnoeic episode are more severe compared to lateral sleep position.16
Continuous positive airway pressure (CPAP) therapy is a well-established treatment modality for OSA and has been shown to improve quality of life in these patients.17,18 However, acceptance and long-term adherence to CPAP therapy can be variable.19–22 Previous studies have reported non-adherence rates to CPAP therapy can range between 34 and 83%.23,24 Consequently, a substantial proportion of patients with OSA who are either untreated or non-adherent to CPAP can experience adverse health consequences.25 Moreover, the affordability and accessibility to a CPAP device can be a major issue, especially among the socioeconomically disadvantaged and people living in regional and remote communities.26,27 However, alternate therapeutic interventions may be helpful in addressing this issue.28,29
OSA is highly prevalent among the adult Australian population.30 However, there is sparse published evidence in the literature in relation to POSA in the regional and remote Australian setting. Previous studies from our centre at the Top End Health Service (TEHS) region of the Northern Territory (NT) of Australia have demonstrated a higher proportion of OSA among both Australian Aboriginal and/or Torres Strait Islander (ATSI) (henceforth represented as Indigenous Australians with respect) and non-Indigenous population.31–33 The population profile of the Top End, NT of Australia is unique and diverse, with a population of about 249,220 people and about 30% of whom are of Indigenous Australian descent living in an area stretched over 245,000 km2 (94,595.0 sq miles) in the northern, sub-tropical part of Australia.34 Moreover, 81% of Indigenous Australians and a minor proportion of non-Indigenous people live in remote and regional communities that can be accessed only by seasonal light aircraft. Hence, access to and monitoring of therapeutic interventions such as CPAP therapy possess unprecedented challenges due to the logistics involved. However, positional therapy (PT) may provide a viable alternative option in this population for those diagnosed to have OSA given the high rates of OSA reported in the literature, that may potentially change the treatment paradigm for OSA in this region. Initially however, it is critical to assess the prevalence of POSA in this population for further interventions. Hence, in this study, we evaluated the demographic, clinical and PSG characteristics and the presence of POSA among patients who underwent a diagnostic sleep study (PSG) in our centre. Furthermore, we also made an attempt to explore a model simulated scenario to understand if PT would be beneficial in this population.
Patients and Methods
Setting and Study Participants
This retrospective study was conducted at the Royal Darwin Hospital (RDH) and Darwin Respiratory and Sleep Health (DRSH), Darwin Private Hospital (DPH) in the TEHS region of the NT of Australia. Patients over 18 years of age from the TEHS region who underwent a diagnostic PSG over a 2-year (2018–2019) study period were included in this study. As per usual practice in our centre, patients underwent a diagnostic PSG after an initial clinical consultation with a Respiratory and Sleep Specialist based at the RDH/DPH. The patients were referred to the respiratory and sleep service at RDH and DRSH/DPH by primary health physicians, general practitioners and specialist practitioners for clinically suspected sleep disorders.
Clinical Parameters
As per usual protocol in this centre, clinical and demographic characteristics including self-identified ethnic status, age, sex, height, weight, BMI (underweight (BMI≤18.5), normal weight (BMI>18.5 and BMI≤25), overweight (BMI>25 and BMI≤30), Obese I (BMI>30 and BMI≤35) and Obese II (BMI>35)), neck circumference and medical co-morbid conditions were recorded for all patients undergoing a sleep study. Self-reported Epworth Sleepiness Scale (ESS) score, alcohol history and smoking status were also recorded. Patient’s residence locality was identified by post code and they were classified as either living in urban, outer rural Regional Australia (RA 2, 3) or remote (RA4) and very remote (RA5), in accordance within the TEHS regions.35
Polysomnography (PSG) Data
All PSGs were performed at the Darwin-based sleep service facility, DRSH based at the DPH, an accredited sleep testing facility by the National Association of Testing Authorities, Australia (NATA) and the Australian Sleep Association (ASA). Sleep studies were performed and analysed in accordance with the American Academy of Sleep Medicine recommendations and as described in previous reports from our centre.31,32 Polysomnography data were extracted to include information on the severity of sleep disordered breathing using Apnea-Hypopnea Index (AHI) criteria. Total AHI was categorised into four groups: AHI ≤5 (normal range), AHI = 5–14.9 (mild sleep apnea), AHI = 15–29.9 (moderate sleep apnea), AHI ≥ 30 (severe sleep apnea). PSG parameters for sleep architectures were also assessed. Only level 1 (monitored “in-lab”) and level 2 (unmonitored ambulatory home) studies were included in the analysis. In order to accurately determine prevalence of POSA the following additional study inclusion criteria were applied: total sleep time ≥4 hours, and recorded time in supine and lateral positions ≥30 minutes each.
POSA and Non-POSA Consideration
Utilising a modified Cartwright definition9 POSA was defined as; total AHI ≥5, and supine to lateral AHI ratio of ≥2:1. Non-POSA was defined as presence of OSA which did not meet the preceding criteria.
Treatment Simulation
The likely impacts on disease severity of treatment modalities were simulated in the present study. In order to give meaningful comparisons and account appropriately for real-world scenarios, optimal usage of both PT and CPAP therapy were set to be the same (60%) for the duration of sleep. The impact of PT was simulated assuming that therapy caused patients to sleep in the (non-supine) lateral position 60% of the night; thus, the PT simulated AHI was calculated using the formula:  . The simulation of the CPAP effect was based on the assumption that the frequency of apnea/hypopnea events is constant throughout the night. Furthermore, it was assumed that CPAP with optimal pressure prevents all respiratory events, and no apneas or hypopneas occur during simulated CPAP usage. CPAP adherence was considered optimal for 60% of the total sleep time.36 Therefore, total AHI in this CPAP simulation was calculated using the formula:
. The simulation of the CPAP effect was based on the assumption that the frequency of apnea/hypopnea events is constant throughout the night. Furthermore, it was assumed that CPAP with optimal pressure prevents all respiratory events, and no apneas or hypopneas occur during simulated CPAP usage. CPAP adherence was considered optimal for 60% of the total sleep time.36 Therefore, total AHI in this CPAP simulation was calculated using the formula: 
Statistical Consideration
Continuous parameters were initially analysed for normality via the Shapiro Wilks distribution test, and all were found to have non-parametric distribution (p<0.01) thus reported as medians (interquartile ranges (IQRs)) while categorical variables were reported as numbers (percentages). BMI was reported both as a continuous parameter and as categorical parameters.
Demographic and clinical parameters were compared between POSA and non-POSA (excluding non-OSA participants) using equality of medians test for continuous parameters, and two-tailed proportions z-test for categorical parameters. Univariate and multivariate logistic regression models were developed to define the individual and combined effects of demographic and clinical parameters on presence of POSA reporting odds ratios (ORs) and 95% confidence intervals (95% CIs), parameter p-values, model p-value and Pearson’s pseudo R2. Predictive patterns of the univariate and multivariate models were graphically represented in coefficients plots.
PSG parameters were compared between POSA and non-POSA (excluding non-OSA participants) using equality of medians test and Wilcoxon rank-sum equality of distributions test, reporting p-values for each. Oxygen saturation parameters were further graphically represented utilising kernel density graphs comparing POSA and non-POSA participants.
Treatment simulation was explored for participants with POSA, comparing post-treatment AHI and absolute AHI reduction between PT and CPAP therapy via equality of median tests and Wilcoxon rank-sum equality of distributions test. The proportions of the number of participants who would demonstrate reduction of one severity level (ie, severe (AHI≥30) to moderate (AHI 15–29.9)) and the proportions of those who would demonstrate any reduction in severity level (ie, severe (AHI≥30) to moderate (AHI 15–29.9), severe to mild (AHI 5–14.9) and severe to absent (AHI<5) summed) were tested between PT and CPAP therapy using two-tailed proportions z-test. All analysis was conducted in STATA IC 15.1 (StataCorp Texas).
Ethical Approval
This study was approved by the Human Research Ethics Committee of the NT Department of Health/TEHS and Menzies School of Health Research (HREC 2020–3671) and was conducted in accordance with the Declaration of Helsinki. Individual consent from the study participants was not obtained, as the study was retrospective in nature and no active positional therapy device or CPAP interventions were investigated during this study. Investigators involved in this study are the usual specialist physicians for the patients included in this study and have access to patients’ medical records and sleep study reports as a part of their usual medical care. Hence, separate patients’ consent to access their medical records or the sleep study reports was not required and was approved by local ethics committee.
Results
Clinical Characteristics of the Study Participants
A total of 1463 adult patients (≥18 years old) underwent a diagnostic sleep study with complete PSG recording at the DRSH centre between January 2018 and December 2019. Of these; 3% (n=39) sleep studies failed, 3% (n=42) had no positional data, 11% (n=161) recorded <30 minutes in supine position, 15% (n=212) recorded <30 minutes in other sleep positions, 2% (n=28) had <4 hours total sleep and 2% (n=35) had discrepancies in records between overall and positional sleep and were excluded from further analysis, resulting in complete records for 65% (n=946) of participants.
The majority of participants were male (62%, n=583), non-Indigenous Australian (92%, n=886) and lived in the urban Darwin region (90%, n=852) (Table 1). Participants tended to be middle-aged (48 years IQR 37, 58.7), overweight (BMI 31.37, IQR 27.67, 36.29) and almost half (44%, n=413) had at least one comorbidity (Heart disease, hypertension, diabetes or mental health issues). A total of 86% (n=810) of participants were recorded to have OSA, of which 36% (n=291) were mild, 29% (n=233) moderate, and 35% (n=286) severe.
 |
Table 1 Clinical and Demographic Characteristics of the Study Participants |
Positional Obstructive Sleep Apnea Data
POSA was calculated to be present in 61% (n=495) of the study cohort with OSA. The clinical characteristics of individuals with POSA compared to those with non-POSA differed significantly (Table 2). A significantly higher proportion of participants with POSA were male (68% vs 60%, p=0.013), non-Indigenous (93% vs 87%, p=0.004) and reported consuming alcohol (72% vs 62%, p=0.001). POSA participants had a lower prevalence of comorbidities, significantly reduced BMI (30.84 (27.46, 35.11) vs 34.72 (30.31, 39.74), p<0.001) and had milder severity of OSA.
 |
Table 2 Comparison of Clinical and Demographic Factors Between POSA and Non-POSA |
Logistic regression identified few predictive factors for POSA in our study cohort. In univariate models’ female sex, Indigenous status, presence of diabetes or hypertension and increased corpulence were all significantly and negatively correlated with POSA (Table 3). Alcohol consumption was the single predictor significantly and positively associated with POSA (OR 1.59, 95% CI 1.18, 2.15, p=0.003). The fit of the model was consistently minor however, with R2 ranging from 0.005 (female sex) to 0.055 (BMI). On adjustment in the combined model only increasing BMI retained significance with obesity class II (BMI>35) significantly and negatively correlated with POSA (OR 0.29, 95% CI 0.13, 0.62, p=0.002) (Figure 1). Overall fit remained low, though the model reached significance (R2=0.066, p<0.001).
 |
Table 3 Logistic Regression Models Displaying Odds Ratios and Confidence Intervals for Clinical and Demographic Factors on Presence of POSA |
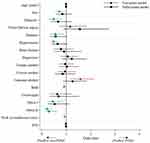 |
Figure 1 Univariate and multivariate logistic regression effects of clinical and demographic factors on odds of POSA outcome |
Significant differences were noted between participants with POSA and those without POSA in PSG parameters (Table 4). Participants with POSA spent significantly less time in non-rapid eye movement (NREM) stage-N2 sleep (p=0.047) and more in NREM-N3 (p<0.001). Though there was no significant difference in the median proportion of time spent in REM sleep, there was a significant difference in the distribution between groups. Participants with POSA had reduced AHI’s in total and in each of rapid eye movement (REM) and non-rapid eye movement (NREM) sleep stages (p<0.001), and reduced total arousal indexes (p=0.031); however, they had heightened spontaneous arousals (p=0.001). Oxygen saturation was greater at each measured point for participants with POSA (p<0.001), and distribution plots show a significantly shortened low end tail (Figure 2).
 |
Table 4 Comparison of PSG Parameters Between Participants with POSA and Non-POSA |
Treatment Simulation
Treatment was simulated and assessed only among patients who demonstrated to have POSA (Table 5). Significant differences were noted for the majority of parameters between PT and CPAP therapy. PT consistently resulted in significantly lesser reductions in AHI across each severity level (p<0.001); however, differences compared to pre-treatment simulation were still significant. Among participants with mild OSA severity and POSA, simulated PT resulted in almost half of participants fully recovering (44% vs 77% PT and CPAP, respectively, p<0.001). Among participants with either moderate or severe POSA, the vast majority (77% and 84%, respectively) demonstrated reductions in OSA severity; however, this was significantly smaller than for CPAP simulation (100% and 98%, respectively, p<0.001). Overall, PT simulation demonstrated clinical improvement for two-thirds (65%) of patients with POSA.
 |
Table 5 Effects of Treatment Simulation for Participants with POSA Using Either PT or CPAP by Severity of OSA |
Discussion
Our study demonstrates that POSA is prevalent among Australian adult males and more so among non-Indigenous Australians. POSA was also noted to be associated with alcohol consumption, among those with lowish BMI and with milder severity of OSA. Model simulation showed PT is beneficial not only among those with milder severity of OSA but also amongst patients with moderate to severe OSA.
Previous studies in the Australian setting, including studies from our centre, have shown that OSA is highly prevalent in this population.30–33 However, studies exploring the prevalence of POSA and the impact on PT have been sparse in this regional and remote Australian population, especially among the NT Australian cohort. Hence, we believe our study may be of value in understanding the demographic, clinical and PSG profile of POSA in this population. In this study, POSA was noted in 61%, in line with previous reports11–14 and was predominantly noted among males (62%) and in non-Indigenous Australians (92%). This translates to three in every five patients with OSA have POSA and thus may merit greater focus and interventions. Although the number of Indigenous Australians in the current study was relatively small, it was enough to note a significantly reduced prevalence of POSA in comparison to non-Indigenous Australians (though this effect was alleviated in multivariate regression analysis). Indigenous Australian patients generally have a higher severity of OSA32 and higher BMI, which may thus be the reason for lesser likelihood of POSA, and the reason for the amelioration of significance in multivariate analysis. There exists evidence in the literature for differences in POSA prevalence among differing ethnicities, most notably a potential increased prevalence among patients of Asian ethnicity compared to Caucasian, which may be related to differences in the craniofacial structure.11–16,29 Further evidence from direct correlation studies however is lacking.
In the current study, a significantly higher proportion of participants with POSA were male in comparison to those without POSA. The gender differences in the clinical manifestations OSA are documented in the literature, including body position that may influence the presence and severity of OSA.31,37–39 The reason for this difference is not clear, but probably a reflection of the differences in adipose tissue distribution between the two genders.40–42 It was beyond the scope of the current study to explore the underlying POSA gender difference in detail; however, future research may be warranted.
We also observed POSA was more prevalent among patients with self-reported alcohol consumption history. Alcohol consumption is known to increase the likelihood to OSA,43 but its relationship with POSA has been sparingly explored. However, it may be reasonable to speculate that alcohol may suppress the arousal response to upper airway obstruction during sleep, hence, suppressing the natural response to change in body position during an apnoeic episode, in turn facilitating higher episodes of POSA with alcohol consumption. Furthermore, alcohol may exert its action on upper airway dilator muscles and also alcohol may be associated with central adiposity with subsequently increasing diaphragm pressure and increasing upper airway collapsibility.44
Our study, in line with the majority of previous literature reporting on prevalence of POSA and the severity of OSA, found the prevalence of POSA was higher in patients with milder OSA and reduced with increasing severity of the OSA.12–14,16,28,29,37,45 It is likely that as the disease severity progresses the positional variability of the obstructive events is lost, and events start being observed in all body positions.46,47 This may also be the reason that POSA is more commonly observed in patients with lower BMI, as BMI generally correlates with OSA severity.31,32,41,46,47 Moreover, in our study, the PSG parameters showed POSA patients had higher NREM stage N2, N3 sleep and higher oxygen saturation, which could also be a reflection of this milder disease severity in this group.
Despite CPAP being established as a gold standard treatment modality for moderate to severe OSA, adherence to CPAP has consistently been noted to be low.24,45,48–50 The simulation model in our study illustrates that PT may be beneficial in most patients with POSA, even among patients with moderate to severe OSA. The overall simulated PT impact in this group of patients, although lesser than that of CPAP, still resulted in two-thirds of patients demonstrating clinically significant improvement. Furthermore, simulated PT resulted in almost half (44%) of POSA patients reducing their AHI’s to <5, and thus no longer being classified as having any form of OSA. This highlights the potential role of PT in the management of OSA,51 especially in patients who are unwilling to use, unable to adopt/adhere/tolerate/limited access or afford CPAP therapy. Nevertheless, in general, adherence to earlier forms of PT including using traditional tennis ball technique have been low as well.52,53 However, the long-term adherence to PT has improved in the recent past with the use of newer generation devices that appear to be much more comfortable and acceptable/applicable.54–60
Our study has shown that POSA is prevalent in this regional and remote Australian population studied and the simulated PT model demonstrates that PT may be beneficial among not only in patients with milder OSA but also among those with moderate to severe OSA and PT could be a potential alternate modality in treating OSA, especially among patients who may have difficulty in the affordability/accessibility or intolerant to CPAP therapy. Further prospective research using novel PT devices is however warranted in this population.
Study Limitations
This is a retrospective study of 946 patients from a single centre observed on a single night; thus, the findings may not be generalized. Australian Indigenous patients (8%) may be under-represented in this study to judge the true impact of ethnic status on POSA determinants. The number of patients from rural and remote region represented in this study was less in comparison to patients living in urban area. This may also indicate that access to health-care service may be limited in patients living in remote communities. Females constituted 38% of our patients and this may have some impact on the assessment of gender on POSA as well. We have used one of the common Cartwright criteria of POSA and the results may vary if other criteria were used. In our simulation protocol we assumed that by using PT, supine sleep time is reduced to 40%, although the recent PT studies have reported almost 84% reduction in supine sleep.49 Our study assumed 60% compliance to CPAP which may vary in different clinical scenarios impacting the results. Despite these limitations, the study illustrates that POSA is extremely common and PT can benefit some of these patients.
Conclusion
Our study highlights, POSA is highly prevalent in the adult Australian population in this region. Positional therapies may provide a viable alternative to number of OSA patients. This may potentially change our treatment paradigm for OSA and may provide a significant advantage in health-care cost.
Abbreviations
AHI, Apnea-Hypopnea Index; ASA, Australian Sleep Association; ATSI, Aboriginal and/or Torres Strait Islander; BMI, body mass index; CI, confidence interval; CPAP, continuous positive airway therapy; DPH, Darwin Private Hospital; DRSH, Darwin Respiratory and Sleep Health; ESS, Epworth Sleepiness Scale; HREC, Human Research Ethics Committee; IQRs, interquartile ranges; NATA, National Association of Testing Authorities; NT, Northern Territory; ORs, odds ratios; OSA, obstructive sleep apnea; POSA, positional sleep apnea; PPs, positional patients; PSG, polysomnography; PT, positional therapy; RA, Regional Australia; RDH, Royal Darwin Hospital; REM, rapid eye movement; NREM, non rapid eye movement; TEHS, Top End Health Service.
Summary
Sleep apnea is a global epidemic that is being increasingly recognised around the world, including among various socioeconomic groups and people living in remote and regional areas of Australia. Currently, the major treatment modality for sleep apnea has been the use of continuous positive airway therapy device and the applicability/monitoring of which poses many logistic challenges to those who have lesser access to health-care services. A phenotypic variant of sleep apnea is “positional sleep apnea”, where the apneas are predominantly noted during certain body positions. Altering the body position during sleep may help in alleviating the apnoeic episodes. However, there is sparse evidence in the literature regarding the prevalence or the effects of positional therapy in the regional and remote Australian population. Our study has demonstrated that positional sleep apnea is highly prevalent in the regional and remote adult Australian population and more commonly noted among males, younger adults, individuals who consume alcohol and in those with a lower body mass index and patients who display lesser overall severity of sleep apnea. Moreover, the model simulation of positional treatment effect in our study shows that positional treatment may be a promising alternate effective therapeutic modality that could help in the treatment paradigm for sleep apnea among vulnerable and underprivileged populations around the world.
Acknowledgments
We extend our sincere gratitude to the administrative staff Ms Tiziana Buysman, Mrs. Elisha Gamorot and sleep technologist Ms. Charmain Atos, Ms. Ara Perez, Mr. Jessie Crespo, Mr. Mark Ramirez and Ms. Bianca Al-Dossary at Darwin Respiratory and sleep health for their contribution towards this study. We also thank Dr David Cunnington, Respiratory and Sleep specialist from the Melbourne Sleep Disorders Centre, Victoria Pde, East Melbourne VIC, Australia for his expert opinion and advice.
Institution where work was performed: Department of Respiratory and Sleep Medicine, Royal Darwin Hospital, Darwin, Northern Territory, Australia and Darwin Respiratory and Sleep Health, Darwin Private Hospital, Darwin, Northern Territory, Australia. 0810.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare no conflicts of interest.
References
1. Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi:10.1016/j.smrv.2016.07.002
2. Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7:687–698. doi:10.1016/S2213-2600(19)30198-5
3. Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–1384.
4. Leung RS, Bradley TD. Sleep apnea and cardiovascular disease. Am J Respir Crit Care Med. 2001;164:2147–2165. doi:10.1164/ajrccm.164.12.2107045
5. Kasai T, Floras JS, Bradley TD. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation. 2012;126:1495–1510. doi:10.1161/CIRCULATIONAHA.111.070813
6. Marshall NS, Wong KKH, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–1086.
7. Deacon NL, Jen R, Li Y, et al. Treatment of obstructive sleep apnea prospects for personalized combined modality therapy. Ann Am Thorac Soc. 2016;13:101–108. doi:10.1513/AnnalsATS.201508-537FR
8. Zinchuk A, Yaggi HY. Phenotypic subtypes of OSA. A challenge and opportunity for precision medicine. Chest. 2020;157:403–420. doi:10.1016/j.chest.2019.09.002
9. Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep. 1984;7:110–1114.
10. Berry RB, Albertario CL, Harding SM, et al. For the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: rules, Terminology and Technical Specifications. Version 2.5. Darien, IL: American Academy of Sleep Medicine; 2018.
11. Iannella G, Magliulo G, Lo Iacono CAM, et al. Positional Obstructive sleep apnea syndrome in elderly patients. Int J Environ Res Public Health. 2020;17:1120. doi:10.3390/ijerph17031120
12. Heinzer R, Petitpierre NJ, Marti-Soler H, et al. Prevalence and characteristics of positional sleep apnea in the HypnoLaus population-based cohort. Sleep Med. 2018;48:157–162. doi:10.1016/j.sleep.2018.02.011
13. Jorquera AJ, Labarca TG, Dreyse DJ, et al. Clinical differences in positional obstructive sleep apnea patients. Rev Chil de Enfermedades Respir. 2017;33:14–20.
14. Laub RR, Mikkelsen KL, Tønnesen P. Prevalence of positional obstructive sleep apnea and patients characteristics using various definitions. Eur Respir J. 2015;46:PA2372. doi:10.1183/13993003.congress-2015.PA2372
15. Olabimpe O, Quan SF. Positional therapy in the management of positional obstructive sleep apnea—a review of the current literature. Sleep Breath. 2018;22:297–304. doi:10.1007/s11325-017-1561-y
16. Oksenberg A, Gadoth N, Töyräs J, et al. Prevalence and characteristics of positional obstructive sleep apnea (POSA) in patients with severe OSA. Sleep Breath. 2020;24:551–559. doi:10.1007/s11325-019-01897-1
17. Streatfeild J, Hillman D, Adams R, et al. Cost-effectiveness of continuous positive airway pressure therapy for obstructive sleep apnea: health care system and societal perspectives. Sleep. 2019;42(12):
18. McEvoy RD, Antic NA, Heeley E, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375:919–931. doi:10.1056/NEJMoa1606599
19. Zozula R, Rosen R. Compliance with continuous positive airway pressure therapy: assessing and improving treatment outcomes. Curr Opin Pulm Med. 2001;7:391–398. doi:10.1097/00063198-200111000-00005
20. Ulander M, Johansson MS, Ewaldh AE, et al. Side effects to continuous positive airway pressure treatment for obstructive sleep apnoea: changes over time and association to adherence. Sleep Breath. 2014;18:799–807. doi:10.1007/s11325-014-0945-5
21. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–258.
22. Yang MC, Lin CY, Lan CC, et al. Factors affecting CPAP acceptance in elderly patients with obstructive sleep apnea in Taiwan. Respir Care. 2013;58:1504–1513. doi:10.4187/respcare.02176
23. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–178. doi:10.1513/pats.200708-119MG
24. Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45:43. doi:10.1186/s40463-016-0156-0
25. Kendzerska T, Mollayeva T, Gershon AS, et al. Untreated obstructive sleep apnea and the risk for serious long-term adverse outcomes: a systematic review. Sleep Med Rev. 2014;18:49–59. doi:10.1016/j.smrv.2013.01.003
26. Simon-Tuval T, Reuveni H, Greenberg-Dotan S, et al. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32:545–552. doi:10.1093/sleep/32.4.545
27. Lee CHK, Leow LC, Song PR, et al. Acceptance and adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea (OSA) in a Southeast Asian privately funded healthcare system. Sleep Sci. 2017;10:57–63. doi:10.5935/1984-0063.20170010
28. Joosten SA, O’Driscoll DM, Berger PJ, et al. Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev. 2014;18:7–17. doi:10.1016/j.smrv.2013.01.005
29. Chou YT, Yang TM, Lin CK, et al. Pay attention to treating a subgroup of positional obstructive sleep apnea patients. J Formos Med Assoc. 2017;116:359–365. doi:10.1016/j.jfma.2016.06.007
30. Adams RJ, Appleton SL, Taylor AW, et al. Sleep health of Australian adults in 2016: results of the 2016 Sleep Health Foundation national survey. Sleep Health. 2017;3:35–42. doi:10.1016/j.sleh.2016.11.005
31. Mehra S, Ghimire RH, Joy J, et al. Gender differences in the clinical and polysomnographic characteristics among australian aboriginal patients with obstructive sleep apnea. Nat Sci Sleep. 2020;12:593–602. doi:10.2147/NSS.S258330
32. Heraganahally SS, Kruavit A, Oguoma VM, et al. Sleep apnoea among Australian Aboriginal and non-Aboriginal patients in the Northern Territory of Australia—a comparative study. Sleep. 2020;43(3):zsz248. doi:10.1093/sleep/zsz248
33. Kruavit A, Fox M, Pearson R, et al. Chronic respiratory disease in the regional and remote population of the northern territory top end: a perspective from the specialist respiratory outreach service. Aust J Rural Health. 2017;25:275–284. doi:10.1111/ajr.12349
34. Estimates of Aboriginal and Torres Strait Islander Australians. Australian bureau of statistics. Canberra; June 2016. Available from: https://www.abs.gov.au.
35. Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS): volume 5—Remoteness Structure, July 2011. ABS cat. no. 1270. 0.55.005. Canberra: Australian Bureau of Statistics; 2013a.
36. Kulkas A, Leppänen T, Nikkonen S, et al. Required CPAP usage time to normalize AHI in obstructive sleep apnea patients: a simulation study. Physiol Meas. 2018;39(11):115009. doi:10.1088/1361-6579/aae7fe
37. Joosten SA, Hamza K, Sands S, et al. Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology. 2012;17:99–107. doi:10.1111/j.1440-1843.2011.02037.x
38. O’Connor C, Thornley KS, Hanly PJ. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161:1465–1472. doi:10.1164/ajrccm.161.5.9904121
39. Lin CM, Davidson TM, Ancoli-Israel S. Gender differences in obstructive sleep apnea and treatment implications. Sleep Med Rev. 2008;12:481–496. doi:10.1016/j.smrv.2007.11.003
40. Millman RP, Carlisle CC, McGarvey ST, et al. Body fat distribution and sleep apnea severity in women. Chest. 1995;107:362–366. doi:10.1378/chest.107.2.362
41. Romero-Corral A, Caples SM, Lopez-Jimenez F, et al. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137:711–719. doi:10.1378/chest.09-0360
42. Young T, Palta M, Dempsey J, et al. The occurrence of sleep disordered-breathing among middle aged adults. N Engl J Med. 1993;328:1230–1235. doi:10.1056/NEJM199304293281704
43. Simou E, Britton J, Leonardi-Bee J. Alcohol and the risk of sleep apnoea: a systematic review and meta-analysis. Sleep Med. 2018;42:38–46. doi:10.1016/j.sleep.2017.12.005
44. Stadler DL, McEvoy RD, Sprecher KE, et al. Abdominal compression increases upper airway collapsibility during sleep in obese male obstructive sleep apnea patients. Sleep. 2009;32:1579–1587. doi:10.1093/sleep/32.12.1579
45. Bouloukaki I, Pataka A, Steiropoulos P, et al. Positional obstructive sleep apnea in the European Sleep Apnoea Database (ESADA). Eur Respir J. 2018;52:PA4335. doi:10.1183/13993003.congress-2018.PA4335
46. Joosten SA, Hamilton GS, Naughton MT. Impact of weight loss management in OSA. Chest. 2017;152:194–203. doi:10.1016/j.chest.2017.01.027
47. Joosten SA, Khoo JK, Edwards BA, et al. Improvement in obstructive sleep apnea with weight loss is dependent on body position during sleep. Sleep. 2017;40(5). PMID: 28444355. doi:10.1093/sleep/zsx047.
48. Heraganahally SS, Zaw KK, Tip S, et al. Obstructive sleep apnoea and adherence to continuous positive airway therapy among Australian women. Int Med J. 2020. doi:10.1111/imj.15076
49. Heraganahally SS, White S. A cost-effective novel innovative box (C-Box) to prevent cockroach infestation of continuous positive airway pressure equipment: a unique problem in Northern Tropical Australia. Am J Trop Med Hyg. 2019;1–4. doi:10.4269/ajtmh.19-0434
50. Heraganahally SS, Kerslake C, Issac S, et al. Outcome of public hospital-funded continuous positive airway therapy device for patients with obstructive sleep apnoea: an Australian Perspective Study. Sleep Vigilance. 2020. doi:10.1007/s41782-020-00114-4
51. Joosten SA, Edwards BA, Wellman A, et al. The effect of body position on physiological factors that contribute to obstructive sleep apnea. Sleep. 2015;38:1469–1478. doi:10.5665/sleep.4992
52. de Vries GE, Hoekema A, Doff MH, et al. Usage of positional therapy in adults with obstructive sleep apnea. J Clin Sleep Med. 2015;11:131–137. doi:10.5664/jcsm.4458
53. Bignold JJ, Deans-Costi G, Goldsworthy MR, et al. Poor long-term patient compliance with the tennis ball technique for treating positional obstructive sleep apnea. J Clin Sleep Med. 2009;5:428–430. doi:10.5664/jcsm.27597
54. Lorenzi-Filho G, Almeida FR, Strollo PJ. Treating OSA: current and emerging therapies beyond CPAP. Respirology. 2017;22:1500–1507. doi:10.1111/resp.13144
55. Jackson M, Collins A, Berlowitz D, et al. Efficacy of sleep position modification to treat positional obstructive sleep apnea. Sleep Med. 2015;16:545–552. doi:10.1016/j.sleep.2015.01.008
56. de Ruiter MHT, Benoist LBL, de Vries N, et al. Durability of treatment effects of the sleep position trainer versus oral appliance therapy in positional OSA: 12-month follow-up of a randomized controlled trial. Sleep Breath. 2018;22:441–450. doi:10.1007/s11325-017-1568-4
57. Levendowski D, Cunnington D, Swieca J, et al. User compliance and behavioral adaptation associated with supine avoidance therapy. Behav Sleep Med. 2018;16:27–37. doi:10.1080/15402002.2016.1163704
58. Ravesloot MJ, White D, Heinzer R, et al. Efficacy of the new generation of devices for positional therapy for patients with positional obstructive sleep apnea: a systematic review of the literature and meta-analysis. J Clin Sleep Med. 2017;13:813–824. doi:10.5664/jcsm.6622
59. Beyers J, Vanderveken OM, Kastoer C, et al. Treatment of sleep-disordered breathing with positional therapy: long-term results. Sleep Breath. 2019;23:1141–1149. doi:10.1007/s11325-019-01792-9
60. De Corso E, Mastrapasqua RF, Fiorita A, et al. Efficacy and long-term follow-up of positional therapy by vibrotactile neck-based device in the management of positional OSA. J Clin Sleep Med. 2020;16:1711–1719. doi:10.5664/jcsm.8664
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

