Back to Journals » OncoTargets and Therapy » Volume 11
Podoplanin-positive cancer-associated fibroblasts predict poor prognosis in lung cancer patients
Authors Hu G, Zhong K, Chen W, Wang S, Huang L
Received 28 May 2018
Accepted for publication 9 August 2018
Published 10 September 2018 Volume 2018:11 Pages 5607—5619
DOI https://doi.org/10.2147/OTT.S175566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr XuYu Yang
Guoming Hu,1 Kefang Zhong,1 Wei Chen,1 Shimin Wang,2 Liming Huang1
1Department of General Surgery (Breast and Thyroid Surgery), 2Department of Nephrology, Shaoxing People’s Hospital (Shaoxing Hospital, Zhejiang University School of Medicine), Zhejiang, China
Background: Cancer-associated fibroblasts (CAFs) are a heterogeneous population, and different subpopulations play differential roles in tumor microenvironment. However, the prognostic role of podoplanin-positive CAFs in human lung cancer still remains controversial.
Methods: Herein, we performed a meta-analysis including 12 published studies with 1,802 patients identified from PubMed and EBSCO to assess the prognostic impact of podoplanin-positive CAFs in lung cancer patients.
Results: We found that podoplanin+ fibroblast infiltration significantly decreased overall survival (OS), disease-free survival (DFS), and progression-free survival in patients. In stratified analyses, podoplanin+ fibroblast infiltration was significantly associated with worse OS and DFS in both squamous cell carcinoma and adenocarcinoma of lung. In addition, high density of podoplanin-positive CAFs significantly correlated with unfavorable clinicopathological features such as lymph node metastasis, and lymphatic, vascular, and pleural invasion of patients.
Conclusion: Podoplanin+ fibroblast infiltration leads to worse clinical outcome in lung cancer patients, implicating that it is a valuable prognostic biomarker and targeting it may have a potential for effective treatment.
Keywords: podoplanin-positive cancer-associated fibroblasts, worse outcome, lung cancer, meta-analysis
Introduction
Lung cancer is the leading cause of cancer-related death worldwide. Accumulating evidence has demonstrated that tumor-infiltrating fibroblasts (also called cancer-associated fibroblasts [CAFs]) were significantly associated with survival of lung cancer patients. However, CAFs are a heterogeneous population, and hence it is important to distinguish among different subpopulations as they may play differential roles in tumor microenvironment (TME).1 Tumor-infiltrating podoplanin+ fibroblasts, a new subset of CAFs identified recently, have been demonstrated to play specific and significant roles in human lung cancer.
Podoplanin, a well-conserved, mucin-type transmembrane protein, has exerted a variety of functions including regulation of organ development and cell motility.2 Recent studies have indicated that podoplanin was often upregulated in CAFs in the tumor stroma.3 Podoplanin+ fibroblasts are often among the early immune cells recruited to tumor sites in response to the stimuli and increase in the TME. In the last decades, multitudinous studies have associated podoplanin-positive CAFs and prognosis in lung cancer patients, but their results were controversial.4 Thus, it needs in-depth assessment, and furthermore, the potential of these cells as an effective prognostic biomarker and targeted therapy is necessary to be explored.
Herein, we performed this meta-analysis to clarify the association between podoplanin+ fibroblast infiltration and outcomes such as overall survival (OS), disease-free survival (DFS), and progression-free survival (PFS) in lung cancer patients, and thereby provided more evidence on the clinical value of podoplanin-positive CAFs as a prognostic biomarker for lung cancer.
Materials and methods
Search strategy
PubMed and EBSCO were searched for studies to evaluate the density of podoplanin-positive CAFs and survival in lung cancer patients from 1980 to April 15, 2018. The keywords adopted for search were (podoplanin [Title/Abstract] OR fibroblasts [Title/Abstract]) AND (lung [Title/Abstract] OR pulmonary [Title/Abstract]) AND (neoplasms [Title/Abstract] OR tumor [Title/Abstract] OR cancer [Title/Abstract] OR carcinoma [Title/Abstract]).
Inclusion and exclusion criteria
In this meta-analysis, the inclusion criteria were that studies included must have 1) been published as original articles; 2) investigated lung cancer patients; 3) detected podoplanin+ fibroblasts in primary tumor specimens with immunohistochemistry; 4) provided HRs with 95% CI, or Kaplan–Meier curves of podoplanin+ fibroblast density associated with OS, and/or DFS, and/or PFS; and 5) been published in English.
We excluded studies that were not published as research articles or were full texts such as commentary, case report, letters to editors, or conference abstracts. Studies that did not provide sufficient data to estimate HRs, or detected fibroblasts without using the marker “podoplanin”, or exhibited metastatic infiltration were also excluded.
End points
In this meta-analysis, OS and DFS were recorded as the primary and PFS as secondary end points. Individual studies defined cut-offs for podoplanin+ fibroblast density and classified patients into high- and low-density groups.
Data extraction
The authors GH and KZ independently reviewed and extracted data such as first author’s name, number of patients, median age, time of follow-up, method applied to quantify podoplanin+ fibroblasts, and cut-off value to determine high density of these cells. OS, DFS, PFS, and clinicopathological data including TNM stage, and lymphatic, vascular, and pleural invasion were extracted from the text, tables, or Kaplan–Meier curves.
Quality assessment
The studies included in this meta-analysis were cohort studies. Two independent authors assessed the quality of the included studies with Newcastle–Ottawa Scale (NOS),5 and achieved consensus for each item with the help of third author. The studies with score 6 or more were recorded as high-quality studies.
Statistical analysis
We combined extracted data into meta-analyses with STATA 12.0 analysis software (Stata Corporation, College Station, TX, USA). Statistical heterogeneity was assessed with the chi-squared based Q-test or I2.6 Data were pooled based on the random-effect model in the presence of heterogeneity,7 otherwise, the fixed-effect model was applied.8 Sensitivity analysis, Begg’s funnel plot, and Egger’s test9 were employed to investigate the influence of each study on the pooled results and potential publication bias, respectively. All P-values were two-sided and values less than 0.05 were considered to be statistically significant.
Result
Search results and description of studies
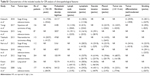
A total of 9,860 records were retrieved and the results are exhibited in Figure S1. We ultimately identified 12 studies including 1,802 lung cancer patients for the assessment of podoplanin-positive CAFs,10–21 and then evaluated all these studies with the NOS. Characteristics of the included studies which satisfied the inclusion criteria and were suitable for data consolidation are shown in Tables 1 and S1.
Meta-analyses
Overall survival
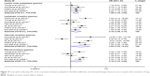
The meta-analysis showed that the elevated density of podoplanin-positive CAFs was significantly associated with decreased OS (HR=1.66, 95% CI 1.20–2.30, P=0.002) in patients with lung cancer (Figure 1).
In stratified analyses by pathologic types of lung cancer, as shown in Figure 2, pooled results indicated that high density of podoplanin-positive CAFs was significantly associated with worse OS in lung adenocarcinoma (AC) (HR=1.81, 95% CI 1.29–2.53, P=0.001); Similar result was observed with regard to podoplanin-positive CAFs and OS in squamous cell carcinoma (SCC) of lung (HR=2.00, 95% CI 1.27–3.15, P=0.003), with little heterogeneity being observed (I2=31.8%, P=0.231).
  | Figure 2 Stratified analyses describing HRs of the association between podoplanin+ fibroblast infiltration and OS. |
Disease-free survival and progression-free survival
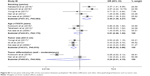
Meta-analysis showed that podoplanin+ fibroblast infiltration was significantly associated with decreased DFS (HR=1.87, 95% CI 1.07–3.26, P=0.027) and PFS (HR=1.78, 95% CI 1.22–2.58, P=0.002) in lung cancer patients (Figure 3).
As for DFS, in stratified analyses by pathologic types, we found that increased density of podoplanin+ fibroblasts within tumor was significantly associated with worse DFS in lung AC (HR=2.52, 95% CI 1.81–3.51, P=0.000), with no heterogeneity existing among included studies (I2=0.0%, P=0.689). Similar result was observed between podoplanin+ fibroblast infiltration and DFS in SCC of the lung (HR=2.33, 95% CI 1.45–3.74, P=0.000) (Figure S2).
We further investigated whether podoplanin-positive CAFs correlated with clinicopathological features such as lymph node metastasis and lymphatic invasion of lung cancer. We found that increased density of these cells was significantly associated with lymph node metastasis (OR=1.99, 95% CI 1.35–2.94, P=0.001); lymphatic (OR=2.10, 95% CI 1.06–4.13, P=0.032), vascular (OR=3.83, 95% CI 1.03–14.21, P=0.044), and pleural invasion (OR=2.19, 95% CI 1.03–4.64, P=0.041) (Figure 4); and also with tumor size (OR=0.46, 95% CI 0.32–0.66, P=0.000) and smoking (OR=2.44, 95% CI 1.39–4.27, P=0.002) status, but not with age (dichotomized according to an age of 70 years) (OR=0.81, 95% CI 0.46–1.42, P=0.463) or tumor differentiation (OR=0.24, 95% CI 0.01–4.15, P=0.324) of patients (Figure S3).
Sensitivity analysis
Sensitivity analysis indicated that each included study had no influence on the overall HR for OS or DFS (Figure S4).
Publication bias
There was no publication bias existing between podoplanin-positive CAFs and OS (P=0.876) or DFS (P=0.491) in patients by Funnel plot and Egger’s test.
Discussion
Fibroblasts play a crucial role in maintaining the structural integrity of connective tissues by continuously secreting precursors of the extracellular matrix (ECM). In the past decades, although many studies have correlated podoplanin-positive CAFs with prognosis of lung cancer patients, their results were not consistent but rather controversial. In the present meta-analysis, we found that podoplanin+ fibroblast infiltration had a negative prognostic effect associated with survival in lung cancer, especially in AC and SCC of lung. In addition, increased density of podoplanin-positive CAFs was significantly associated with lymph node metastasis; lymphatic, vascular, and pleural invasion; tumor size, and smoking status. We believe that our study is the first to provide meaningful statistical evidence exhibiting the important prognostic value of podoplanin-positive CAFs as a cancer promoter in lung cancer patients.
We thought that the following reasons could possibly be responsible for the close association between increased podoplanin-positive CAFs and decreased survival of patients identified in this study: Activated fibroblasts are able to promote tumor cell invasion, proliferation, and survival through releasing growth factors, cytokines,22 and ECM-degrading proteases such as matrix metalloproteinases.23 More importantly, podoplanin expressed in fibroblasts can enhance the ability of these cells to promote motility and survival of neighboring tumor cells through increased RhoA activity, especially in AC cells.24 Podoplanin-positive CAFs can synthesize and release angiogenic factors including IL-8 and TNF-α as well as VEGF which promote neoangiogenesis, thereby facilitating tumor growth.25 In addition, they can also produce varied amounts of immunosuppressive cytokines such as TGF-β1, IL-6, and IL-10 to inhibit antitumor immunity mediated by effector T cells,25 recruit tumor-associated macrophages via CCL2 secretion, and decrease the activation of effector T cells through their acquisition of adhesion molecules such as intercellular adhesion molecule–1 (ICAM-1),26 and thereby establishing immunosuppressive microenvironment. Thus, it is reasonable to conclude that the podoplanin-positive CAFs are able to promote tumor progression, thus decreasing survival. However, one included study reported that the presence of podoplanin-positive CAFs within tumor predicted favorable prognosis in high-grade neuroendocrine carcinomas,14 suggesting that these cells might possess antitumor property. However, further investigation is needed to validate such result.
Previous studies have demonstrated that many cancer types are rich in CAFs, such as pancreatic cancer, and can facilitate a desmoplastic TME, hindering antitumor agents from infiltrating into tumor and thereby dampening treatment efficacy to a greater extent.27 Researchers have developed several therapeutic strategies to target fibroblasts such as nano-delivery of fraxinellone and nanoparticle-mediated trapping of Wnt family member 5A to remodel the TME in preclinical studies, yielding somewhat promising results.28,29 We think our finding may provide a new strategy for effective lung cancer treatment.
There were some limitations in this study. First, morphometric analyses for podoplanin-positive CAFs used in individual included studies were not consistent. Second, there was only one study reporting the relevant data for OS in neuroendocrine carcinomas of the lung; therefore, we could not get a combined result for it. Finally, studies with negative results may not be published, which can cause potential publication bias.
In conclusion, increased density of podoplanin-positive CAFs leads to an unfavorable clinical outcome in lung cancer patients, implicating that it is a valuable prognostic biomarker and targeting it may have a potential for effective treatment.
Acknowledgments
We thank all the members of the departments who helped in this study. This work was funded by the National Natural Science Foundation of China (Grant No 81702803, GH). This work was partly funded by the projects of Zhejiang Province Scientific Research Foundation of Traditional Chinese Medicine (Grant No 2017ZB089, LH) and Science and Technology Innovation Project of Shaoxing Health and Family Planning Program (Grant No 2016CX002, WC).
Author contributions
GH conceived the study, participated in its design, extracted data, performed the statistical analysis, and drafted the manuscript. KZ participated in data extraction. WC and SW participated in the statistical analysis. LH participated in the design of the study. All authors contributed to the paper revision, agreed to be accountable for all aspects of the work and approved the final version. Guoming Hu and Kefang Zhong are co-first authors.
Disclosure
The authors report no conflicts of interest in this work.
References
Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16(9):582–598. | ||
Wicki A, Christofori G. The potential role of podoplanin in tumour invasion. Br J Cancer. 2007;96(1):1–5. | ||
Astarita JL, Acton SE, Turley SJ. Podoplanin: emerging functions in development, the immune system, and cancer. Front Immunol. 2012;3:283. | ||
Pula B, Witkiewicz W, Dziegiel P, Podhorska-Okolow M. Significance of podoplanin expression in cancer-associated fibroblasts: a comprehensive review. Int J Oncol. 2013;42(6):1849–1857. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. | ||
Kuritz SJ, Landis JR, Koch GG. A general overview of Mantel-Haenszel methods: applications and recent developments. Annu Rev Public Health. 1988;9:123–160. | ||
Dersimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–114. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Nakasone S, Mimaki S, Ichikawa T, et al. Podoplanin-positive cancer-associated fibroblast recruitment within cancer stroma is associated with a higher number of singlenucleotide variants in cancer cells in lung adenocarcinoma. J Cancer Res Clin Oncol. 2018;144(5):893–900. | ||
Kubouchi Y, Yurugi Y, Wakahara M, et al. Podoplanin expression in cancer-associated fibroblasts predicts unfavourable prognosis in patients with pathological stage IA lung adenocarcinoma. Histopathology. 2018;72(3):490–499. | ||
Yurugi Y, Wakahara M, Matsuoka Y, et al. Podoplanin expression in cancer-associated fibroblasts predicts poor prognosis in patients with squamous cell carcinoma of the lung. Anticancer Res. 2017;37(1):207–214. | ||
Koriyamai H, Ishii G, Yoh K, et al. Presence of podoplanin-positive cancer-associated fibroblasts in surgically resected primary lung adenocarcinoma predicts a shorter progression-free survival period in patients with recurrences who received platinum-based chemotherapy. J Cancer Res Clin Oncol. 2015;141(7):1163–1170. | ||
Takahashi A, Ishii G, Kinoshita T, et al. Identification of prognostic immunophenotypic features in cancer stromal cells of high-grade neuroendocrine carcinomas of the lung. J Cancer Res Clin Oncol. 2013;139(11):1869–1878. | ||
Ono S, Ishii G, Nagai K, et al. Podoplanin-positive cancer-associated fibroblasts could have prognostic value independent of cancer cell phenotype in stage I lung squamous cell carcinoma: usefulness of combining analysis of both cancer cell phenotype and cancer-associated fibroblast phenotype. Chest. 2013;143(4):963–970. | ||
Neri S, Ishii G, Taira T, et al. Recruitment of podoplanin positive cancer-associated fibroblasts in metastatic lymph nodes predicts poor prognosis in pathological N2 stage III lung adenocarcinoma. Ann Surg Oncol. 2012;19(12):3953–3962. | ||
Ito M, Ishii G, Nagai K, Maeda R, Nakano Y, Ochiai A. Prognostic impact of cancer-associated stromal cells in patients with stage I lung adenocarcinoma. Chest. 2012;142(1):151–158. | ||
Hoshino A, Ishii G, Ito T, et al. Podoplanin-positive fibroblasts enhance lung adenocarcinoma tumor formation: podoplanin in fibroblast functions for tumor progression. Cancer Res. 2011;71(14):4769–4779. | ||
Kitano H, Kageyama S, Hewitt SM, et al. Podoplanin expression in cancerous stroma induces lymphangiogenesis and predicts lymphatic spread and patient survival. Arch Pathol Lab Med. 2010;134(10):1520–1527. | ||
Kawase A, Ishii G, Nagai K, et al. Podoplanin expression by cancer associated fibroblasts predicts poor prognosis of lung adenocarcinoma. Int J Cancer. 2008;123(5):1053–1059. | ||
Yoshida T, Ishii G, Goto K, et al. Podoplanin-positive cancer-associated fibroblasts in the tumor microenvironment induce primary resistance to EGFR-TKIs in lung adenocarcinoma with EGFR mutation. Clin Cancer Res. 2015;21(3):642–651. | ||
Bruzzese F, Hägglöf C, Leone A, et al. Local and systemic protumorigenic effects of cancer-associated fibroblast-derived GDF15. Cancer Res. 2014;74(13):3408–3417. | ||
Boire A, Covic L, Agarwal A, Jacques S, Sherifi S, Kuliopulos A. PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell. 2005;120(3):303–313. | ||
Ito S, Ishii G, Hoshino A, et al. Tumor promoting effect of podoplanin-positive fibroblasts is mediated by enhanced RhoA activity. Biochem Biophys Res Commun. 2012;422(1):194–199. | ||
Poggi A, Musso A, Dapino I, Zocchi MR. Mechanisms of tumor escape from immune system: role of mesenchymal stromal cells. Immunol Lett. 2014;159(1–2):55–72. | ||
Powell DW. Myofibroblasts: paracrine cells important in health and disease. Trans Am Clin Climatol Assoc. 2000;111:271–292. | ||
Miao L, Liu Q, Lin CM, et al. Targeting tumor-associated fibroblasts for therapeutic delivery in desmoplastic tumors. Cancer Res. 2017;77(3):719–731. | ||
Liu Q, Zhu H, Tiruthani K, et al. Nanoparticle-mediated trapping of Wnt family member 5A in tumor microenvironments enhances immunotherapy for B-Raf proto-oncogene mutant melanoma. ACS Nano. 2018;12(2):1250–1261. | ||
Hou L, Liu Q, Shen L, et al. Nano-delivery of fraxinellone remodels tumor microenvironment and facilitates therapeutic vaccination in desmoplastic melanoma. Theranostics. 2018;8(14):3781–3796. |
Supplementary materials
  | Figure S1 Flowchart diagram of study selection. |
  | Table S1 Characteristics of the included studies for OR analysis of clinicopathological features |
  | Figure S2 Stratified analyses describing HRs of the association between podoplanin+ fibroblast infiltration and DFS. |
  | Figure S4 Plots describing the influence of individual studies on the overall HRs for OS (A) and DFS (B) in lung cancer patients. |
References
Nakasone S, Mimaki S, Ichikawa T, et al. Podoplanin-positive cancer-associated fibroblast recruitment within cancer stroma is associated with a higher number of singlenucleotide variants in cancer cells in lung adenocarcinoma. J Cancer Res Clin Oncol. 2018;144(5):893–900. | ||
Kubouchi Y, Yurugi Y, Wakahara M, et al. Podoplanin expression in cancer-associated fibroblasts predicts unfavourable prognosis in patients with pathological stage IA lung adenocarcinoma. Histopathology. 2018;72(3):490–499. | ||
Yurugi Y, Wakahara M, Matsuoka Y, et al. Podoplanin expression in cancer-associated fibroblasts predicts poor prognosis in patients with squamous cell carcinoma of the lung. Anticancer Res. 2017;37(1):207–214. | ||
Koriyamai H, Ishii G, Yoh K, et al. Presence of podoplanin-positive cancer-associated fibroblasts in surgically resected primary lung adenocarcinoma predicts a shorter progression-free survival period in patients with recurrences who received platinum-based chemotherapy. J Cancer Res Clin Oncol. 2015;141(7):1163–1170. | ||
Takahashi A, Ishii G, Kinoshita T, et al. Identification of prognostic immunophenotypic features in cancer stromal cells of high-grade neuroendocrine carcinomas of the lung. J Cancer Res Clin Oncol. 2013;139(11):1869–1878. | ||
Ono S, Ishii G, Nagai K, et al. Podoplanin-positive cancer-associated fibroblasts could have prognostic value independent of cancer cell phenotype in stage I lung squamous cell carcinoma: usefulness of combining analysis of both cancer cell phenotype and cancer-associated fibroblast phenotype. Chest. 2013;143(4):963–970. | ||
Neri S, Ishii G, Taira T, et al. Recruitment of podoplanin positive cancer-associated fibroblasts in metastatic lymph nodes predicts poor prognosis in pathological N2 stage III lung adenocarcinoma. Ann Surg Oncol. 2012;19(12):3953–3962. | ||
Ito M, Ishii G, Nagai K, Maeda R, Nakano Y, Ochiai A. Prognostic impact of cancer-associated stromal cells in patients with stage I lung adenocarcinoma. Chest. 2012;142(1):151–158. | ||
Hoshino A, Ishii G, Ito T, et al. Podoplanin-positive fibroblasts enhance lung adenocarcinoma tumor formation: podoplanin in fibroblast functions for tumor progression. Cancer Res. 2011;71(14):4769–4779. | ||
Kitano H, Kageyama S, Hewitt SM, et al. Podoplanin expression in cancerous stroma induces lymphangiogenesis and predicts lymphatic spread and patient survival. Arch Pathol Lab Med. 2010;134(10):1520–1527. | ||
Kawase A, Ishii G, Nagai K, et al. Podoplanin expression by cancer associated fibroblasts predicts poor prognosis of lung adenocarcinoma. Int J Cancer. 2008;123(5):1053–1059. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.