Back to Journals » Risk Management and Healthcare Policy » Volume 14
Pitfalls of Advanced Retinopathy of Prematurity Presentation: A Content Analysis of Medical Records
Authors AlBathi L, Abouammoh N, AlSwaina N, AlBalawi HB, Al Qahtani AA, Talea M, AlSulaiman SM, Abouammoh MA
Received 2 July 2021
Accepted for publication 4 September 2021
Published 16 September 2021 Volume 2021:14 Pages 3873—3882
DOI https://doi.org/10.2147/RMHP.S326757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Jongwha Chang
Lojain AlBathi,1 Noura Abouammoh,2 Nayef AlSwaina,3 Hani B AlBalawi,4 Abdullah A Al Qahtani,5 Mohammed Talea,6 Sulaiman M AlSulaiman,7 Marwan A Abouammoh1
1Department of Ophthalmology, College of Medicine, King Saud University, Riyadh, Saudi Arabia; 2Department of Community and Family Medicine, King Saud University, Riyadh, Saudi Arabia; 3Department of Ophthalmology, College of Medicine, Qassim University, Buraidah, Saudi Arabia; 4Department of Ophthalmology, College of Medicine, Tabuk University, Tabuk, Saudi Arabia; 5Department of Ophthalmology, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 6Department of Ophthalmology, Asir Central Hospital, Abha, Saudi Arabia; 7King Khaled Eye Specialist Hospital, Vitreoretinal and Uveitis Divisions, Riyadh, Saudi Arabia
Correspondence: Marwan A Abouammoh
Department of Ophthalmology, College of Medicine, King Saud University, P. O. Box 245, Riyadh, 11411, Saudi Arabia
Email [email protected]
Purpose: To identify the pitfalls in retinopathy of prematurity (ROP) screening leading to advanced disease at Ministry of Health (MOH) hospitals in Saudi Arabia.
Methods: A qualitative deductive content analysis was used to study the phenomena of defects in ROP screening. A retrospective review of medical records of newborns presenting to two tertiary eye care centers with advanced ROP (stage 4 and 5) from January 2012 to June 2019 was completed. An extensive review of the original files at the referring hospitals was conducted, including the general condition and findings of ophthalmic examination and the sequence of follow-up until the infant was discharged/referred. Data analysis was completed using pre-structured categorization matrix.
Results: Records of 29 infants with advanced stage ROP were identified. Only 13 medical records were available and obtained. The pitfalls in screening found in the study were failure to refer by the neonatologist, delayed follow-up by the ophthalmologist, failure to follow-up by the ophthalmologist, failure to diagnose by the ophthalmologist, poor documentation in patient files, unavailability of ophthalmologist, family negligence, lack of treatment and delayed referral to a higher center, and progression despite timely screening and management.
Conclusion: Although clear ROP screening guidelines are available, implementations of these guidelines are suboptimal. This study showed that the most common defect in screening is physician’s inadequacy and unavailability. A proper network of competent ROP screening physicians in all neonatal intensive care units should be established. Centers for advanced ROP surgery should be allocated to deliver a timely surgical care if needed.
Keywords: retinopathy of prematurity screening, pitfalls, content analysis
Introduction
Retinopathy of prematurity (ROP) is one of the most important causes of avoidable childhood blindness that is seen exclusively in neonates born prematurely but can be prevented if diagnosed and treated in a timely manner.1,2
It was estimated globally that more than 20,000 infants are blinded by ROP every year. In addition, 12,300 infants were reported to have mild to moderate visual impairment.3 Due to the rapidly evolving neonatal care facilities, more preterm infants are surviving. Major factors that play a role in increasing rates of blindness in ROP are linked to uneven standards of neonatal care, absence or delayed screening, and marked deficiency in trained ophthalmologists to screen and treat ROP.4
An “epidemic” of ROP causing blindness is greatly linked to socioeconomic developments and the quality and accessibility of healthcare facilities. In 2010, two-thirds of all cases of visual impairment were due to ROP in Brazil, India, Indonesia, Mexico, China, Thailand, Turkey, Iran, USA, and the Russian federation.4 Thus, middle-income countries are currently suffering from an ROP epidemic while incidence is also increasing slowly in low-income nations.5 Bowe et al found that ROP screening criteria may need to be adjusted according to the country’s NICU capabilities and unique challenges.5
In 2019, it has been shown that ROP is becoming an increasingly important cause of blindness in sub-Saharan Africa -Kenya and Nigeria in particular- as neonatal care expands. Within the decade, a new ROP epidemic is on the brink as more African countries are developing advanced neonatal intensive care units.
One of the fundamental strategies to prevent permanent blindness from ROP is establishing an effective screening program. The goal of screening is to identify infants at risk of developing ROP and those that require treatment interventions. Although not all preterm infants require treatment, ROP is a visually threatening disease that may lead to blindness, so appropriate timely screening helps diagnose and treat infants at risk.6,7
The use of content analysis of texts permit providing valid inferences to the context of their use. The use of content analysis of medical records in health research is well established.8,9 Medical records are used to represent the medical consultation event, including patients details and diagnostic and therapeutic activities undertaken. Thus, it is regarded as the best reflection of the actual consultation events without recall bias.10
The ROP screening guidelines followed by the Saudi Arabian Ministry of Health (MOH) hospitals were developed by a multidisciplinary guideline development group which included ophthalmologists and neonatologists. This was led by the National Eye Health Program at the MOH.11 The Saudi guidelines differ from the North American guidelines only in the inclusion of even older babies (<32 weeks gestational age).11
Causes of advanced ROP, and risk factors or pitfalls leading to ROP progression have been described in the literature (Table 1).12–21 To date, no study utilized content analysis of patients’ medical records to identify pitfalls of ROP screening. We aim to review pitfalls in screening of premature infants in the MOH hospitals in the country. Identifying the pitfalls will help target the defects in screening to prevent serious vision threatening complications and avoid advanced stage ROP in premature infants.
 |
Table 1 Identified Pitfalls in Retinopathy of Prematurity Screening |
Materials and Methods
Study Design
This study is a qualitative deductive content analysis following principals of inductive content analysis.22
Setting
Medical records of patients with advanced ROP in two specialised ophthalmology referral hospitals; King Khaled Eye Specialist Hospital and King Abdulaziz University Hospital, which are two tertiary eye care facilities located in Riyadh, Saudi Arabia serving as referral centers for advanced ROP cases from all over the country.
Patient Recruitment
A retrospective chart review of a consecutive series of patients presenting with advanced ROP, defined as ROP stage 4 and 5, between January 2012 and June 2019 to the two largest tertiary eye referral centers was performed. The cases were ascertained using an administrative database linked to electronic health records and cases of advanced ROP were extracted.
Infants were excluded from the study if information about the hospital they were born at was not obtainable from the records, lacking contact information, or parents were not reachable by phone. Patients were also excluded if they were born at a private hospital (non-MOH institute). Written informed consent from the patients’ parents living in Riyadh was obtained. For those who live far away and could not come to the hospital, verbal informed consent over the phone was obtained from the parents prior to data collection and this was documented in the file.
The research ethics board at the College of Medicine, King Saud University, and Institutional Review Board at King Khaled Eye Specialist Hospital approved the study which was conducted in adherence to the tenets of the declaration of Helsinki (IRB# RP1934-R).
The following represent the three main phases of content analysis as described by Elo and Kyngas.22
Data Collection
This phase represents the preparation phase for the content analysis. The place of birth {hospital/neonatal intensive care (NICU) was gathered from the files and officials at the respective hospitals were contacted to retrieve data from the files of all included infants. Information that was extracted from the files were the patients’ date of birth, national identification number, the region, and the family’s contact information. If the name of the hospital was not provided in the records, the families were contacted by phone and were asked about the hospital the infant was born in. Infants were divided according to the place/governorate of birth. Data from each file was read thoroughly and summarized in order to form a sequence of events from the time of birth until referral to the specialized center and identify causes of late presentation of infants with ROP. The following data were extracted from the files: birth weight, gestational age, gender, ophthalmic screening timings/visits and their findings, duration of NICU admission, and duration of oxygen requirement. Ophthalmic examination at these hospitals were performed by ophthalmologists at these hospitals. Poor documentation is defined as lack of standard proper documentation of the patient’s examination encounter per national guidelines.11 Delayed follow-up was defined as not abiding by the national ROP screening guidelines in following up ROP patients.11
Data Analysis
The organizing phase commenced with the formation of a categorization matrix for the content analysis. This is considered a feature of directed content analysis as proposed by Hsieh and Shannon, 2005.23 An electronic search using PubMed and the Cochrane digital library databases was conducted. Search terms of the following terms in various combinations (screening retinopathy of prematurity, advanced retinopathy of prematurity, pitfalls in screening, malpractice claims, Stage 4 and 5 ROP) were used. The search was limited to all articles related to the above terms that were published from 1996 to 2019 and to studies published in English. The search yielded ten studies related to malpractice claims in ROP screening and advanced ROP due to deficient screening (Figure 1).
 |
Figure 1 Flow chart of article extraction method conducted to retrieve related articles. |
Extracted data from relevant articles were reviewed to identify the pitfalls and shortcomings in screening ROP infants. The next step was to identify and categorize the causes of advanced ROP observed in the collected studies in order to form a categorization matrix. The categories included causes related to system, ophthalmologists/neonatologists, patients, and families. Table 1 shows all identified pitfalls from the studies organized according to a preformed categorization matrix.12–21
Data from patients’ records were reviewed and contents were coded according to the categories. An additional column titled “others” was added to allow new emerging categories from patient’s records. Each patient’s record was read several times to contract a whole understanding of the case. Then, the text was divided into meaningful units, which were summarized and identified with codes, based on the categorization matrix with the flexibility to add new codes. Finally, the codes were sorted into subcategories and main categories.24
Results
Twenty-nine infants with advanced ROP were identified from the two referral hospitals and divided into the 5 regions of the country they were born in and referred from to identify the region with the most cases of advanced ROP. Thirty percent of ROP cases were found in the central region of the country while 13% were found in the Western region (Table 2).
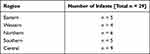 |
Table 2 Place of Birth (by Region) of Infants Found from the Included Referral Hospitals |
Information was extracted from 13 infants (Table 3). The remaining files of 16 infants from different regions in the country were not obtainable either due to lack of contact information, parents were not reachable by the recorded contact information or lack of information about the hospital where the infant was born.
 |
Table 3 Patients’ Demographics |
All patients had one or more pitfall contributing to advanced ROP as follows (Table 4): Failure to follow-up by the ophthalmologist was identified in 5 patients. Failure to diagnose by the ophthalmologist due to lack of knowledge or experience was noted in 4 patients. Failure to arrange ophthalmic screening by the neonatologist was identified in 3 patients. Failure to show for follow-up appointments due to family negligence was observed in 3 patients. Failure to deliver treatment or refer to higher center for treatment in a timely manner despite correct diagnosis was identified in 2 patients. In one patient, the disease progressed despite timely diagnosis and treatment. Table 5 lists pitfall categories by percentage of occurrence.
 |
Table 4 Categorization Matrix Showing Causes of Late Presentation of ROP Infants in Saudi Arabia |
 |
Table 5 Rate of Pitfalls in Percentage |
The following presents summaries of all included patients.
Patient 1
The neonate was screened at 33 weeks with no ROP seen in both eyes. No follow-up appointment was given, and no other ophthalmic examination was found. The child presented to the referral hospital with stage 5 ROP in the right eye and stage 4B ROP in the left eye.
Patient 2
A premature infant was admitted to NICU for 65 days. First screening and first follow-up were done in a timely manner. Follow-up exam at 33- and 34-week postmenstrual age (PMA) revealed poor visualization of both eyes and then no signs of ROP, respectively. The ophthalmologist recommended that the child should be assessed by a retina consultant. Two weeks later at 36 weeks, the infant was seen again and showed no signs of ROP in both eyes. There was an undated recommendation to refer the patient to a higher center for further assessment. However, it did not occur for an unknown reason. The child presented to the referral hospital with stage 5 ROP in both eyes.
Patient 3
One of triplets was admitted suffering from encephalopathy, developmental delay, and asthma. The infant was screened at 36 weeks and documented to have no ROP and no plus disease in both eyes. She was given a 1-week follow-up which was not performed. The child was then discharged from the NICU 2 weeks later. No documentation that an appointment was given to the family before discharge. The patient then presented to the referral hospital with Stage 5 ROP in both eyes.
Patient 4
An infant was admitted to the NICU for 7 weeks, mechanically ventilated then on oxygen nasal cannula. She was first screened at 33, 34- and 35-weeks PMA and was found to have no ROP in both eyes. Follow-up was given in 2 weeks however, the files showed that the infant was re-examined at 40 weeks and found to have Stage 3 with vitreous hemorrhage in the right eye, and Stage 2 with vitreous opacity in the left eye. The family were given a report and were told to seek care at a tertiary center. She then presented to the referral hospital with bilateral stage 5 ROP.
Patient 5
An infant was admitted to the NICU for 5 weeks. An ophthalmic exam has been ordered but was never performed. The infant was referred for to a general hospital for his medical condition and was screened by the ophthalmologist at 37 weeks PMA and found to have Stage 5 ROP in both eyes. The child was sent to the referral hospital for further management.
Patient 6
An infant was admitted to the NICU for 14 weeks. The infant was on continuous positive airway pressure and oxygen hood. The infant also had a patent ductus arteriosus (PDA), and a grade I intraventricular hemorrhage (IVH). The first ophthalmic screening was at 34 weeks and was found to have Stage 1 in Zone II in both eyes. Follow-up examinations at weeks 36 and 38 weeks revealed the same findings. Examination at 40 weeks revealed Stage 3 in Zone II with plus disease. The infant was treated with laser indirect ophthalmoscopy in both eyes twice over a 2-week period. The infant was discharged from NICU at 44 weeks. Examination at discharge revealed a flat retina with blood vessels bridging anteriorly in the right eye. Left eye was poorly dilating due to posterior synechia and a tractional retinal detachment involving the macula with a fibrotic band [Stage 4B]. The infant presented to the referral hospital with bilateral Stage 4B.
Patient 7
Premature male infant was admitted to the NICU for 12 weeks. The infant suffered from chronic lung disease and was ventilated for 8 weeks. The infant was screened once for ROP, but the physician failed to document the date and age of the infant at screening. The exam reported no ROP in both eyes with tortuous vessels, the infant was not followed up. The infant then presented to the referral hospital with bilateral Stage 5 disease.
Patient 8
A premature male infant was admitted to the NICU for 12 weeks, required oxygen for 10 weeks. The infant suffered from respiratory distress syndrome (RDS) and IVH. The infant was screened at 31 weeks and found to have bilateral vitreous hemorrhage with poor view to the fundus in both eyes. The family were informed, but the child was unstable to be transferred to an eye center for management, and the hospital did not have the equipment to deliver treatment. Eight weeks later, once the infant was stabilized, he was referred to a tertiary eye center in the region, he was immediately treated with laser indirect ophthalmoscopy in both eyes. The family then pursued a second opinion, and the infant was found to have bilateral retinal detachment. The patient was directed to the referral center and presented with bilateral Stage 4B ROP.
Patient 9
A premature infant was admitted to the NICU for 52 days, suffered from RDS, pulmonary hemorrhage with a collapsed right upper lobe and required oxygen for 6 weeks. The infant was screened at 31 weeks and was suspected to have advanced ROP. The Patient was referred to a higher center for further screening and management, but the parents refused medical advice, signed the legal forms to be discharged against medical advice and were lost to follow-up. The family then presented to the referral center and the infant was found to have Stage 4B in the right eye and Stage 5 in the left eye.
Patient 10
A premature twin was admitted to the NICU for 25 days. The infant suffered from PDA, neonatal jaundice, chronic anemia requiring multiple blood transfusions and pseudomonas eye infection. First ophthalmic screening was at 35 weeks which revealed no ROP and was given a follow-up in 2 weeks. However, the patient was seen 5 weeks later at 40 weeks of gestation due to missed follow-up by the ophthalmologist. The infant was found to have bilateral retinal detachment (Stage 4). The infant presented to the referral center at 41 weeks and was found to have bilateral stage 5 ROP.
Patient 11
A premature infant was admitted to the NICU for 25 days, suffered from sepsis and RDS. First screening was at 35 weeks post-menstrual age which revealed no ROP in both eyes, and a follow-up 2 weeks later was requested but not done by the ophthalmologist. The infant was discharged from the NICU and a follow-up ophthalmology clinic appointment was given. The clinic appointment was missed. Another follow-up appointment was arranged at 39 weeks at which the infant was found to have Stage 5 ROP in both eyes. The infant was referred to our specialized tertiary hospital.
Patient 12
A premature infant was admitted to the NICU for 8 weeks. The first ocular exam was at 36 weeks, which revealed no ROP in both eyes and was given follow-up after 2 weeks. The second exam showed the same picture, and a 3rd follow-up 2 weeks later was requested after discharge from NICU but the patient did not show up. The parents sought another opinion by a retinal specialist in a different clinic and the infant’s examination showed bilateral Stage 5 ROP. At 43 weeks the infant presented to the referral center and the diagnosis was confirmed.
Patient 13
A premature twin was admitted to the NICU for 12 weeks. The infant suffered from RDS and required oxygen for 8 weeks. First screening at 33 weeks of gestation, the general ophthalmologist documented a “normal” retinal exam with normal blood vessels, retina and a healthy disc. No follow-up was given, and no other ophthalmic exam was performed. At 42 weeks of gestation, the family brought the infant to our hospital and was found to have bilateral Stage 5 ROP.
Discussion
In the current study, a total number of 29 infants with advanced stage 4 or 5 ROP presented to two large tertiary eye centers in Riyadh, Saudi Arabia over a 6-year period. Most ROP cases were referred from the central region of the country. The pitfalls in screening found were failure to follow-up by the ophthalmologist, failure to refer by the neonatologist to ophthalmology, failure to diagnose by the ophthalmologist, poor documentation in patients’ files, family negligence (missed appointment or delayed follow-up), delayed follow-up by the ophthalmologist, lack of treatment and delayed referral to a higher center, and progression despite timely screening and management.
The pitfalls observed in our study were similar to those reported in the literature. The current study shows that in Saudi Arabia, challenges related to screening by ophthalmologists are the most frequently identified barriers to effective diagnosis and hence timely treatment of ROP patients. Additionally, the occurrence of multiple pitfalls in a single patient was not uncommon.
Aprahamian et al identified barriers to follow-up of ROP patients. Their study showed that 50% of the premature infants were not scheduled for a timely outpatient follow-up appointment, and that 20% of the infants were never brought by the parents to their scheduled appointments.12
Screening begins with the neonatologist arranging for an ophthalmic exam and ensuring that eye exam is conveyed. It was found that the neonatologist either did not request the eye exam, or did make the request but did not follow up and ensure that an ophthalmologist came to conduct the examination. Pitfalls by the ophthalmologist, however, included poor documentation of patients’ information and ophthalmic findings; failure to diagnose due to lack of knowledge regarding ROP, unsupervised resident or general ophthalmologist not competent to do ROP screening; failure to document in the file that a follow-up is to be performed or failure to show up for the follow-up. It is the ophthalmologist’s responsibility to follow-up ROP patients or refer them if the physician is unavailable or is not sure about the exam findings. Physicians must be diligent and proactive in providing care to their patients.6 Otherwise, this will lead to devastating results for premature infants at risk of ROP. It was also found that one center lacked the surgical equipment to treat one infant, and it is the ophthalmologist’s responsibility to ensure that the infant is referred and transferred to the appropriate place in a timely manner.
In Germany, Muether et al found that following the recommended screening guidelines yielded no advanced ROP stage 4 and 5 throughout 9 years. This is due to strict implementation of the screening guidelines, prompt treatment when necessary, and high level of care by neonatal intensive care unit.25 The discovery of advanced ROP despite the presence of a national guideline for screening and follow-up was comprehensively described in the current study.
Inductive content analysis was the most suitable approach to be used as although the literature is rich in studies focusing on causes of late presentation of ROP, little is known about this issue in Saudi Arabia. Furthermore, using content analysis allowed us to categorize causes of late presentation of ROP patients in relation to the existent literature and highlight the exact step or steps where suboptimum care was delivered.22
Although the MOH has a well-established guideline to diagnose, treat, and refer ROP. The study showed that some MOH hospitals are not clearly following the screening guidelines recommended for premature infants. It also showed that some ophthalmologists were not competent to perform the ROP screening, and that further training is required to prepare these physicians in order not to miss possible cases. Some cases showed parental negligence or lack of knowledge about the severity of the disease.
Hariharan et al set an example on how legislative, governmental, and economic support helped Argentina to successfully enforce legislations and resolutions that aided in decreasing childhood blindness from ROP since 2012.26 We aim that this study would identify areas of defect in the current ROP screening program which will help MOH policy makers and advocate officials to prioritize the development a national program to control blindness from ROP.
Limitations and Future Research
The study included 29 patients presenting during the period of 2012 to 2019. However, the data extraction was limited because the files were not accessible in many regions. It was also observed that documentation in many of the patients’ files was poor and unclear whether ophthalmic exam was ordered or performed which made it difficult to obtain the information needed. For referring hospitals, this is considered a grave lack of proper patient documentation, whether contact information or clinical data, which might have participated in the delay of identifying and properly managing those patients. Such lack of basic patient identification information should not be accepted in the presence of current advanced patient information systems. In addition, replicating the study might not be possible because of the differences of medical care and referral systems in this country compared to other countries.
In-depth semi-structured interviews is a qualitative methodology that is needed to explore parents understanding of ROP in addition to the barriers and motivators that could encourage them to be involved in the care process.
Recommendations
To reduce the incidence of advanced ROP in Saudi Arabia the current study recommends enforcement of implementation of screening guidelines through setting up strict key performance indicators in all hospitals with a NICU. This should ensure proper patient and family identification and establishing means of immediate reach, and the initiation and continuity of screening until the infant reaches discharge criteria. A network of ROP treating physicians should be established to cover the kingdom. This should solve any issues related to delay in treatment delivery. Alternatively, a national telemedicine ROP screening program could be implemented. This should support healthcare centers where ophthalmologists are lacking, especially in the peripheral and rural areas. This also works as a safety net to obtain second opinion in areas where an ophthalmologist is available but lacks the experience in diagnosing ROP. All of the above recommendations should attend to ROP primary prevention. Additionally, Centers of excellence for ROP surgery should be allocated and announced to deliver a timely surgical care if needed to avoid the progression to stage 5 ROP. The location of these centers should take into consideration the ease of access and reach for patients from all around the country.
Training general ophthalmologists to be competent in ROP screening, diagnosis and delivery of care is crucial. This could be performed through courses, workshops and clinical training and solve the issue of lack of knowledge and ability to deliver care.
It is fundamental to educate parents at the time of discharge about the importance of ophthalmic follow-up. Furthermore, it is possible to establish a regulation in liaison with child protection services and law enforcement bodies in the country ensuring timely follow-up of discharged neonates.
In conclusion, we found that implementation of ROP screening guidelines is not ideal as many MOH hospitals are clearly not following the guidelines for screening of premature infants. This study identified that some ophthalmologists were not competent to perform the ROP screening, and it also revealed that families may not understand the importance of ophthalmic screening and follow-up. Pitfalls in screening lead to unfavorable or catastrophic results. Thus, focused efforts by the neonatologist, ophthalmologist, healthcare workers and the family are required to prevent advanced stage of ROP, strict forceful implementation of screening guidelines is demanded, and further training is required to prepare ophthalmologists in order to be competent in ROP screening, diagnosis and delivery of care. This could be performed through courses, workshops and clinical training. A back-up safety net for the screening ophthalmologists in the form of an appropriate consultation service of a senior physician or a national telemedicine ROP screening program should be set up for borderline cases and for cases requiring a second opinion. A network of ROP treating physicians should be established to cover the kingdom. This should solve any issues related to delay in treatment delivery. Further action is also needed to spread proper awareness and education about ROP within the patient’s families and medical staff.
Data Sharing Statement
The PI can submit an access to the data of the article upon a reasonable request.
Ethics Approval
The study was approved by the Institutional Review Board at King Khaled Eye Specialist Hospital, and it was conducted in adherence to the tenets of the declaration of Helsinki.
Consent to Participate
An informed consent was obtained from the patients for the anonymous use of data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Researchers Supporting Project number (RSP-2021/330), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. McGavin DD. The global initiative for the elimination of avoidable blindness - vision 2020: the right to sight. Community Eye Health. 1999;12(30):32.
2. Shastry BS. Genetic susceptibility to advanced retinopathy of prematurity (ROP). J Biomed Sci. 2010;17(1):69.
3. Chan-Ling T, Gole GA, Quinn GE, Adamson SJ, Darlow BA. Pathophysiology, screening and treatment of ROP: a multi-disciplinary perspective. Prog Retin Eye Res. 2018;3(62):77–119.
4. Dogra MR, Katoch D, Dogra M. An update on Retinopathy of Prematurity (ROP). Indian J Pediatr. 2017;84(12):930–936.
5. Bowe T, Nyamai L, Ademola-Popoola D, et al. The current state of retinopathy of prematurity in India, Kenya, Mexico, Nigeria, Philippines, Romania, Thailand, and Venezuela. Digit J Ophthalmol. 2019;25(4):49–58.
6. Fierson WM. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;189(1):189–195.
7. Fierson WM. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2018;142(6):e20183061. doi:10.1542/peds.2018-3061
8. Karlsson A, Lidell E, Johansson M. Health-care professionals’ documentation of wellbeing in patients following open heart surgery: a content analysis of medical records. J Nurs Manag. 2013;21(1):112–120.
9. Raol N, Lilley E, Cooper Z, Dowdall J, Morris M. Preoperative counseling in salvage total laryngectomy: content analysis of electronic medical records. Otolaryngol Head Neck Surg. 2017;157(4):641–647.
10. Berg M. Practices of reading and writing: the constitutive role of the patient record in medical work. Sociol Health Illn. 1996;18(4):499–524.
11. Al Amro SA, Al Aql F, Al Hajar S, et al. Practical guidelines for screening and treatment of retinopathy of prematurity in Saudi Arabia. Saudi J Ophthalmol. 2018;32(3):222–226.
12. Aprahamian AD, Coats DK, Paysse EA, Brady-McCreery K. Compliance with outpatient follow-up recommendations for infants at risk for retinopathy of prematurity. J AAPOS. 2000;4(5):282–286.
13. Moshfeghi DM. Top five legal pitfalls in retinopathy of prematurity. Curr Opin Ophthalmol. 2018;29(3):206–209.
14. Reynolds JD. Malpractice and the quality of care in retinopathy of prematurity (an American ophthalmological society thesis). Trans Am Ophthalmol Soc. 2007;105:461.
15. Azad R, Chandra P, Gangwe A, Kumar V. Lack of screening underlies most stage-5 retinopathy of prematurity among cases presenting to a tertiary eye center in India. Indian Pediatr. 2016;9(7):S103–S106.
16. Vinekar A, Jayadev C, Dogra M, Shetty B. Improving follow-up of infants during retinopathy of prematurity screening in rural areas. Indian Pediatr. 2016;9(7):151–154.
17. Zepeda-Romero L, Meza-Anguiano A, Barrera-de León J, et al. Case series of infants presenting with end stage retinopathy of prematurity to two tertiary eye care facilities in Mexico: underlying reasons for late presentation. Matern Child Health J. 2015;19(6):1417–1425.
18. Day S, Menke AMA, Abbott RRL. Retinopathy of prematurity malpractice claims: the ophthalmic mutual insurance company experience. Arch Ophthalmol. 2009;127(6):794–798.
19. Padhi T, Badhani A, Mahajan S, et al. Barriers to timely presentation for appropriate care of retinopathy of prematurity in Odisha, Eastern India. Indian J Ophthalmol. 2019;67(6):824–827.
20. Demorest BH. Retinopathy of prematurity requires diligent follow-up care. Surv Ophthalmol. 1996;41(2):175–178.
21. Engelhard S, Collins M, Shah C, Sim A, Reddy A. Malpractice litigation in pediatric ophthalmology. JAMA Ophthalmol. 2016;134(11):1230–1235.
22. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115.
23. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
24. Graneheim U, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112.
25. Muether PS, Kribs A, Hahn M, et al. No advanced retinopathy of prematurity stages 4 or 5 in a large high-risk German cohort. Br J Ophthalmol. 2012;96(3):400–404.
26. Hariharan L, Gilbert C, Quinn G, et al. Reducing blindness from Retinopathy of Prematurity (ROP) in Argentina through collaboration, advocacy and policy implementation. Health Policy Plan. 2018;33(5):654–665.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
