Back to Journals » Drug, Healthcare and Patient Safety » Volume 7
Persistent nonmalignant pain management using nonsteroidal anti-inflammatory drugs in older patients and use of inappropriate adjuvant medications
Authors Rianon N, Knell M, Agbor Bawa W, Thelen J, Burkhardt C, Rasu R
Received 9 May 2014
Accepted for publication 26 June 2014
Published 29 January 2015 Volume 2015:7 Pages 43—50
DOI https://doi.org/10.2147/DHPS.S67425
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Nahid Rianon,1 Maureen E Knell,2 Walter Agbor-Bawa,3 Joan Thelen,4 Crystal Burkhardt,3 Rafia S Rasu3
1Division of Geriatric and Palliative Medicine, Department of Internal Medicine, University of Texas Medical School at Houston, Houston, TX, USA; 2Department of Pharmacy Practice and Administration, University of Missouri-Kansas City School of Pharmacy, Kansas City, MO, USA; 3Department of Pharmacy Practice, University of Kansas School of Pharmacy, Lawrence, KS, USA; 4Department of Psychology, University of Missouri-Kansas City, Kansas City, MO, USA
Objective: Due to the high risk of life-threatening side effects, nonsteroidal anti-inflammatory drugs (NSAIDs) are not favored for treating persistent nonmalignant pain in the elderly. We report national prescription trends with determinants of NSAIDs prescription for persistent nonmalignant pain among older patients (age 65 and over) in the US outpatient setting.
Methods: A cross-sectional analysis was performed using National Ambulatory Medical Care Survey data. Prescriptions for NSAIDs, opioids, and adjuvant agents were identified using five-digit National Ambulatory Medical Care Survey drug codes.
Results: About 89% of the 206,879,848 weighted visits in the US from 2000 to 2007 recorded NSAIDs prescriptions in patients (mean age =75.4 years). Most NSAIDs users had Medicare (75%), and about 25% were prescribed with adjuvant medications considered inappropriate for their age. Compared to men, women were 1.79 times more likely to be prescribed NSAIDs.
Conclusion: The high percentage of NSAIDs prescription in older patients is alarming. We recommend investigating the appropriateness of the high prevalence of NSAIDs use among older patients reported in our study.
Keywords: pain management, NSAIDs, inappropriate adjuvant, AGS guideline, NAMCS
Introduction
Persistent or chronic pain associated with nonmalignant medical conditions is a common chronic health problem in older adults.1 Besides incurring the high health care cost of about $635 billion in medical care and lost productivity in the US, persistent pain is also highly salient for functional impairment, sleep disturbance, decreased appetite with weight loss, and depression, ultimately leading to decreased quality of life and even failure to thrive.2–4 Medication is the most common intervention in managing persistent pain, and older patients are at greater risk of adverse drug reactions (ADRs) due to age-related physiological changes, multiple comorbidities, and polypharmacy.4–7 The American Geriatrics Society (AGS) guidelines for persistent nonmalignant pain management in older adults recommend acetaminophen as a first-line agent for mild to moderate pain.4–7 In inflammatory pain conditions, nonsteroidal anti-inflammatory drugs (NSAIDs) are known to provide superior short-term relief compared to acetaminophen.8,9 However, NSAIDs possess a higher potential for life-threatening side effects in older adults, such as gastrointestinal bleeding, renal toxicity, and cardiovascular events,10 making NSAIDs a medication to use with caution in the vulnerable elderly population. Guidelines provided by the AGS emphasize pain control with NSAIDs among patients in whom other therapies have failed and goals to control persistent pain were not achieved. However, AGS guidelines recommend doing so with great caution, and only after appropriate assessment by clinicians.4 The prevalence of NSAIDs use for persistent pain among the general US adult population has been estimated to be 95%.11 However, studies addressing NSAIDs use for persistent pain in the geriatric population worldwide have been sporadic and yield conflicting results regarding the prevalence of NSAIDs use for nonmalignant pain management.
One analysis of a national database from the 1980s and the 1990s on prescription analgesic use in older Americans reported that the prevalence of prescription NSAIDs use in the preceding month was between 8% and 13%, with greater usage rates in females (12%–13%) compared to males (8%–9%).12 Similarly, in a cohort of over 2,000 Finnish older adults, approximately 8% used NSAIDs to relieve chronic joint or back pain.13 Alternatively, in a Spanish study of over 17,000 osteoarthritis patients, nearly 80% used NSAIDs for chronic pain relief.14 While these studies provide some estimates of the prevalence of NSAIDs use among older adults, most US studies are limited to descriptions of prevalence by sex and cost related to NSAIDs prescriptions filled by older patients,15–20 and lack information on determining factors associated with NSAIDs use in the elderly. Information on factors influencing NSAIDs prescriptions among the general community-dwelling elderly population is essential for identifying risk factors and appropriateness of prescribing, and may educate clinicians on AGS guidelines to help improve health quality while adequately managing persistent pain. We describe national prescription trends with determinants of NSAIDs prescription for nonmalignant pain management among older patients (aged 65 years and over) in the US outpatient settings using the National Ambulatory Medical Care Survey (NAMCS) data from 2000 to 2007.
Methods
This cross-sectional analysis utilized data from NAMCS provided by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics from 2000 to 2007. The NAMCS employed a multistage probability design; more information about the NAMCS sampling and weighting methods can be found on the NAMCS webpage (http://www.cdc.gov/nchs/ahcd.htm).21,22
Physician–patient office visits were used as the primary sampling unit. We followed AGS guidelines to identify appropriate patients aged 65 years or older who visited outpatient clinics for nonmalignant pain management;4 these were: 1) documented by patients’ self-reported reason for visit; 2) International Classification of Diseases, Ninth Revision code for assessment of persistent nonmalignant pain recorded by physician for that visit; or 3) prescription received for pain management during that visit. Reports of chronic pain were further categorized into the four classifications of chronic pain: neuropathic, muscle, inflammatory, and mechanical/compressive, as determined by the Institute for Clinical Systems Improvement guidelines.15,16 Additionally, reports of two or more types of chronic pain by a single patient were categorized separately. The NAMCS survey used office visit forms in order to extract information regarding patients’ demographics, insurance status, reason for visit, known diagnoses, current and prescribed medication(s), and recommended services. Identification of prescriptions for NSAIDs, opioids, and adjuvant agents were identified by using the unique five-digit NAMCS drug codes. Each variable in the study was coded before beginning the statistical analysis. Because this investigation used de-identified data available through the CDC, the study was exempt from IRB review.
Bar graphs describe the trend of NSAIDs prescription in the study population over 8 years (from 2000 to 2007) with a graphic representation. Descriptive statistics report patient and physician characteristics, regional distributions, types of medication, and insurance for all patients as well as those who received NSAIDs prescriptions only for persistent nonmalignant pain. A multivariate logistic regression model using the variables described above reports the determinants of prescribing NSAIDs for persistent nonmalignant pain. The multivariate model included all visits reporting prescriptions written for NSAIDs for persistent non malignant pain. All analyses were weighted to determine nationally representative estimates. The statistical software STATA® version 11 was used for all analyses (StataCorp LP, College Station, TX, USA). Statistical significance was assessed at the P<0.05 level.
Results
We analyzed a total of 206,879,848 weighted (5,968 unweighted) outpatient visits for patients aged 65 years or older with nonmalignant pain from 2000 to 2007. About 89% of these visits recorded a clinician prescribing NSAIDs. The mean age for NSAIDs prescription recipients was 75.4 years, with the majority being women (68%) and non-Hispanic white (87.6%) (Table 1). A large percentage of the NSAIDs users had Medicare (75%), while 15% had private insurance. Most patients with NSAIDs (68.8%) received a total of four or fewer prescriptions during the outpatient visit (Table 1). About a quarter of the NSAIDs users were also prescribed adjuvant agents that are considered inappropriate for the geriatric population (Table 1).
Figure 1 displays the trend of NSAIDs use nationally in older adults (aged 65 years and over) from 2000 to 2007. Although fluctuations were observed, there was no significant increasing or decreasing trend in the prescribing of NSAIDs among the geriatric population during the study period.
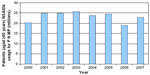  | Figure 1 Patients (aged ≥65 years) NSAIDs usage 2000–2007. |
Table 2 reports determinants of NSAIDs prescribing in the geriatric population. Sex, geographical region, number of concurrent medications, and provider status significantly impacted prescribing patterns (P<0.05). Women were 1.79 times more likely to be prescribed NSAIDs for persistent nonmalignant pain compared to men. Patients on four or fewer medications were 12.4 times more likely to be prescribed NSAIDs compared to patients with five or more medications. Primary care providers (PCPs) were 37% less likely to prescribe NSAIDs compared to non-PCPs.
Discussion
In the current study sample, a large percentage (89.6%) of older adults were prescribed NSAIDs for treating persistent nonmalignant pain in outpatient settings. Compared to men, women had a higher likelihood of receiving a prescription for NSAIDs. Patients with concomitant use of four or fewer prescriptions or visiting a PCP were less likely than patients with at least five prescriptions or visiting non-PCPs to receive NSAIDs in our study. Our finding of high percentages of NSAIDs prescription use in the study sample is alarming for patients who are at risk of ADRs due to their age. However, it is consistent with a CDC briefing that reported analgesics to be the most common drug category mentioned during outpatient physicians’ office visits in 2007,23 with NSAIDs being the most commonly prescribed type of analgesics for adults over age 65.24 Our data reports a much higher percentage of NSAIDs prescription compared to previous estimates; we report 18%–40% of adults aged 65 years and older filling at least one NSAIDs prescription each year.25,26 Despite the presence of specific guidelines that caution the use of NSAIDs among older adults due to the risk of ADRs and hospitalizations, our report from a national database is concerning for the quality of care in older patients, specifically women, who are seeking pain management for persistent nonmalignant pain.
About 75% of the current study patients receiving NSAIDs prescriptions had Medicare insurance. This is consistent with a report that drug mention rates are significantly higher for office visits among patients with Medicare as their main expected source of payment.24
Our report of women’s increased likelihood to receive NSAIDs compared to men, as well as higher percentages (68%) of women receiving NSAIDs, is consistent with a previous report of the third National Health and Nutrition Examination Survey (NHANES III) data from the 1980s and 1990s.27,28 Longer life expectancies among women, with a greater number of women than men among the geriatric patient population in the US,27 may also explain these findings. Women are also known to account for a disproportionately larger share of expenditures for NSAIDs, with more women (12.2%–13.0%) using NSAIDs prescriptions than men (8.1%–9.1%) of similar age (≥65 years) in the US.12,29 This is similar to a national drugstore chain report on prescription dispensing, which documented a higher likelihood of dispensing anti-inflammatory drugs for older women compared to men (odds ratio =1.70, 95% confidence interval: 1.70–1.70).17
We found that PCPs were 37% less likely to prescribe NSAIDs compared to non-PCPs in this geriatric population (Table 2). Among those patients receiving an NSAIDs prescription, 26.8% saw an internal medicine specialist, while 20.9% of these visits occurred with a family practitioner (Table 1). Conversely, physicians specializing in geriatrics and pain medicine prescribed the smallest percentage of NSAIDs (Table 1). Results from the NAMCS data from 2003 to 2004 showed that the annual rate of reported medications (ie, prescription and over the counter medications, immunizations, allergy shots, anesthetics, and dietary supplements that were ordered, supplied, administered, or continued during a visit) in primary care offices increased significantly between 1993–1994 and 2003–2004.24 For patients aged 65 years and older, the annual rate of reported number of medications was highest in primary care office visits compared to all other settings.24 It has been previously reported that PCPs treat 52% of chronic pain patients.18 We report consistent data, such that 52.3% of all geriatric patients with persistent nonmalignant pain visited a PCP, and 50.6% of all geriatric patients receiving a prescription for NSAIDs visited a PCP. Our study reports lower percentages of NSAIDs prescribed by PCPs compared to non-PCPs. Continuation of care with appropriate medication reconciliation by PCPs may be a protective factor for preventing ADRs due to NSAIDs use in patients treated by PCPs. Special training in geriatrics and pain management may have led to the reduced percentage of prescriptions written by physicians from these specialties. However, a low number of specialty physicians in these categories, as well as PCPs with advanced training categorizing themselves as PCPs (as opposed to geriatricians or pain specialists who are treating persistent pain) may have biased the outcome by misreporting the specialty type as PCPs. That said, it is beyond our scope of investigation to tease out such a discrepancy from the current data analysis. We recommend future studies targeting geriatricians and pain management specialties to more precisely assess the appropriate adherence to AGS guidelines for managing persistent nonmalignant pain among elderly patients.
The use of NSAIDs for persistent pain among the general adult population in the US from 2000 to 2007 was approximately 95%.11 In comparison, 89.6% of the geriatric population in the current study had a prescription for NSAIDs use. Continuity of care by PCPs is important in improving quality of care. Judicious prescribing of appropriate medications to improve persistent pain management and avoid ADRs are among the primary goals of the current AGS guidelines. As a chronic health problem, PCPs from family medicine and internal medicine with or without advanced training in either geriatrics and/or pain management may play an important role in treating persistent nonmalignant pain among older patients. Our report of reduced likelihood of NSAIDs prescriptions by PCPs indicate a positive step toward persistent pain management when patients are treated by PCPs. It is common for older adults to use multiple medications to treat multiple concurrent health conditions, such as hypertension, diabetes, high cholesterol, depression, arthritis, and musculoskeletal and chronic pain.19,20 The government agency Administration on Aging reported that, in 2009, nearly one-quarter of Medicare beneficiaries had greater than four comorbid conditions.27 The prevalence of polypharmacy, or use of multiple concurrent medications, increases with advanced age.30 Polypharmacy is also associated with a higher potential for ADRs, with worse outcomes in the elderly.31,32 The relationship between polypharmacy and ADRs among older adults is likely due to age-related changes in physiology, as well as pharmacodynamics and pharmacokinetics of medications.32,33 Close to two-thirds of our study population (68.8%) received a total of four prescriptions during their outpatient visits. Furthermore, in our sample, patients using four or fewer medications were 12.4 times more likely to be prescribed NSAIDs for persistent nonmalignant pain compared to patients with five or more medications. The prevention of ADRs by prescribing appropriate medications for multiple comorbidities while protecting patients from polypharmacy and following published AGS guidelines may be a possible explanation as to how patients with polypharmacy (at least five medications) were less likely to get NSAIDs for chronic pain management in our study. This cross-sectional survey is limited in reporting physicians’ knowledge or attitude toward prescribing and whether or not they followed AGS guidelines. A separate future survey on physicians’ knowledge and attitudes on the relevant topic may help confirm assumptions based on our findings.
Opioids and adjuvant agents are recommended for moderate to severe pain, as well as pain that causes functional impairment or diminishes quality of life. Our data showed that approximately 10% of the older adults receiving NSAIDs prescriptions also used an opioid drug, while 26% also used some type of adjuvant agent (such as a tricyclic antidepressant [TCA] or muscle relaxant). Previous estimates of opiate use among older adults living at home ranged between 2.8% and 6.6%, and about 30% among the nursing home residents suffering from persistent nonmalignant pain.17,34 In comparison, a study of community-dwelling older adults in Finland reported that 18.5% received opiate prescriptions for pain relief.13 Like NSAIDs, opioid drugs possess the potential for ADRs in older adults, including delirium, gastrointestinal symptoms, respiratory depression, and increased risk of injuries due to falls, thereby presenting a barrier to the long-term use of opioids.35–37 In addition to guidelines for opioids (as appropriate based on clinicians’ assessment) for uncontrolled persistent nonmalignant pain, the AGS also provides recommendation for adjuvant therapies.4 The guidelines for adjuvant therapies provide information on side effects including those of high significance due to serious consequences, eg, fall and related injuries, confusion or deliriums. TCAs are adjuvants with “significant” side effects (as described in the AGS guidelines) and therefore, are recommended to be avoided in patients with syncope or delirium and to be used only when other suitable medications are contraindicated for those patients.38 Muscle relaxants are another group of medications with severe side effects, eg, fall, a “never” event for older hospitalized patients. Although not very high in percentages, both TCAs and muscle relaxants were prescribed as adjuvants in our study sample. Our study is limited in scope to describe whether specific comorbidities would make it inappropriate to use adjuvants (eg, TCAs and muscle relaxants) in our study population. Yet, the use of adjuvants with significant side effects that are also listed as inappropriate for use in the elderly by Beer’s criteria4,38 indicates the need to evaluate and educate prescribers on AGS guidelines for persistent nonmalignant pain management. Future research on prescription pattern by physicians may help explore the need for educational intervention.
Older adults are more likely to be hospitalized due to ADRs than younger patients,39,40 and about 23% of hospital admissions for older adults in the US occur due to ADRs related to NSAIDs.41 Further, NSAIDs are thought to be responsible for ten to 20 of every 1,000 hospitalizations.42 A recent survey of 1,572 Veterans Affairs Medical Center patients (mean age =61 years) reported that 32% used NSAIDs inappropriately, either because they used more than one NSAIDs, exceeded the maximum suggested daily dosage, or both. Reported ADRs for NSAIDs among the elderly include gastrointestinal bleeding, cardiovascular events, and renal toxicity.43–46 The risks are greater among older adults with reduced creatinine clearance, cardiovascular disease, or gastropathy. Moreover, a concomitant use of NSAIDs with low-dose aspirin use for cardioprotective purposes increases the possibility for gastrointestinal effects in the vulnerable elderly population.4 Therefore, it is often recommended that older persons taking a nonselective NSAID or COX-2 selective inhibitor with aspirin also obtain a prescription for a proton pump inhibitor, H2 receptor antagonist, or a similar appropriate medication to ensure gastroprotection.4 The inappropriate NSAIDs users reported significantly more gastrointestinal symptoms and more pain in the previous week compared to the appropriate NSAIDs users.47 While pain severity and length of treatment are not reported in NAMCS to fully determine the appropriate use of NSAIDs in older adults, it is imperative to further explore if appropriate guidelines are applied for pain management in these patients who are at higher risk of ADRs due to NSAIDs use.
Limitations
The NAMCS database is limited to up to six to eight drugs per patient visit. The cross-sectional nature of the NAMCS data limits us from knowing if prescriptions written were actually dispensed or filled by the patients, and for how long they were using these medications. Pain was defined as chronic or persistent, but level of severity is not reported in the NAMCS dataset.
Conclusion
A large percentage of older adults were prescribed NSAIDs for the management of persistent nonmalignant pain in US outpatient settings. While pain severity and length of treatment are not reported in NAMCS to fully determine appropriate use of NSAIDs in older adults, we report a consistent trend of NSAIDs use between 2000 and 2007, and that a large percentage of prescriptions were written by PCPs. Our data also report some use of adjuvant medications that are inappropriate for geriatric patients, which is also incongruent with AGS guidelines for persistent pain management. Future follow-up with actual prescription refill data is imperative to explore the extent of appropriate medication use according to AGS guidelines for persistent pain management in patients at high risk of ADRs. Lower percentages of NSAIDs prescriptions written by PCPs, particularly by geriatric specialists, is an encouraging indication that continuation of care by these physicians is important in appropriate persistent nonmalignant pain management in the vulnerable community-dwelling elderly population in the US.
Disclosure
Part of the findings were presented as a poster at the American Geriatric Society (AGS) Annual Meeting in Seattle, WA held in May 2012. The authors report no conflicts of interest in this work.
References
Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17(3):417–431, v. | |
Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies; 2011. Available from: http://books.nap.edu/openbook.php?record_id=13172&page=1. Accessed October 30, 2012. | |
Willman A, Petzäll K, östberg AL, Hall-Lord ML. The psycho-social dimension of pain and health-related quality of life in the oldest old. Scand J Caring Sci. 2013;27(3):534–540. | |
American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57(8):1331–1346. | |
Chou R, Huffman LH; American Pain Society; American College of Physicians. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):505–514. | |
Zhang W, Jones A, Doherty M. Does paracetamol (acetaminophen) reduce the pain of osteoarthritis? A meta-analysis of randomised controlled trials. Ann Rheum Dis. 2004;63(8):901–907. | |
Wegman A, van der Windt D, van Tulder M, Stalman W, de Vries T. Nonsteroidal antiinflammatory drugs or acetaminophen for osteoarthritis of the hip or knee? A systematic review of evidence and guidelines. J Rheumatol. 2004;31(2):344–354. | |
Wienecke T, Gøtzsche PC. Paracetamol versus nonsteroidal anti-inflammatory drugs for rheumatoid arthritis [review]. Cochrane Database Syst Rev. 2004;1:CD003789. | |
Lee C, Straus WL, Balshaw R, Barlas S, Vogel S, Schnitzer TJ. A comparison of the efficacy and safety of nonsteroidal antiinflammatory agents versus acetaminophen in the treatment of osteoarthritis: a meta-analysis. Arthritis Rheum. 2004;51(5):746–754. | |
Marcum ZA, Hanlon JT. Recognizing the risks of chronic nonsteroidal anti-inflammatory drug use in older adults. Ann Longterm Care. 2010; 18(9):24–27. | |
Rasu RS, Sohraby R, Cunningham L, Knell ME. Assessing chronic pain treatment practices and evaluating adherence to chronic pain clinical guidelines in outpatient practices in the United States. J Pain. 2013;14(6):568–578. | |
Paulose-Ram R, Hirsch R, Dillon C, Losonczy K, Cooper M, Ostchega Y. Prescription and non-prescription analgesic use among the US adult population: results from the third National Health and Nutrition Examination Survey (NHANES III). Pharmacoepidemiol Drug Saf. 2003;12(4):315–326. | |
Pitkala KH, Strandberg TE, Tilvis RS. Management of nonmalignant pain in home-dwelling older people: a population-based survey. J Am Geriatr Soc. 2002;50(11):1861–1865. | |
Lanas A, Garcia-Tell G, Armada B, Oteo-Alvaro A. Prescription patterns and appropriateness of NSAID therapy according to gastrointestinal risk and cardiovascular history in patients with diagnoses of osteoarthritis. BMC Med. 2011;9:38. | |
Assessment and Management of Chronic Pain. Guideline Summary [webpage on the Internet]. Bloomington: Institute for Clinical Systems Improvement; 2013. Available from: https://www.icsi.org/guidelines__more/catalog_guidelines_and_more/catalog_guidelines/catalog_neurological_guidelines/pain/. Accessed December 19, 2014. | |
ICD-9 and ICD9CM Codes Search [database on the Internet]. Bexhill-on-Sea, UK: MediLexicon International Ltd. Available from: http://www.medilexicon.com/icd9codes.php. Accessed December 19, 2014. | |
Anthony M, Lee KY, Bertram CT, et al. Gender and age differences in medications dispensed from a national chain drugstore. J Womens Health (Larchmt). 2008;17(5):735–743. | |
Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738–747. | |
Carbonin P, Pahor M, Bernabei R, Sgadari A. Is age an independent risk factor of adverse drug reactions in hospitalized medical patients? J Am Geriatr Soc. 1991;39(11):1093–1099. | |
Milton JC, Hill-Smith I, Jackson SH. Prescribing for older people. BMJ. 2008;336(7644):606–609. | |
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230–1239. | |
About the Ambulatory Health Care Surveys [webpage on the Internet]. Atlanta: Centers for Disease Controls and Prevention; 2009. Available from: http://www.cdc.gov/nchs/ahcd/about_ahcd.htm. Accessed November 27, 2012. | |
Gu Q, Dillon CF, Burt VL. Prescription drug use continues to increase: US prescription drug data for 2007–2008. NCHS Data Brief. 2010;(42):1–8. | |
Raofi S, Schappert SM. Medication therapy in ambulatory medical care: United States, 2003–2004. Vital Health Stat 13. 2006;(163):1–40. | |
Solomon DH, Glynn RJ, Bohn R, Levin R, Avorn J. The hidden cost of nonselective nonsteroidal antiinflammatory drugs in older patients. J Rheumatol. 2003;30(4):792–798. | |
Ray WA, Stein CM, Byrd V, et al. Educational program for physicians to reduce use of non-steroidal anti-inflammatory drugs among community-dwelling elderly persons: a randomized controlled trial. Med Care. 2001;39(5):425–435. | |
US Department of Health and Human Services. Administration on Aging, A Profile of Older Americans. Washington, DC: Administration for Community Living; 2010. | |
National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: United States Department of Health and Human Services; 2012. Available from: http://www.cdc.gov/nchs/data/hus/hus11.pdf. Accessed November 6, 2014. | |
Correa-de-Araujo R, Miller GE, Banthin JS, Trinh Y. Gender differences in drug use and expenditures in a privately insured population of older adults. J Womens Health (Larchmt). 2005;14(1):73–81. | |
Wyles H, Rehman HU. Inappropriate polypharmacy in the elderly. Eur J Intern Med. 2005;16(5):311–313. | |
Cooper JW. Probable adverse drug reactions in a rural geriatric nursing home population: a four-year study. J Am Geriatr Soc. 1996;44(2):194–197. | |
Kaufman G. Polypharmacy in older adults. Nurs Stand. 2011;25(38):49–55; quiz 58. | |
Bowie MW, Slattum PW. Pharmacodynamics in older adults: a review. Am J Geriatr Pharmacother. 2007;5(3):263–303. | |
Won AB, Lapane KL, Vallow S, Schein J, Morris JN, Lipsitz LA. Persistent nonmalignant pain and analgesic prescribing patterns in elderly nursing home residents. J Am Geriatr Soc. 2004;52(6):867–874. | |
Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35(2):214–228. | |
O’Neil CK, Hanlon JT, Marcum ZA. Adverse effects of analgesics commonly used by older adults with osteoarthritis: focus on non-opioid and opioid analgesics. Am J Geriatr Pharmacother. 2012;10(6):331–342. | |
Pergolizzi J, Böger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008;8(4):287–313. | |
American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–631. | |
Crandall RC. Gerontology: A Behavioral Science Approach. 2nd ed. New York: McGraw-Hill; 1991. | |
Brvar M, Fokter N, Bunc M, Mozina M. The frequency of adverse drug reaction related admissions according to method of detection, admission urgency and medical department specialty. BMC Clin Pharmacol. 2009;9:8. | |
Herndon CM, Hutchison RW, Berdine HJ, et al; Ambulatory Care, Cardiology, and Pain and Palliative Care Practice and Research Networks of the American College of Clinical Pharmacy. Management of chronic nonmalignant pain with nonsteroidal antiinflammatory drugs. Joint opinion statement of the Ambulatory Care, Cardiology, and Pain and Palliative Care Practice and Research Networks of the American College of Clinical Pharmacy. Pharmacotherapy. 2008;28(6):788–805. | |
Bhatt DL, Scheiman J, Abraham NS, et al; American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2008;118(18):1894–1909. | |
Mamdani M, Juurlink DN, Lee DS, et al. Cyclo-oxygenase-2 inhibitors versus non-selective non-steroidal anti-inflammatory drugs and congestive heart failure outcomes in elderly patients: a population-based cohort study. Lancet. 2004;363(9423):1751–1756. | |
Niccoli L, Bellino S, Cantini F. Renal tolerability of three commonly employed non-steroidal anti-inflammatory drugs in elderly patients with osteoarthritis. Clin Exp Rheumatol. 2002;20(2):201–207. | |
Rahme E, Nedjar H. Risks and benefits of COX-2 inhibitors vs non-selective NSAIDs: does their cardiovascular risk exceed their gastrointestinal benefit? A retrospective cohort study. Rheumatology (Oxford). 2007;46(3):435–438. | |
Varas-Lorenzo C, Riera-Guardia N, Calingaert B, et al. Stroke risk and NSAIDs: a systematic review of observational studies. Pharmacoepidemiol Drug Saf. 2011;20(12):1225–1236. | |
Kovac SH, Houston TK, Weinberger M. Inappropriate nonsteroidal anti-inflammatory drug use: prevalence and predictors. J Patient Saf. 2010;6(2):86–90. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


