Back to Journals » Clinical Interventions in Aging » Volume 11
Periprocedural temporary pacing in primary percutaneous coronary intervention for patients with acute inferior myocardial infarction
Authors Hwang Y , Kim C, Moon K
Received 2 November 2015
Accepted for publication 9 December 2015
Published 10 March 2016 Volume 2016:11 Pages 287—292
DOI https://doi.org/10.2147/CIA.S99698
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
You Mi Hwang,1 Chul-Min Kim,2 Keon-Woong Moon2
1Department of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, 2Department of Internal Medicine, St Vincent’s Hospital, The Catholic University of Korea, Suwon, South Korea
Objective: High-degree atrioventricular block (AVB), including complete AVB in acute inferior ST-elevation myocardial infarction (STEMI), is not uncommon. However, there is no study evaluating the clinical differences between patients who have undergone temporary pacing (TP) and patients who have not. The present study was designed to investigate whether TP has any prognostic significance in inferior STEMI complicated by complete AVB.
Methods: From January 2009 to December 2014, 295 consecutive patients diagnosed with inferior wall STEMI in a university hospital were reviewed. All of them underwent primary percutaneous coronary intervention (PCI). Among the 295 patients, there were 72 patients with complete AVB. The clinical characteristics, procedural data, and long-term major adverse cardiocerebrovascular events were compared in patients with and without TP.
Results: Baseline clinical and procedural characteristics were similar between patients with and without TP. Patients with TP were more likely to present with cardiogenic shock; thus, additional interventions were attempted via a femoral approach, as patients received further treatment with intra-aortic balloon pumps and were subjected to additional cardiopulmonary resuscitation. Most cases of complete AVB were primarily caused by right coronary artery occlusion. After a median follow-up period of 344 (range, 105.5–641) days, major adverse cardiocerebrovascular events did not differ between the groups (P=0.528).
Conclusion: We conclude that primary PCI without TP is acceptable in complete AVB-complicated acute inferior STEMI. To avoid delay in reperfusion, we suggest that primary PCI should be the first priority therapy rather than treating patients initially with TP.
Keywords: myocardial infarction, complete atrioventricular block, primary percutaneous coronary intervention, temporary pacemaker
Introduction
Any degree of atrioventricular block (AVB) is a common complication of acute myocardial infarction (AMI).1–5 High-degree atrioventricular block (HAVB) is seen in ~2% to 13% of all AMI cases.6–8 Especially, in patients with ST-elevation myocardial infarction (STEMI), the occurrence of HAVB has been reported to be even higher than that in non-STEMI patients.9–11 In particular, patients suffering from inferior STEMI tend to present with cardiogenic shock and bradyarrhythmia. In the thrombolytic era, HAVB in acute inferior myocardial infarction (MI) has been associated with older age, larger infarct size, female predominance, and higher mortality.12–15 The mortality rate has been significantly improved as primary percutaneous coronary intervention (PCI) has replaced thrombolysis in the treatment of STEMI. However, in previous reports, the presence of HAVB was a significant prognostic factor for survival.16,17 Although there is a definite recommendation for treatment with primary PCI in these patients, no accepted guidelines exist for managing HAVB; however, patients were frequently treated with temporary right ventricular (RV) pacing (TP) in this clinical setting, at the clinician’s discretion.18 The clinical significance of HAVB in a highly select group of patients suffering from inferior wall STEMI has not yet been studied. In addition, a study by Ho et al19 indicated that TP failed to improve mortality in anterior MI, but no other studies examined inferior wall STEMI. Therefore, the objective of this study was to investigate the incidence, predictors, and prognostic significance of HAVB in inferior STEMI. Furthermore, we investigated whether performing TP in patients with HAVB-complicated inferior wall STEMI improved the clinical outcome.
Methods
Patients
Among 295 patients who were diagnosed with STEMI involving the inferior wall from January 2009 to December 2014, we reviewed 72 patients with HAVB. Inferior wall STEMI was defined as typical chest pain or dyspnea lasting for >30 minutes, ST-segment elevation ≥1.0 mm in more than two of the three inferior leads (II, III, and aVF), and elevated serum creatinine phosphokinase or troponin-T levels more than twice the upper limits of normal. HAVB was defined as a high-degree AVB, greater than a Mobitz type 2 AVB, including a complete AVB. A temporary RV pacemaker was implanted if there was hemodynamic instability and bradycardia with a heart rate of <40 bpm refractory to intravenous administration of atropine or saline. Cardiogenic shock was defined as systolic blood pressure <80 mmHg in spite of adequate fluid administration with or without bradycardia. All patients received successful primary PCI. TP was done via femoral vein approach, and RV lead was placed at the RV apex and the pacing rate was set at 50–80 bpm, at the physician’s discretion. The clinical characteristics, laboratory data, angiographic findings, PCI procedural data, and inhospital and long-term clinical outcomes were compared between patients receiving TP and patients not receiving TP. MACEs (major adverse cardiocerebrovascular events) were defined as any cardiocerebrovascular events, such as any death from cardiocerebrovascular events, MI, and target vessel revascularization. Echocardiographic measurements of left ventricular ejection fraction were performed 1 day or 2 days after PCI. The study protocol was approved by the Institutional Review Board of St Vincent’s Hospital (Suwon, South Korea; IRB No VC15RASI0034). All patients were retrospectively enrolled. However, informed written consent for the procedure was obtained from the patients.
Statistical analysis
Analyses were performed using R 3.1.1 statistical software (R Development Core Team, 2014). Categorical variables were described using frequencies, while continuous variables were reported as median and interquartile ranges. Fisher’s exact test or Pearson’s χ2-test with Yates’ continuity correction was used to compare categorical variables between patients with HAVB and those without HAVB and patients receiving TP and those not receiving TP. A two-sided t-test was used to compare continuous variables. The survival of patients with and without HAVB was determined using the Kaplan–Meier method and compared using a log-rank test.
Results
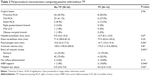
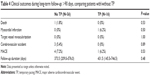
The baseline characteristics of 72 patients are summarized in Table 1. Among 72 HAVB patients, 16 (22.2%) were implanted with a temporary pacemaker. There were no significant differences in sex, age, basal metabolic index, lipid profiles, peak cardiac markers, inflammatory status, or prevalence of underlying medical conditions between TP and non-TP groups. However, there were statistical differences in serum creatinine level and smoking status. Never smoker and ex-smoker with HAVB tended to be more prevalent in the TP group (39.3% vs 75%, P=0.041). Clinical presentation at emergency room and periprocedural data are summarized in Tables 2 and 3, respectively. Basal rhythm, heart rate, bundle branch block, and left ventricular systolic function at emergency room at presentation were not different between the two groups. However, among the 25 patients presented with cardiogenic shock, 12 patients underwent TP, which seemed to be a major factor to decide TP (P<0.001). In our study population, most of the HAVBs were caused by right coronary artery infarction (97.2%). Door-to-balloon time and needle-to-balloon time were similar between the two groups. However, more patients with TP underwent primary PCI via femoral access (25% vs 75%, P=0.001), had intra-aortic balloon pump support (1.8% vs 18.8%, P=0.046), and had longer radiation exposure time (10 minutes vs 14.7 minutes, P=0.044) than those in the non-TP group. TP group patients also stayed longer in the hospital than the non-TP group (5 days vs 6 days, P=0.03). HAVB was reversed in all patients after primary PCI, and in TP, pacing lead was removed mostly in the cardiac catheterization laboratory soon after reperfusion.
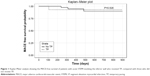
After a median of 344 (range, 105.5–641) days of follow-up, the mortality rate (P=0.89) and MACEs (P=0.53) were not significantly different between the two groups. Especially, there was no short-term (<90 days) mortality event in both groups. During the long-term follow-up period, five MACEs occurred in four patients: four MACEs in the non-TP group (three patients had cerebrovascular accident and one patient died) and one MACE in the TP group (Table 4). Finally, Kaplan–Meier analysis showed a comparable prognosis based on the mortality events between patients with and without TP in acute inferior wall STEMI (P=0.53; Figure 1).
Discussion
HAVB is a common complication of AMI. In particular, patients with inferior AMI are more prone to developing HAVB compared with patients with anterior AMI.16 By extension, STEMI increases the risk of HAVB compared with patients with non-STEMI. The mechanism of HAVB in inferior wall STEMI is not fully elucidated. However, as mentioned in our previous study,20 we consider that the underlying major cause of bradyarrhythmia results from the cardioinhibitory (Bezold–Jarisch) reflexes arising from vagal efferent nerves in the ischemic ventricular wall. In this study, we investigated the prognostic significance of TP in 72 patients with inferior STEMI treated with primary PCI. There are some studies demonstrating poor clinical outcomes in HAVB, such as in cases of cardiogenic shock, atrioventricular arrhythmias, and short-term (<30 days) mortality rate.3,15,17,21 In our study patients with a manifested cardiogenic shock, more TP was performed; in addition, femoral access was more frequent in the TP group, which was estimated as interrelated. However, in our study, all the patients, even those with HAVB, recovered from complete AVB with low short- and long-term mortality rate. The result is contrary to previous reports that HAVB-complicated inferior STEMI was associated with poor cardiovascular outcomes.3,4,11,14,22,23
Our study has several limitations. First, it was conducted with a relatively small number of patients, resulting in an insufficient power to postulate generalizations. However, this study was designed to determine the effect of TP in patients with HAVB-complicated inferior wall STEMI on a relatively large scale at a local center. Even though the numbers were small, the study group was reduced to a particular group of inferior STEMI that underwent successful primary PCI. Second, the follow-up period was too short to generalize any long-term outcomes, although it contained a wide variation in the follow-up duration (0–1,071 days). Third, to evaluate the effect of TP, we should have distributed patients evenly in the TP and non-TP groups. However, the decision to select the distribution of the patients was at the clinician’s discretion, and there were also related ethical issues to consider for patient distribution in the study.
However, our study also has several strengths. First, it was conducted using a discrete population of inferior STEMI patients from one center during a 6-year period with consistent criteria for HAVB. Although primary PCI is usually recommended for all STEMI patients in present-day practice, there have been no other studies conducted specifically on inferior STEMI with HAVB to define the prognostic implication of TP in such a clinical setting. Moreover, in our study, all patients received primary PCI. After primary PCI, HAVB was reversed in all patients, indicating that TP is unnecessary in inferior STEMI treated successfully with primary PCI. In our hospital, a temporary pacemaker was implanted if there was hemodynamic instability and bradycardia with a heart rate ≤40 bpm refractory to intravenous atropine administration with fluids. With experience, we recently performed primary PCI without TP in STEMI patients with HAVB. Most of the patients were stable and HAVB could be reversed with primary PCI.
Conclusion
Primary PCI solely can ameliorate HAVB-complicated inferior STEMI without using a time-consuming and cumbersome TP procedure. Thus, we recommend primary reperfusion therapy with PCI as the first-line therapy in most patients with HAVB-complicated acute inferior MI, because early reperfusion therapy solely reverses HAVB without the need of TP. However, we should consider applying all the possible measures to maintain the hemodynamic stability of patients, if symptomatic or hemodynamic unstable bradycardia persists even after successful reperfusion.
Although our study has several limitations, these results may help in decision-making for clinicians and further contribute some part in future guidelines dealing with patients suffering from HAVB-complicated inferior STEMI.
Acknowledgment
We acknowledge the helpful support of all authors.
Disclosure
The authors report no conflicts of interest in this work.
References
Goldstein JA, Lee DT, Pica MC, Dixon SR, O’Neill WW. Patterns of coronary compromise leading to bradyarrhythmias and hypotension in inferior myocardial infarction. Coron Artery Dis. 2005;16(5):265–274. | ||
Harpaz D, Behar S, Gottlieb S, Boyko V, Kishon Y, Eldar M. Complete atrioventricular block complicating acute myocardial infarction in the thrombolytic era. SPRINT Study Group and the Israeli Thrombolytic Survey Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. J Am Coll Cardiol. 1999;34(6):1721–1728. | ||
Aplin M, Engstrom T, Vejlstrup NG, et al; TRACE Study Group. Prognostic importance of complete atrioventricular block complicating acute myocardial infarction. Am J Cardiol. 2003;92(7):853–856. | ||
Berger PB, Ruocco NA Jr, Ryan TJ, Frederick MM, Jacobs AK, Faxon DP. Incidence and prognostic implications of heart block complicating inferior myocardial infarction treated with thrombolytic therapy: results from TIMI II. J Am Coll Cardiol. 1992;20(3):533–540. | ||
Meine TJ, Al-Khatib SM, Alexander JH, et al. Incidence, predictors, and outcomes of high-degree atrioventricular block complicating acute myocardial infarction treated with thrombolytic therapy. Am Heart J. 2005;149(4):670–674. | ||
Giglioli C, Margheri M, Valente S, et al. Timing, setting and incidence of cardiovascular complications in patients with acute myocardial infarction submitted to primary percutaneous coronary intervention. Can J Cardiol. 2006;22(12):1047–1052. | ||
Grines CL, Browne KF, Marco J, et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993;328(10):673–679. | ||
Rathore SS, Gersh BJ, Berger PB, et al. Acute myocardial infarction complicated by heart block in the elderly: prevalence and outcomes. Am Heart J. 2001;141(1):47–54. | ||
Nguyen HL, Lessard D, Spencer FA, et al. Thirty-year trends (1975–2005) in the magnitude and hospital death rates associated with complete heart block in patients with acute myocardial infarction: a population-based perspective. Am Heart J. 2008;156(2):227–233. | ||
Spencer FA, Jabbour S, Lessard D, et al. Two-decade-long trends (1975–1997) in the incidence, hospitalization, and long-term death rates associated with complete heart block complicating acute myocardial infarction: a community-wide perspective. Am Heart J. 2003;145(3): 500–507. | ||
Goldberg RJ, Zevallos JC, Yarzebski J, et al. Prognosis of acute myocardial infarction complicated by complete heart block (the Worcester Heart Attack Study). Am J Cardiol. 1992;69(14):1135–1141. | ||
Birnbaum Y, Sclarovsky S, Herz I, et al. Admission clinical and electrocardiographic characteristics predicting in-hospital development of high-degree atrioventricular block in inferior wall acute myocardial infarction. Am J Cardiol. 1997;80(9):1134–1138. | ||
Gang UJ, Hvelplund A, Pedersen S, et al. High-degree atrioventricular block complicating ST-segment elevation myocardial infarction in the era of primary percutaneous coronary intervention. Europace. 2012;14(11):1639–1645. | ||
Behar S, Zissman E, Zion M, et al. Complete atrioventricular block complicating inferior acute wall myocardial infarction: short- and long-term prognosis. Am Heart J. 1993;125(6):1622–1627. | ||
Jim MH, Chan AO, Tse HF, Lau CP. Predictors of inhospital outcome after acute inferior wall myocardial infarction. Singapore Med J. 2009;50(10):956–961. | ||
Pirzada AM, Zaman KS, Mahmood K, Sagheer T, Mahar SA, Jafri MH. High degree atrioventricular block in patients with acute inferior myocardial infarction with and without right ventricular involvement. J Coll Physicians Surg Pak. 2009;19(5):269–274. | ||
Gomez-Talavera S, Vivas D, Perez-Vizcayno MJ, et al. Prognostic implications of atrio-ventricular block in patients undergoing primary coronary angioplasty in the stent era. Acute Card Care. 2014;16(1):1–8. | ||
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127(4):e362–e425. | ||
Ho KW, Koh TH, Wong P, et al. Complete atrioventricular block complicating acute anterior myocardial infarction can be reversed with acute coronary angioplasty. Ann Acad Med Singapore. 2010;39(3):254–257. | ||
Lee SN, Hwang YM, Kim GH, et al. Primary percutaneous coronary intervention ameliorates complete atrioventricular block complicating acute inferior myocardial infarction. Clin Interv Aging. 2014;9: 2027–2031. | ||
Jim MH, Chan AO, Tse HF, Barold SS, Lau CP. Clinical and angiographic findings of complete atrioventricular block in acute inferior myocardial infarction. Ann Acad Med Singapore. 2010;39(3):185–190. | ||
Berger PB, Ryan TJ. Inferior myocardial infarction. High-risk subgroups. Circulation. 1990;81(2):401–411. | ||
Nicod P, Gilpin E, Dittrich H, Polikar R, Henning H, Ross J Jr. Long-term outcome in patients with inferior myocardial infarction and complete atrioventricular block. J Am Coll Cardiol. 1988;12(3):589–594. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.