Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
Periodontal ligament injection versus routine local infiltration for nonsurgical single posterior maxillary permanent tooth extraction: comparative double-blinded randomized clinical study
Authors Al-Shayyab MH
Received 3 June 2017
Accepted for publication 8 September 2017
Published 6 October 2017 Volume 2017:13 Pages 1323—1331
DOI https://doi.org/10.2147/TCRM.S143173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Mohammad H Al-Shayyab
Department of Oral and Maxillofacial Surgery, Oral Medicine and Periodontology, School of Dentistry, University of Jordan, Amman, Jordan
Aim: The aim of this study was to evaluate the efficacy of, and patients’ subjective responses to, periodontal ligament (PDL) anesthetic injection compared to traditional local-anesthetic infiltration injection for the nonsurgical extraction of one posterior maxillary permanent tooth.
Materials and methods: All patients scheduled for nonsurgical symmetrical maxillary posterior permanent tooth extraction in the Department of Oral and Maxillofacial Surgery at the University of Jordan Hospital, Amman, Jordan over a 7-month period were invited to participate in this prospective randomized double-blinded split-mouth study. Every patient received the recommended volume of 2% lidocaine with 1:100,000 epinephrine for PDL injection on the experimental side and for local infiltration on the control side. A visual analog scale (VAS) and verbal rating scale (VRS) were used to describe pain felt during injection and extraction, respectively. Statistical significance was based on probability values <0.05 and measured using Χ2 and Student t-tests and nonparametric Mann–Whitney and Kruskal–Wallis tests.
Results: Of the 73 patients eligible for this study, 55 met the inclusion criteria: 32 males and 23 females, with a mean age of 34.87±14.93 years. Differences in VAS scores and VRS data between the two techniques were statistically significant (P<0.001) and in favor of the infiltration injection.
Conclusion: The PDL injection may not be the alternative anesthetic technique of choice to routine local infiltration for the nonsurgical extraction of one posterior maxillary permanent tooth.
Keywords: PDL injection, infiltration, anesthesia, extraction
A Letter to the Editor has been received and published for this article.
Introduction
Local anesthesia (LA) is the most commonly used treatment modality for pain control during medical and dental procedures.1 However, the LA injection itself has been reported as the only perceived painful part of dental procedures, and the associated fear of this injection is often considered a factor in avoiding dental treatment.2 Numerous studies have investigated factors determining fear, as well as success and effectiveness of LA injections, including tissue distensibility,1 speed of injection,3 solution temperature,4 and patient characteristics.5 In addition, the type of technique has been reported to have an important role in determining pain perceived at the time of injection or extraction.6
Local infiltration is commonly regarded as the technique of choice for confined maxillary anesthesia, because it is an easier technique to perform, not affected by collateral innervations, and allows rapid and easy diffusion of the LA solution through the relatively porous maxillary bone and its thin bony cortex.1,7 However, local infiltration techniques show great variation in success rates8,9 and pain scores during administration of anesthetic injections for maxillary teeth.6 This variation has been explained by anatomical deviations in the bone surrounding maxillary teeth and individual variations in response to the anesthetic agent administered.10 As such, the periodontal ligament (PDL) injection was suggested as a possible alternative to minimize pain scores during injection of LA for maxillary teeth procedures.6,11 The PDL anesthetic-injection technique was first described in 1924 and popularized in the 1970s, when special dental syringes were dedicated to this technique.12 It entails the deposit of LA solution into the coronal part of PDL and then the solution reaches the alveolar bone through fenestrations found in the alveolar socket.13 The PDL anesthetic-injection technique is often employed as a supplemental injection for unsuccessful conventional techniques, particularly inferior alveolar nerve block for mandibular anesthesia.14 However, it is also the preferred primary technique when anesthesia of short duration is desired and a safer alternative when limited soft-tissue anesthesia for simple single-tooth extraction is required15 or for patients with bleeding tendencies.16 This technique shows variable success rates according to the indication for treatment,17 rapid onset of action, 30–45 minutes’ duration of anesthesia,18 and rare systemic toxicity.15,19
The literature concerning the success and pain scores of the PDL injection technique compared with other techniques remains controversial: whereas some studies20,21 have found no significant difference in pain scores between local infiltration and PDL injection, other older studies found that pain during administration of PDL injection was described by the majority of patients as either greater than local infiltration6 or as a less painful injection compared with other injection techniques.22,23 The results of the most recent studies11,24–26 showed that PDL anesthesia is an effective anesthetic technique for localized anesthesia in the mandible. With new devices like the computer-controlled LA-delivery system (CCLADS), the PDL injection has been reported as a convenient primary anesthetic technique of LA for both patient and dentist,24 and as effective as local infiltration when used during conservative treatment of primary mandibular posterior teeth;25,27 however, local infiltration has been more effective than PDL when used during extraction procedures.27 Compared with conventional local infiltration anesthesia, PDL anesthesia with CCLADS reduces injection pain while achieving a satisfactory anesthetic effect.27 The first meta-analysis comparing the effectiveness of anesthesia and pain during injection between inferior alveolar nerve block and PDL concluded that PDL was neither superior nor inferior.28 However, to the author’s best knowledge, no published English literature has compared conventional primary PDL injection and local infiltration for single maxillary permanent tooth anesthesia and extraction.
The aim of this study was to evaluate the efficacy of and patients’ subjective responses to the PDL injection technique compared to the traditional infiltration injection for the nonsurgical extraction of one posterior maxillary permanent tooth. In the present study, the null hypothesis was that the PDL injection would be associated with similar pain scores during injection and extraction compared to routine local infiltration for the nonsurgical extraction of one posterior maxillary permanent tooth. Therefore, PDL injection would be the alternative technique of choice to routine local infiltration for nonsurgical extraction of one posterior maxillary permanent tooth.
Materials and methods
This was a prospective randomized double-blinded split-mouth study approved by the research ethics committee at the University of Jordan (10/2015/15791), and registered in a public trials registry (ClinicalTrials.gov, NCT03173898). It was conducted according to the principles of the Helsinki Declaration from July 6, 2015 to January 31, 2016. All patients scheduled for nonsurgical symmetrical maxillary posterior permanent tooth extraction in the Department of Oral and Maxillofacial Surgery at the University of Jordan Hospital, Amman, Jordan were invited to participate in this study. Written informed consent was then obtained from the patient or legal guardian for patients under 18 years of age.
Inclusion criteria were patients who were fit for surgery under LA (classified by the American Society of Anesthesiologists [ASA] as ASA I–III), patients exhibiting full understanding of given oral instructions, and bilateral symmetrical posterior maxillary permanent teeth referred for nonsurgical extractions under LA. Exclusion criteria were presence of acute dentoalveolar infection, patients requiring conscious sedation or general anesthesia, patients unwilling to participate in the study, patients with ASA >III; patients on anti-inflammatory or recreational drugs, and patients requiring more than two additional injections in one or both sides for incomplete anesthesia.
Patients were instructed and guided by a blinded clinician on two self-reported scales used for assessment of pain in clinical trials: the visual analog scale (VAS) and the verbal rating scale (VRS).29–31 The VAS is composed of a 100 mm line, and allows the patient to score the pain experienced during injection and extraction: 0 represents “no pain” at the rightmost point, and 100 represents the “worst pain” at leftmost point. The VRS allows the patient to describe pain during extraction as less than expected, as expected, or greater than expected, and to describe the extraction as acceptable or unacceptable.
The recommendations of Malamed1 and other investigators7,17 concerning anesthetic procedures and volumes for posterior maxillary permanent tooth extraction were followed. For each technique, a standard dental syringe (KLS Martin, Tuttlingen, Germany), 27-gauge short dental needles (0.4×21 mm; CK Dental, Orange, CA, USA), and the recommended volume of 2% lidocaine with epinephrine 1:100,000 (Lignospan standard; Septodont, Paris, France) in a cartridge-ampoule syringe at room temperature were used. The method of anesthesia used for the left or right sides was blinded to the patient and performed randomly by the same surgeon (MA), who was not involved in the extraction. This systematic random allocation was created by an independent resident who was not directly involved with the study. All patients received on one side (experimental side) a primary PDL injection, and on the other side (control side) a primary infiltration injection started by buccal injection and then followed by palatal injection. Markings labeled on the cartridge were enhanced to administer the recommended volume for each injection accurately. Accordingly, on one side, 1.8 mL of the anesthetic solution for the buccal injection and 0.3 mL for the palatal injection were given adjacently to the tooth of interest at a slow rate over approximately 1 minute. On the other side, the PDL injection was carried out after expressing half of the contents of the cartridge using the standard dental syringe, aiming to administer 0.2 mL of solution over 30 seconds on the mesial aspect of each root of the tooth. However, the needle was repositioned and the injection repeated when no backward pressure was felt during injection. A latency period of 5 minutes was then given to allow the anesthetic to take effect, during which patients were asked to complete the VAS by themselves to evaluate the degree of pain experienced on each anesthetic injection. Following the 5-minute latency period, the extraction procedure was randomly (created by an independent resident who was not directly involved with the study) commenced using the same set of instruments (elevators or forceps) and techniques for such extractions by the same resident who was blinded to the anesthetic technique administered randomly by the surgeon. If the patient experienced unacceptable pain during extraction, one additional PDL injection on the experimental side or buccal infiltration injection on the control side was given by the surgeon who was familiar with the technique employed on each side and then waiting 5 minutes. If the pain was still unacceptable, a second additional PDL injection on the experimental side or palatal injection on the control side was also administered, and the whole step was recorded. These additional injections were administered using a protocol identical to the primary injections. Teeth needing surgical extraction were excluded from the study. Lastly, after completion of extractions, patients were invited to complete the VAS and VRS by themselves to evaluate the degree of pain during extraction.
Power analysis
For this study, power was calculated using the statistical software package G*Power version 3.1.5. Post hoc power analysis was computed given α-values, sample size, and effect size. A t-test of independent means (two groups) was set as the statistical test to perform power analysis using α=0.05, sample size of 55 subjects valid for analysis, and medium effect size of 0.5. Analysis yielded 83.2% power.
Statistical analyses
Statistical analyses were performed using SPSS 19.0 (SPSS, Chicago, IL, USA). VAS values and VRS data for both sides were assessed using Student’s t-test and χ2 test, respectively. Comparison of VAS values within and among individual groups of indications for tooth extraction and extracted teeth was achieved using the nonparametric Mann–Whitney and Kruskal–Wallis tests, respectively. A probability value less than 0.05 was considered statistically significant.
Results
Of the 73 patients eligible for this study, 18 were excluded: seven had an acute dentoalveolar infection, six required surgical extraction for complete removal of a tooth, and five were on anti-inflammatory drugs. The final cohort comprised a total of 55 patients: 32 males and 23 females, with mean age of 34.87±14.93 (range 13–65) years. As such, a total of 110 maxillary posterior permanent teeth were extracted: 38 heavily carious (unrestorable), 33 periodontally compromised, 15 badly destructed crown structures (unrestorable), 14 with periapical lesions and deemed unsuitable for root-canal treatment, and ten for orthodontic reasons. Of the extracted teeth, 22 were first premolars, 30 second premolars, 32 first molars, and 36 second molars.
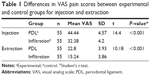
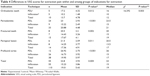
The mean VAS pain score (for injection and extraction) in the PDL group was significantly (P<0.001) higher than in the infiltration group (Table 1). Differences in the VRS data (for extraction) and the need for additional injections were statistically significant (P<0.05, Table 2). In the PDL group (experimental), none of the patients described extraction pain as “less than expected”; rather, it was described as “expected” by 33 (60%) patients and “greater than expected” by 22 (40%) patients, and evaluated overall as “acceptable” by only 20 (36.4%) patients. In the infiltration group (control), extraction pain was described as “less than expected” by eight (14.5%) patients, “expected” by 36 (65.5%) patients, and “greater than expected” by eleven (20%) patients, and evaluated overall as “acceptable” by the majority (80%) of patients. In addition, 16 (29.1%) patients needed additional PDL injections compared to six (10.9%) patients needing additional infiltration injections. However, none of the patients required more than two additional injections. The majority (90.1%) of patients preferred the infiltration technique.
Indications for extraction and their influence on VAS pain scores for injection and extraction are detailed in Tables 3 and 4, respectively. Within each group of indications, Mann–Whitney tests showed statistically significant (P<0.05) differences between the two injection techniques. However, when ignoring injection technique, Kruskal–Wallis tests showed that VAS differences among groups of indications were statistically significant (P<0.05) for extraction pain only. For median VAS score, indications were ordered: orthodontic teeth < periapical lesion = profound caries < fractured teeth < periodontitis. However, Mann–Whitney tests revealed that this significance was between two pairs of indications only: orthodontic teeth and teeth with periodontitis and profound caries (P<0.005). Differences for the remaining eight pairs were not statistically significant (P>0.005).
With regard to the influence of extracted teeth on VAS pain scores, the injection and extraction of the second premolar recorded the lowest pain scores compared with other extracted teeth: first premolar (injection 39.45±8.61, extraction 19.36±5.60), second premolar (injection 36.67±7.13, extraction 17.63±5.61), first molar (injection 37.97±7.12, extraction 20.25±4.85), second molar (injection 40.08±7.16, extraction 18.81±5.67). However, Kruskal–Wallis tests showed that these VAS differences (for injection and extraction) among groups of extracted teeth were not statistically significant (P>0.05). For type of injection technique within each group of extracted teeth, Mann–Whitney tests showed that PDL injection resulted in statistically significant (P<0.01) higher pain scores for injection and extraction compared with local infiltration.
Discussion
Pain is a dynamic process that begins with injury or disease producing neural signals, and is influenced by psychological variables, such as past experience, attention, culture, anxiety, and depression.29,32 Self-reported VAS and VRS scores were used to measure pain scores in previous clinical trials.30,31 These self-reported scales have shown validity and reliability and are easy to use, placing minimal demands on almost all patients.33 For pain measurement, indices of validity and consistency of these scales can be used to rank them hierarchically.34 A number of strengths and weaknesses of the VAS and VRS have been reported. The VAS is considered to have more sensitivity and validity than the VRS, possibly due to the higher number of response categories.32 Additionally, The VRS allows for data that can be more simply ranked, as it provides a consequent fixed number of response categories to express pain experience, with no ability of the intervals between each category to be compartmentalized to be equal. Therefore, the VRS is considered less sensitive than the VAS.32 By contrast, patients with difficulties in equating pain with the length of a line, such as the elderly, have difficulty with the VAS compared with the VRS; therefore, the VAS could be less sensitive than the VRS.32,35 In this study, the VAS was selected to measure pain during injection and extraction due to its high reliability and validity in the unidimensional measurement of pain, which is expected to be provided by the increased number of categories allocated for patients’ responses.32 However, the VRS was selected to measure the overall satisfaction of patients during extraction only; although it limits statistical analysis to nonparametric tests,32 it is simple, especially for elderly patients, so that promotes compliance.33
The number of subjects included in this equivalence study was greater than previous studies with similar design and methodology,19,27 and analysis computation yielded 83.2% power. This power was considered to be adequate for such clinical study matching and controlling the study sample over a 7-month period. In this study, some precautions were implemented by the author to avoid the possible influence of the extraneous variables on reliability and validity of the results. Therefore, only subjects who were scheduled for symmetrical extraction by one surgeon (MA), not all surgeons in our maxillofacial surgery unit, over the 7-month period were studied. Although it was a split-mouth (crossover) study and there could have been a residual effect from the first injection or extraction on the second, a washout period (a few seconds usually given to start the second injection or extraction) would avoid the possibility of this residual effect. The author also adopted systematic randomization of injection and extraction side to avoid the possible influence of their order on patients’ responses. This systematic random allocation would determine the sequence of injections and extractions for each study subject alternately and provide the same chance of treatment sequence for all subjects. Furthermore, previous split-mouth studies30,36 reported that the order of LA technique and extraction did not influence the pain felt during injection and extraction. Additionally, the double-blind design of this trial was followed to ensure that there were no differences in the way the study injections and extractions were assessed or managed, thus minimizing bias. This was achieved by ensuring that both injection techniques and extraction procedures appeared the same. Additionally, neither the clinicians nor the study subjects were aware of the anesthetic technique assigned on each side. These are strategies aimed at reducing the threats to validity, and sometimes used in terms of control, which are used to avoid the possible influence of situational and interoperator variability on study outcome.37 Furthermore, since acute dentoalveolar infection or surgical (not simple) extraction or anti-inflammatory drugs are known to influence the effectiveness of LA and patients’ responses to LA and extraction,1 18 subjects (24.7%) with such factors were excluded. Such a methodological approach consistently leads to a homogeneous sample of blocked characteristics, and may have been necessary in this study, with its small cohort. A standard conventional dental syringe was used in the present study, not a special PDL syringe, since the former is readily available in the clinic and proves equally successful when a standard 27-gauge short needle was used.1,17,38 To avoid the drawbacks of using conventional syringes for PDL injection, the author expressed half the cartridge’s contents prior to injection to reduce the exerted pressure and the likelihood of breakage.1 Malamed17 reported no cartridge breakage during PDL injection using conventional syringes. This would also make the results of this study more applicable: no need to buy the highly expensive new syringes and disposable attachments or to change work routines.20 In addition, 2% lidocaine was used in the present study, as it is a widely used anesthetic39 and considered a reference for any new LA.1,7 These are all considered key strengths of the design of this study.
In this double-blind, split-mouth clinical study, the PDL injection technique was associated with higher pain scores during injection and extraction compared to routine local infiltration for the nonsurgical extraction of posterior maxillary permanent teeth. Therefore, the null hypothesis was rejected. The present study compared the PDL injection with local infiltration (buccal and palatal injection) for single permanent tooth extraction in the posterior maxilla. The findings indicated that the pain felt during infiltration injection was significantly less than during PDL injection. This was attributed to the number of free nerve endings in the area of needle insertion, which has been related to the perception of pain: whereas the submucosa has fewer, the PDL has an abundant number.40 However, local infiltration technique employed in this study yielded VAS scores in excess of 30 mm. This is similar to other reports,30 and indicates that patients are likely to register at least moderate pain during the infiltration technique.41 Possibly, this can be attributed to the palatal injection rather than the buccal, as a single buccal infiltration has been reported to cause only mild pain.30 Palatal infiltration injection itself has been recognized as one of the most painful injections in dental practice and considered the most common source of fear associated with oral surgical procedures.2 Consequently, this would suggest that the PDL injection could be the most painful injection in dental practice.
In this study, extraction with PDL injection was mild (mean VAS <30 mm), but significantly higher than infiltration injection. This was emphasized by the significant differences in VRS data and the need for additional injections, which were in favor of the infiltration technique. This is in concordance with some recent studies,7,30 which reported very low VAS values for extractions after local infiltration, and attributed this to the relatively porous maxillary bone and to the possible pronounced effect of gravity on the diffusion of anesthetic solution for posterior maxillary teeth compared with anterior teeth. By contrast, it is known that with the PDL injection, perfusion of anesthetic solution to adjacent tissues is less than that in the injected area, particularly when moving from molars toward incisors.42,43 This is attributed to the fact that there is a gradual decrease in size and number of the openings in the lamina dura (the gate through which the LA solution diffuses into adjacent bone marrow) when moving from posterior to anterior teeth.43 Therefore, with regard to PDL injections, patients possibly experienced some pressure transmitted to the area adjacent to the surgical procedure. This is consistent with some studies6,42,44 on the extension of anesthesia after PDL injection: 14.77 mm on the buccal side and 11.18 mm on the palatal side. These figures would indicate that the extension of soft-tissue anesthesia after PDL injection would not exceed the width of two maxillary premolars and could be an explanation of the mild pain felt during extraction on the side of PDL injection. Accordingly, it has been reported44 that PDL injections could be used to obtain single-tooth anesthesia and thus employed as an aid in endodontic diagnosis. Furthermore, the mild extraction pain with PDL injections could be linked to the type and concentration of the anesthetic agent and vasoconstrictor used in this study: higher success ratios have been reported with the use of 3% mepivacaine than with 2%, and with 2% lidocaine with 1:50,000 epinephrine than with 1:100,000.17,45
Injection technique in this study was still found to have a significant influence on injection and extraction pain, regardless of indications for extraction. Interestingly, when anesthetic technique was not considered, specific indications would have a significant input on extraction pain only: extraction of orthodontic teeth was rated as involving less pain than extraction of teeth with periodontitis and profound caries. This is consistent with a recent study,30 and attributed to the possible straightforward and rapid surgical procedures used for orthodontic tooth extraction and to the possible complex and longer surgical procedures used for the extraction of teeth with profound caries.31 Furthermore, periodontally compromised teeth and inflamed gingival tissues might result in an increase in the number of tetrodotoxin-resistant channels (Nav1.8 and Nav1.9),46 and could lead to rapid dissociation of the LA to a cationic form unable to cross the nerve membrane, which would result in inadequate conduction blockade.1
The findings of this study stress the need to consider the new types of anesthetic drugs and models of injection techniques. A CCLADS has been reported to provide more satisfied, accepted, and comfortable block, infiltration, palatal, and periodontal injections than provided by conventional injection techniques.47 In addition, the use of new anesthetic agents known to provide more comfortable, effective, and simple injections than other older agents30 has to be considered. The deposition of articaine/HCl, for example, into the buccal vestibule has to be encouraged in the dental practice to make routine local infiltration achieved by single buccal injection and to avoid the discomfort associated with palatal injection, which remains unpleasant for most patients.30 Such suggestions have to be taken seriously in light of the data known on the fear associated with the LA injection itself, which is often considered a factor in avoidance of dental treatment.2 Despite the aforementioned findings and strengths of this study, it is not without limitations. The possibility of undetected systemic diseases affecting bone and periodontal tissues, particularly in the elderly, and consequently their effect on pain scores were not considered. The influence of patient characteristics, including sex, age, smoking habits, and weight, on pain were not permitted either by the design of this study. In addition, although the model of bilateral symmetrical surgery is used widely for such comparative studies, it can be argued that this type of model is not sound.48 Therefore, future studies have to consider these limitations to confirm the results of this study.
Conclusion
The PDL injection is associated with unfavorable patient responses and less effective anesthesia compared to routine local infiltration for the nonsurgical extraction of one posterior maxillary permanent tooth. Therefore, The PDL injection may not be the alternative anesthetic technique of choice to routine local infiltration for the nonsurgical extraction of posterior maxillary permanent teeth.
Acknowledgment
The author would like to thank Professor Zaid H Baqain, vice-president and senior consultant oral and maxillofacial surgeon at the University of Jordan, for his substantial contributions to conception and design of data, revising it critically for important intellectual content and final approval of the version to be submitted. The author also thanks Dr Mahmood Nassif, maxillofacial resident at the University of Jordan, for his help in performing the extractions.
Disclosure
The author reports no conflicts of interest in this work.
References
Malamed SF. Handbook of Local Anesthesia. 6th ed. St Louis: Elsevier; 2013. | ||
Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128(6):756–766. | ||
Rood JP. The pressures created by inferior alveolar injections. Br Dent J. 1978;144(9):280–282. | ||
Rogers KB, Allen FF, Markiewicz SW. The effect of warming local anesthetic solutions prior to injection. Gen Dent. 1989;37(6):496–499. | ||
Dworkin SF. Psychological considerations for facilitating anesthesia and sedation in dentistry. In: Dionne RA, Laskin DM, editors. Anesthesia and Sedation in the Dental Office. New York: Elsevier; 1986:15–28. | ||
Kaufman E, Epstein JB, Naveh E, Gorsky M, Gross A, Cohen G. A survey of pain, pressure, and discomfort induced by commonly used oral local anesthesia injections. Anesth Prog. 2005;52(4):122–127. | ||
Brunetto PC, Ranali J, Ambrosano GM, et al. Anesthetic efficacy of 3 volumes of lidocaine with epinephrine in maxillary infiltration anesthesia. Anesth Prog. 2008;55(2):29–34. | ||
Haas DA, Harper DG, Saso MA, Young ER. Lack of differential effect by Ultracaine (articaine) and Citanest (prilocaine) in infiltration anaesthesia. J Can Dent Assoc. 1991;57(3):217–223. | ||
Kennedy M, Reader A, Beck M, Weaver J. Anesthetic efficacy of ropivacaine in maxillary anterior infiltration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(4):406–412. | ||
Nusstein J, Wood M, Reader A, Beck M, Weaver J. Comparison of the degree of pulpal anesthesia achieved with the intraosseous injection and infiltration injection using 2% lidocaine with 1:100,000 epinephrine. Gen Dent. 2005;53(1):50–53. | ||
Allen KD, Kotil D, Larzelere RE, Hutfless S, Beiraghi S. Comparison of a computerized anesthesia device with traditional syringe in preschool children. Pediatr Dent. 2002;24(4):315–320. | ||
Moore PA, Cuddy MA, Cooke MR, Sokolowski CJ. Periodontal ligament and intraosseous anesthetic injection techniques: alternatives to mandibular nerve blocks. J Am Dent Assoc. 2011;142 Suppl 3:13S–18S. | ||
Smith GN, Walton RE. Periodontal ligament injection: distribution of injected solutions. Oral Surg Oral Med Oral Pathol. 1983;55(3):232–238. | ||
Blanton PL, Jeske AH. Dental local anesthetics: alternate delivery methods. J Am Dent Assoc. 2003;134(2):228–234. | ||
Hochman MN. Single-tooth anesthesia: pressure-sensing technology provides innovative advancement in the field of dental local anesthesia. Compend Contin Educ Dent. 2007;28(4):186–188. | ||
Yamashiro M, Furuya H. Anesthetic management of a patient with Sturge-Weber syndrome undergoing oral surgery. Anesth Prog. 2006;53(1):17–19. | ||
Malamed SF. The periodontal ligament (PDL) injection: an alternative to inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol. 1982;53(2):117–121. | ||
Smith GN, Walton RE. Periodontal ligament injection: distribution of injected solutions. Oral Surg Oral Med Oral Pathol. 1983;55(3):232–238. | ||
Brkovic BM, Savic M, Andric M, Jurisic M, Todorovic L. Intraseptal vs. periodontal ligament anaesthesia for maxillary tooth extraction: quality of local anaesthesia and haemodynamic response. Clin Oral Investig. 2010;14(6):675–681. | ||
Ram D, Peretz B. The assessment of pain sensation during local anesthesia using a computerized local anesthesia (Wand) and a conventional syringe. J Dent Child (Chic). 2003;70(2):130–133. | ||
Fan S, Chen WL, Pan CB, et al. Anesthetic efficacy of inferior alveolar nerve block plus buccal infiltration or periodontal ligament injections with articaine in patients with irreversible pulpitis in the mandibular first molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(5):e89–e93. | ||
Marin MK. Intraseptal anesthesia in the general dental practice. Compend Contin Educ Dent. 1987;8(3):202–209. | ||
Mansour MS, Adawy AM. The periodontal ligament injection; a solitary method of inducing local anesthesia. Egypt Dent J. 1985;31(2):109–119. | ||
Schenkel JS, Lübbers HT, Metzler P. Die intraligamentäre Anästhesie: eine wertvolle Alternative zu konventionellen Techniken? Swiss Dent J. 2016;126(12):1160–1163. | ||
Jing Q, Wan K, Wang XJ, et al. Effectiveness and safety of computer-controlled periodontal ligament injection system in endodontic access to the mandibular posterior teeth. Chin Med Sci J. 2014;29(1):23–27. | ||
Ma L, Wan K, Jing Q, Kong LJ, Feng Z, Tian BB. Comparison of periodontal ligament anesthesia and submucosal infiltration anesthesia in healthy volunteers. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2014;36(3):271–276. | ||
Elbay UŞ, Elbay M, Kaya E, Cilasun U. Intraligamentary and supraperiosteal anesthesia efficacy using a computer controlled delivery system in mandibular molars. J Clin Pediatr Dent. 2016;40(3):193–199. | ||
Shabazfar N, Daubländer M, Al-Nawas B, Kämmerer PW. Periodontal intraligament injection as alternative to inferior alveolar nerve block: meta-analysis of the literature from 1979 to 2012. Clin Oral Investig. 2014;18(2):351–358. | ||
Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79(2):231–252. | ||
Fan S, Chen WL, Yang ZH, Huang ZQ. Comparison of the efficiencies of permanent maxillary tooth removal performed with single buccal infiltration versus routine buccal and palatal injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(3):359–363. | ||
Badcock ME, Gordon I, McCullough MJ. A blinded randomized controlled trial comparing lignocaine and placebo administration to the palate for removal of maxillary third molars. Int J Oral Maxillofac Surg. 2007;36(12):1177–1182. | ||
Briggs M, Closs JS. A descriptive study of the use of visual analogue scales and verbal rating scales for the assessment of postoperative pain in orthopedic patients. J Pain Symptom Manage. 1999;18(6):438–446. | ||
Marquié L, Duarte LR, Mariné C, Lauque D, Sorum PC. How patients and physicians rate patients’ pain in a French emergency department using a verbally administered numerical rating scale and a visual analog scale. Acute Pain. 2008;10(1):31–37. | ||
de Leon SP, Lara-Muñoz C, Feinstein AR, Wells CK. A comparison of three rating scales for measuring subjective phenomena in clinical research – II: use of experimentally controlled visual stimuli. Arch Med Res. 2004;35(2):157–162. | ||
Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13(4):227–236. | ||
Meechan JG, Day PF. A comparison of intraoral injection discomfort produced by plain and epinephrine-containing lidocaine local anesthetic solutions: a randomized, double-blind, split mouth, volunteer investigation. Anesth Prog. 2002;49(2):44–48. | ||
Polit DF, Beck CT. Resource Manual for Nursing Research. Philadelphia: Wolters Kluwer; 2012. | ||
Madon GA, Madon SG, Madon AD. Failure of inferior alveolar nerve block: exploring the alternatives. J Am Dent Assoc. 2002;133(7):843–846. | ||
Corbett IP, Ramacciato JC, Groppo FC, Meechan JG. A survey of local anaesthetic use among general dental practitioners in the U.K. attending post-graduate courses on pain control. Br Dent J. 2005;199(12):784–787. | ||
Farsakian LR, Weine FS. The significance of needle gauge in dental injections. Compend Contin Educ Dent. 1991;12(4):262–268. | ||
Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72(1):95–97. | ||
Hamad SA. Anaesthetic efficacy of periodontal ligament injection of 2% lidocaine with 1:80,000 adrenaline. Al-Rafidain Dent J. 2006;6(1):26–34. | ||
Birn HA. The vascular supply of the periodontal ligament: an investigation of the number and size of perforations in the alveolar wall. J Periodontal Res. 1966;1(1):51–68. | ||
Simon DE, Jacobs TL, Senia ES, Walker WA. Intraligamentary anesthesia as an aid in endodontic diagnosis. Oral Surg Oral Med Oral Pathol. 1982;54(1):77–78. | ||
Kim S. Ligament injection: a physiological explanation of its efficacy. J Endod. 1986;12(10):486–491. | ||
Amir R, Argoff CE, Bennett GJ, et al. The role of sodium channels in chronic inflammatory and neuropathic pain. J Pain. 2006;7(5 Suppl 3):S1–S29. | ||
Rosenberg ES. A computer-controlled anesthetic delivery system in a periodontal practice: patient satisfaction and acceptance. J Esthet Restor Dent. 2002;14(1):39–46. | ||
Mao J, Price DD, Coghill RC, Mayer DJ, Hayes RL. Spatial patterns of spinal cord [14C]-2-deoxyglucose metabolic activity in a rat model of painful peripheral mononeuropathy. Pain. 1992;50(1):89–100. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.