Back to Journals » International Medical Case Reports Journal » Volume 9
Peribulbar anesthesia causing bilateral orbital hemorrhage
Authors Garft K, Burt P, Burt B
Received 19 May 2015
Accepted for publication 12 September 2015
Published 26 February 2016 Volume 2016:9 Pages 43—46
DOI https://doi.org/10.2147/IMCRJ.S88824
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Kyla Garft,1,2 Peter Burt,1,2 Benjamin Burt1,3
1Bendigo Eye Clinic, Victoria, 2Ophthalmology Education, Monash University Rural Medical School, Melbourne, 3Occuloplastics Department, Royal Victorian Eye and Ear Hospital, Victoria, Australia
Abstract: We report a case of bilateral orbital hemorrhage as a complication of peribulbar anesthesia in a 78 year old man. Initially, unilateral orbital hemorrhage occurred but quickly spread to the contralateral side. Neuroophthalmological assessment revealed a proptosed tense globe with normal retinovascular findings. Visual acuity was adversely affected and this was conservatively managed with no lasting ophthalmic sequela. This patient's case was reported as it illustrates an unusual complication of bilateral spread of orbital hemorrhage secondary to peribulbar anesthesia. It highlights how early ophthalmic assessment can ensure a good visual outcome in the setting of appropriate ophthalmic monitoring. The mechanisms of orbital hemorrhage spread and appropriate management options are discussed.
Keywords: ophthalmic, anesthetic, complication, cataract, retrobulbar, bleeding
Introduction
Retrobulbar hematoma is an uncommon complication of retrobulbar/peribulbar block, which requires urgent decompression to prevent blindness from raised intraorbital pressure.1 Furthermore, bilateral periorbital hemorrhage, as a complication of retrobulbar hematoma, is exceedingly rare.2 To the authors’ knowledge, such a complication resulting from this form of anesthesia has not been previously reported in the current literature.
Case report
A 78-year-old man was scheduled to undergo cataract surgery in the right eye and intraocular lens insertion, but developed a right-sided retrobulbar hemorrhage followed by bilateral periorbital hematoma secondary to right peribulbar anesthesia. This occurred within 1–2 minutes following a peribulbar injection of 6 mL of 50% lignocaine (1%) with 1:100,000 adrenaline and 50% bupivicane with 1:200,000 adrenaline, plus hyalase. This technique included positioning the bevel of the needle sufficiently below the globe to avoid rupturing of the globe, ie, along the inferior orbital rim, and aspirating the syringe prior to injecting to avoid an intravenous injection.
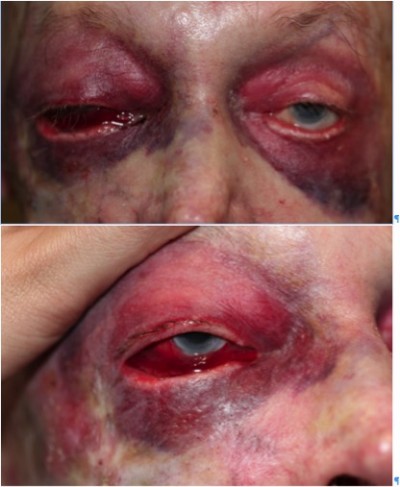
The diagnosis of retrobulbar hemorrhage is made by the presence of proptosis, a fixed dilated pupil, ophthalmoplegia, decreasing visual acuity, and a winking or ischemic optic nerve head.3–5 On examination, proptosis, a tense globe, and a normal optic disc with a normal pulsating central retinal artery were noted (Figure 1). Marked subconjunctival hemorrhage without a posterior limit on the right side, right-sided proptosis, and bilateral periorbital ecchymosis were noted. Visual acuity, pain, ophthalmoplegia, and pupils could not be assessed accurately due to the anesthetic and mydriatic agents administered in preparation for cataract surgery.
  | Figure 1 Facial photographs ~6 hours after surgery. |
Right visual acuity was to count fingers at 1.5 m after 3 hours of injection, although this was likely related to the local anesthetic still dissipating. The patient was admitted for investigations and monitoring, as in all cases of retrobulbar hemorrhage.5 Conservative management was deemed appropriate based on the stability of intraocular pressure measurements and right visual acuity. Visual fields were grossly intact throughout. International normalized ratio, activated partial thrombin time, and platelets were all found to be normal. Visual field deficits had resolved by the following morning when facial photographs were taken (Figure 2).
  | Figure 2 Facial photographs ~20 hours after surgery. |
Medical history was found to be relatively unremarkable with no hypertension, hematological conditions, paranasal sinus surgery, or facial injury. Although he had no previous diagnosis of thrombotic or bleeding disorders, a history of one previous episode of significant bleeding following minimal surgery was elicited on extensive questioning following the incident. The month prior, he had been admitted for unremitting hemorrhage following excision of multiple basal cell carcinomas. This urgent episode was treated conservatively with compression, bed elevation, and ice packs and monitored until the following morning, when visual acuity and fields had returned to baseline. No abnormal blood test results were observed at any point, and the patient was not taking any anticoagulant medication.
On review after 2 weeks, the patient was found to have fully recovered with no persistent symptoms. On examination, intraocular pressure and visual acuity was normal, and residual ecchymosis was still present. He was rebooked for cataract surgery with a sub-Tenon anesthetic block, which was successful and uneventful. There was also an unremarkable review at 4 months, and a preexisting right-sided ectropion was found to have progressed but was asymptomatic (Figure 3).
  | Figure 3 Facial photograph ~4 months later. |
Patient consent was obtained for the purposes of facial photography and de-identified publication. No ethics approval was needed for this case report.
Discussion
We have presented a case of a 78-year-old man who experienced retrobulbar hemorrhage following peribulbar anesthetic injection for phacoemulsification, which subsequently spread to the contralateral eye. This was resolved with conservative management, and the patient later underwent successful lens extraction and intraocular lens insertion.
Successful anesthetic block for the purposes of cataract surgery requires adequate anesthesia and usually akinesia.5,6 A Cochrane Review concluded that there was little difference between anesthesic options with respect to akinesia, development of severe complications, patient acceptability, and failure rates requiring further injections.6 Complications can include ecchymosis, retrobulbar hemorrhage, globe perforation, cranial nerve palsy, and raised intraocular pressure resulting in central retinal artery occlusion and transitory or permanent vision loss and brain stem anesthesia.5–9 Fortunately, these complications are exceedingly rare.6–12 Other documented causes of nontraumatic retrobulbar hemorrhage include vascular malformations, increased venous pressure (during childbirth or Valsalva maneuvres), coagulopathies, orbital lesions, infection, and interestingly scurvy.13,14
Both peribulbar anesthetic injection and topical anesthesia are well established as safe and effective methods to use prior to cataract surgery.6–12 It has been established that when comparing anesthetic options for cataract surgery, a variety of factors must be considered and the optimal option is situationally dependent.4,7 The use of nonsteroidal anti-inflammatory drug medications, aspirin, anticoagulants, and certain supplements, such as St John’s Wort, should be withheld 2 weeks prior to cataract surgery to reduce the risk of bleeding-related complications.4 A 2012 meta-analysis established that topical anesthesia reduces the risk of injection-related complications, such as retrobulbar hemorrhage and chemosis and alleviates patient anxiety regarding injections.7 However, it does not provide comparable analgesia and does not increase intraoperative difficulty, despite increased eye motility.7
Many of these complications are a result of the confined space that is the orbit. The floor, roof, medial and lateral walls, and anteriorly the orbital septum limit the orbital cavity.13,15 This compartment can contain hemorrhages of various origin and they can theoretically spread in multiple ways. The most likely explanation of the spread of hemorrhage to the contralateral eye in this case is either via the loose areolar tissue of the scalp or possibly retroseptal spread.16
The scalp consists of skin, connective tissue, aponeurosis, loose areolar tissue, and pericranium (periosteum of the skull). The loose areolar tissue provides a subaponeurotic potential space within which bleeding can spread. This could potentially spread hemorrhage from one eye to another as this tissue extends beneath orbicularis oculi but could penetrate dehiscences in the contralateral orbital septum.17,18
Retroseptally, the most likely source of spread would be emissary veins in the medial wall allowing spread via the ethmoid cavities or potentially even the cavernous sinus, which is valveless.
The ideal management of retrobulbar hemorrhage is not fully established.18 Management should, however, be done in consultation with an ophthalmologist and involves a thorough clinical assessment and monitoring for deterioration.5,8,19,20 Imaging can be used to confirm diagnosis, though may unnecessarily delay urgent treatment, as retrobulbar hemorrhages can often be diagnosed clinically.4,5
Mild retrobulbar hemorrhages can be managed conservatively.2,8,21–23 In these circumstances, certain factors ought to be optimized in order to reduce the risk of further hemorrhage:8,17,21
- Patients should be advised to avoid coughing or straining.
- The bed head should be elevated at least 45°.
- Blood pressure and coagulopathies should be normalized.
- Ice packs may be of benefit in reducing blood flow and edema.
- Intraocular pressure-lowering medications and high-dose systemic corticosteroids may also play a role.
In the circumstances where conservative management is insufficient to preserve eyesight, surgical intervention may be required.22 This initially involves a lateral canthotomy with an inferior cantholysis.2,3 A canthotomy is an incision of the lateral canthal tendon, and cantholysis is the disinsertion of the canthal tendon from the orbital rim. The aforementioned procedure involves cutting the lateral canthal tendon in a horizontal plane to the orbital rim and dividing the inferior limb until it releases the lower lid tension.
In the event that this does not sufficiently reduce pressure for perfusion to return, the following steps may be performed:2,3,17
- Disinsertion of the superior portion of the canthal tendon.
- The orbital septum may be further surgically detached from the orbital rim.
- A surgical exploration of the lateral wall, followed by the orbital floor and medial wall, if necessary, will definitively relieve pressure within the orbital cavity in the most extreme cases.
However, orbital decompression and optic nerve fenestration are not yet established as efficacious interventions by current data.8,19
Conclusion
In conclusion, nontraumatic bilateral spread of retrobulbar hemorrhage has not been discussed in the current literature. We have presented such a case and speculated on the possible mechanisms of pathogenesis and potential treatments. Important issues raised by this case include the following:
- Practitioners ought to delve extensively into bleeding history prior to undergoing invasive procedures with potentially significant complications.
- Less-invasive anesthetic blocks, such as topical anesthesia or sub-Tenon anesthetic blocks, ought to be considered in such cases.
- Retrobulbar hemorrhage can be managed conservatively in some cases but lateral canthotomy can be a relatively safe, urgent intervention.
Disclosure
The authors report no conflicts of interest in this work.
References
Kallio H, Paloheimo M, Maunuksela EL. Haemorrhage and risk factors associated with retrobulbar/peribulbar block: a prospective study in 1383 patients. Br J Anaesth. 2000;8(5):708–711. | |
Rose GE, Verity DH. Acute presentation of vascular disease within the orbit-a descriptive synopsis of mechanisms. Eye (Lond). 2013; 27(3):299–307. | |
Lima V, Burt B, Leibovitch I. Orbital Compartment Syndrome: the ophthalmic surgical emergency. Surv Ophthalmol. 2009;54(4):441–449. | |
Hislop W, Dutton G, Douglas P. Treatment of retrobulbar haemorrhage in accident and emergency departments. Br J Oral Maxillofac Surg. 1996;34:289–292. | |
Hayter J, Sugar A. An orbital observation chart. Br J Oral Maxillofac Surg. 1991;29:77–79. | |
Alhassan MB, Kyari F, Ejere HO. Peribulbar versus retrobulbar anaesthesia for cataract surgery. Anesth Analg. 2008;107(6):2089. | |
McCombe M, Heriot W. Penetrating ocular injury following local anaesthesia. Aust N Z J Ophthalmol. 1995;23(1):33–36. | |
Smith R. Cataract extraction without retrobulbar anaesthetic injection. Br J Ophthalmol. 1990;74(4):205–207. | |
Kongsap P. Superior subconjctival anesthesia versus retrobulbar anesthesia for manual small-incision cataract surgery in a residency training program: a randomized controlled trial. Clin Ophthalmol. 2012;6:1981–1986. | |
Schrader WF, Schargus M, Schneider E, Josifova T. Risks and sequelae of scleral perforation during peribulbar or retrobulbar anaesthesia. J Cataract Refractive Surg. 2010;36:885–889. | |
Zhao LQ, Zhu H, Zhao PQ, Wu QR, Hu YQ. Topical anesthesia versus regional anesthesia for cataract surgery: a meta-analysis of randomized controlled trials. Am Acad Opthalmol. 2012;119:659–667. | |
Gross A, Cestari D. Optic neuropathy following retrobulbar injection: a review. Semin Ophthalmol. 2014;29(5–6):434–439. | |
McNab A. Nontraumatic orbital haemorrhage. Surv Ophthalmol. 2014;59:166–184. | |
Sloan B, Kulwin DR, Kersten RC. Scurvy causing bilateral orbital haemorrhage. Arch Ophthalmol. 1999;117(6):842–843. | |
Nouvellon E, L’Hermite J, Chaumeron A, et al. Medial canthus episcleral (Sub-Tenon) single injection block. Ophthalmic Reg Anesth. 2004;100:370–374. | |
Bron A, Tripathi R, Tripathi B. Wolff’s Anatomy of the Eye and Orbit. 8th ed. London: Chapman & Hall Medical; 1998. | |
Sinnatamby CS. Last’s Anatomy. 12th ed. New York: Churchill Livingstone; 2011. | |
Karabekir HS, Gocmen-Mas N, Emel E, et al. Ocular and periocular injuries associated with an isolated orbital fracture depending on a blunt cranial trauma: anatomical and surgical aspects. J Craniomaxillo Surg. 2012;40(7):e189–e193. | |
Ord RA, Awty MD, Pour S. Bilateral retrobulbar haemorrhage: a short case report. Br J Maxillofacial Surg. 1986;24(1):1–6. | |
Han JK, Caughey RJ, Gross CW, Newman S. Management of retrobulbar hematoma. Am J Rhinol. 2008;22(5):522–524. | |
McClenaghan F, Ezra D, Holmes S. Mechanisms and management of vision loss following orbital and facial trauma. Curr Opin Ophthalmol. 2011;22:426–431. | |
Popat H, Doyle PT, Davies SJ. Blindness following retrobulbar haemorrhage – it can be prevented. Br J Oral Maxillofacial Surg. 2007; 45(2):163–164. | |
Machado RA, Silveira RL, Borges HO, Filho AM, de Oliveira MG. Retrobulbar hemorrhages: a case report. J Contemp Dent Pract. 2006; 7(2):130–136. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
