Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Percutaneous autologous bone marrow transplantation for the treatment of delayed union of limb bone in children
Authors Wu J, Guo HX, Liu X, Li M, Cao YJ, Qu XY, Zhou H, Weng LQ
Received 14 July 2017
Accepted for publication 22 December 2017
Published 2 February 2018 Volume 2018:14 Pages 219—224
DOI https://doi.org/10.2147/TCRM.S146426
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Jun Wu,* Hongxi Guo,* Xing Liu, Ming Li, Yujiang Cao, Xiangyang Qu, Hai Zhou, Liuqi Weng
Department of Orthopaedics, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Engineering Research Center of Stem Cell Therapy, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Background and purpose: Percutaneous autologous bone marrow transplantation (PABMT) is a minimally invasive therapeutic strategy for the treatment of delayed bone union in adults, which has been confirmed by many studies. However, there is no report on PABMT application in pediatric orthopedic surgery. The aim of this article was to analyze the therapeutic effect of PABMT in children with delayed union of limb bone and its influence in relation to delayed bone union therapy, transplantation period, patients’ sex, fracture location, and fracture fixation.
Methods: In this study, 53 patients (aged 3–16 years, with an average age of 6.7 years) with delayed union of long bone (20 femurs, 12 tibiae, 10 humeri, 5 radiuses, 5 ulnas, and 1 fibula) were treated using PABMT. Clinical examination and X-ray were integrated to evaluate the therapeutic effect.
Results: All 53 patients were followed up for 2–6 years (average time, 3.5 years). Of the 53 patients, 47 (88.7%) were healed, whereas the other 6 (11.3%) were not, and were subsequently treated by autologous bone grafting. In 30 patients who received their first PABMT treatment 6–8 months after fixation, the clinical cure rate, operation times, and healing time were 83.3%, 5.8±0.5 months, and 2.5±0.6, respectively. In the other 23 patients, whose first PABMT treatments were started within 4 to 6 months after fixation, the clinical cure rate, operation times, and healing time were 95.7% (P=0.167), 3.2±0.3 months (P=0.001), and 1.3±0.6 (P=0.001), respectively. The patients’ sex, fracture location, and fracture fixation did not have statistical influence on the clinical efficacy.
Conclusion: PABMT is a minimally invasive and effective strategy for the treatment of delayed union of limb bone in children. The early surgical treatment facilitates the fracture healing, reduces the number of transplantation, and shortens the course of treatment.
Keywords: fracture, minimally invasive, medulla ossium, mesenchymal stem
Introduction
Fracture healing is a complex and well-orchestrated physiological process.1 Most fractures are able to reunite through satisfactory reduction, fixation, and appropriate rehabilitative functional training. The average fracture healing time of long bones of the limb in children is approximately 4 months. However, if the mechanical and biological factors are impaired, the emergence of callus is interrupted, leading to the delay of bone union.2 The fractures which have failed to achieve radiographic progression of healing or an unstable fracture on clinical examination in the duration of average healing time of the same location and type, are called delayed bone union, defined by the US Food and Drug Administration. The delayed bone union, accounting for 5%–10% of all fractures, seriously affects physical and mental health of the patients, inevitably gives the family and society a heavy burden, and is a challenge for orthopedic surgeons.3
The therapeutic strategies for delayed bone union fall into three types: invasive, minimally invasive, and noninvasive. The noninvasive therapeutic strategies, including ultrasound, electrical stimulation, electromagnetic stimulation, and shock wave, are effective adjuvant therapy for delayed bone union.4–7 The invasive therapeutic strategies such as autologous bone graft, vascularized bone (periostea) flap graft, and allograft implantation are the most common treatment methods for delayed bone union.8 Moreover, autologous bone graft has been the “gold standard” for the treatment of fractures and nonunion since 1947.9 However, the clinical application of autologous bone graft is restricted owing to the limited bone supply, nerve injury, pain, hematoma, and infection in donor site.10 The minimally invasive therapeutic strategies for delayed bone union, which include injection of bone marrow, stem cells, bone morphogenetic protein, or growth factors into the sites of fracture delayed union, are under intense investigation and widely used in clinical practice to accelerate fracture repair.11
The percutaneous autologous bone marrow transplantation (PABMT) is a minimally invasive therapeutic strategy for the treatment of delayed bone union. PABMT was first reported in 1986 by Connolly et al,12 confirmed by their following studies and other researchers’ reports.13–15 Nowadays, PABMT is considered as an alternative to the invasive therapeutic strategies to achieve good clinical efficacy due to its low complications. However, as far as we know, there has not been any report on its application in pediatric orthopedic surgery. Over a period of 8 years, 53 children with delayed union of long bone were treated using PABMT in our hospital and followed up for an average of 3.5 years. In this study, we present outcomes of the follow-up to evaluate the clinical effects of PABMT for the treatment of delayed union of limb bone in children.
Methods
Patients
This study was approved and supervised by the Ethics Committee of the Children’s Hospital of Chongqing Medical University and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. The patients were strictly selected by diagnostic criteria, inclusion criteria, and exclusion criteria. A delayed union was defined as the absence of radiographic progression of healing or an unstable fracture on clinical examination between 4 and 6 months after injury.16 Inclusion criteria and exclusion criteria are listed in Table 1. According to the diagnostic, inclusion, and exclusion criteria, 53 patients with delayed union of long bone were involved in this study. A flow chart is shown in Figure 1. Prior to the operations of PABMT, the parents or guardians of the patients signed an informed consent to participate in the study and to authorize the publication of the results and use of photographs of their children. Surgical opportunity was determined by the parents or guardians. According to the period from fracture fixation to the first operation of PABMT, the children were divided into two groups: the 4- to 6-month group and the 6- to 8-month group.
  | Table 1 The inclusion criteria and exclusion criteria |
  | Figure 1 Flow chart of PABMT for delayed bone union in children. |
Surgical procedure
The surgical procedure was performed according to the Hernigou’s method, which was described in detail in the Journal of Bone and Joint Surgery.17 Briefly, the patients in supine position underwent satisfactory general anesthesia, and their surgical sites were prepared and draped in a sterile fashion. Bone marrow was harvested from the anterior iliac crest with an 11-gauge spinal needle (Gallini, Mirandola, Italy) and aspirated into a 20-mL heparinized plastic syringe. The needle was turned 45° between each aspiration to achieve successive aspiration from the largest possible space. The needle was turned more than 2 cm between each insertion site, and no more than 2 mL of marrow should be harvested in each insertion site, to reduce the degree of dilution by peripheral blood. The same needle, which was used to aspirate the bone marrow, was percutaneously inserted at the nonunion gap under a C-arm fluoroscope. Prior to the injection of the bone marrow, the intervening fibrous tissues should be peeled off with the needle, but no attempt should be made to remove the callus or fibrous tissue. The average bone marrow of 12.7 mL (range, 5–20 mL) was injected slowly, at the rate of about 20 mL per minute, to avoid marrow extravasation and a fat embolism syndrome. The patients received repeated PABMT every 1–2 months until the fractures achieved clinical union. However, if there was no progress in fracture healing after three injections, other surgical methods were used.
Follow-up
The patients should avoid load bearing during the first month after the PABMT, and the clinical examination and X-ray imaging tests were integrated to determine the time of load bearing and to evaluate the efficiency of bone marrow grafting. The patients were followed up every 1–2 months until the fractures achieved clinical union. The criteria of clinical bone union were defined by total weight bearing without pain and macro mobility at fracture site associated with cortical bridging and no fracture line on the anteroposterior and lateral X-ray films. The number of PABMT surgical procedures, healing time, and clinical cure rate were recorded and evaluated.
Statistics
Statistical analysis was performed with the IBM SPSS Statistics 17.0 (IBM Corporation, Armonk, USA). The clinical cure rate and number of operations were analyzed using chi-square test. A Spearman correlation test was used for healing time analysis. P<0.05 was considered as statistically significant.
Results
This study included 53 patients, 35 boys and 18 girls, aged from 3 to 16 years with an average age of 6.7 years. The delayed bone union was present in the femur (20 cases), tibia (12 cases), humerus (10 cases), radius (5 cases), ulna (5 cases), and fibula (1 case). Of the 53 fractures, 26 (49.1%) were treated by external fixation, 14 (26.4%) by plate fixation, 7 (13.2%) by intramedullary nailing, and the other 6 (11.3%) by Kirschner wire fixation. No patient suffered from local or systemic complications associated with the bone marrow transplantation procedure, such as infection, fat embolism, and compartment syndrome, and all patients were discharged within 48 hours after the surgical procedure. No patient showed oncological pathology at the injection site.
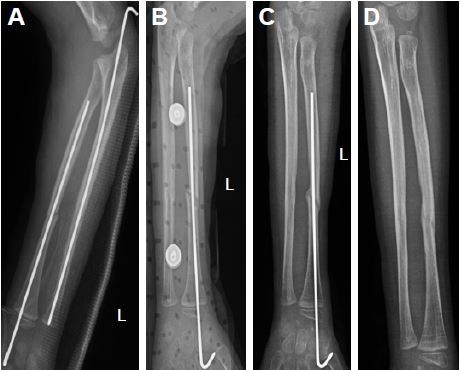
The patients were followed up for 2–6 years (average, 3.5 years). Of the 53 cases, 47 (88.7%) were healed by 2.0±0.8 surgical procedures within 4.8±1.6 months. The X-ray images of typical cases are shown in Figures 2 and 3. After three surgical procedures of PABMT, the other six patients (11.3%) still failed to achieve progress in bone union, suggested by the clear fracture lines with little callus and fracture end sclerosis in their X-ray films, and were subsequently treated by autologous bone grafting.
The clinical efficacy was significantly affected by the transplantation period (Table 2). In 30 patients who received their first PABMT treatment 6–8 months after fixation, the clinical cure rate, healing time, and operation times were 83.3%, 5.8±0.5 months, and 2.5±0.6, respectively. In the other 23 patients, who received first PABMT treatment within 4–6 months after fixation, the clinical cure rate, healing time, and operation times were 95.7% (P=0.167), 3.2±0.3 months (P=0.001), and 1.3±0.6 (P=0.001), respectively.
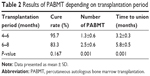  | Table 2 Results of PABMT depending on transplantation period |
However, the patients’ general characteristics such as sex, fracture location, and fixation did not have statistical influence on PABMT results.
Discussion
Bone marrow has been demonstrated to have great osteogenic properties and has already been widely used as a bone graft substitute in basic research and clinical practice. In 1869, Goujon first demonstrated the osteogenic capacity of the bone marrow in rabbit.18,19 Thereafter, it was found by numerous studies that the ossifying property of bone marrow was mainly due to bone mesenchymal stem cells (BMSCs) within the bone marrow.13,20 The BMSCs had multidirectional differentiation potential that could proliferate and differentiate into osteoblasts, chondrocytes, and adipose cells under the stimulation of bone induction signal.21 Hernigou et al17 found that the number and concentration of fibroblast colony-forming units (CFU-F) in the graft was closely related to the healing rate and time needed for union. They found that the patients could not obtain bone union if the concentration of progenitors injected into the nonunion sites was less than 634±187 progenitors/mL and total numbers were less than 19,324±6,843. Since the number of progenitor cells available in the bone marrow aspirated from the iliac crest was less than required concentration, the aspirated bone marrow should be concentrated by filtration and centrifugation. The surgical technique was adopted and confirmed by numerous studies.14,15,22,23
However, in this study, the bone marrow aspirated from the iliac crest was directly injected into the delayed union sites. The results of this study showed that the healing rate was 88.7%, which was comparable with 88.3% reported in the study by Hernigou et al17 in 2006 and 76.0% reported in the study by Sugaya et al15 in 2014. The finding was associated with the following reasons. First, there was a significant difference in the age of the participants. The patients in this study were children, whereas most participants reported in literature were adult and elderly people. The marrow of the long bone in children mostly was red marrow, being rich in primitive osteogenic cells or hematopoietic cells that were responsible for the bone marrow osteogenic capacity. Since the end of growth and development stage, the red marrow in the long bone had been gradually substituted for yellow marrow containing fat, which is hematopoietically inactive.24 It had been reported by Gross et al25 that the time to healing would be increased with patients’ age. Second, the bone morphogenetic protein and other bone growth factors contained in the bone marrow matrix also contributed to the bone marrow osteogenic capacity.25,26 Currently, more and more researchers have stressed the importance of appropriate biological environment in fracture healing and that the lack of osteoblast and growth factors was an important risk factor for delayed union and nonunion.27–29 Unconcentrated bone marrow transplantation could provide both osteoblast and growth factors to promote fracture healing, which provided the theory basis for the clinical treatment of delayed union with bone marrow.
The results also showed that the mean volume of injected bone marrow was 12.7 mL, ranging from 5 to 20 mL. According to the study by Hernigou et al,17 the marrow extravasation and a fat embolism syndrome would not occur if the injection volume was less than 20 mL, which was consistent with our study.
The surgical procedure of PABMT without filtration and centrifugation is more simple and easy to master, contributing to promotion and application, in areas with poor medical conditions.
Another crucial issue in the treatment of delayed bone union with PABMT is the treatment opportunity, which has not reached agreement all over the world. As shown in this study, the time since fixation to first PABMT significantly influenced the required number of PABMT procedures and clinical healing time. The early bone marrow transplants facilitate the fracture healing, reduce the number of transplantations, and shorten the course of treatment. Since the delayed bone union has an insidious onset and is difficult in early diagnosis, PABMT treatment should be done once the delayed bone union is diagnosed.
PABMT is a simple, safe, minimally invasive, and effective strategy for the treatment of delayed bone union in children. However, the limitation of this study is the lack of a series of randomized controlled studies to explore in detail the influencing factors of therapeutic efficacy of PABMT for delayed bone union in children. Moreover, the children underwent more than one operation to achieve clinical fracture healing. In our next studies, some effective measures should be taken to reduce the number of surgical operations, minimize suffering, speed up recovery, and cut hospital fees.
According to the literature and empirical findings of this study, the authors have developed some experience in the treatment of delayed union of long bone in children with PABMT. First, strict indication is an important procedure for the success of PABMT. PABMT is an effective treatment for uninfected delayed union of limb bone which followed a stable fracture fixation without severe angular deformity or shortening. It is likely to fail if the fracture was a pathological fracture or infected fracture, if there is an unhealed wound and fistula around the fracture site, or if the gap between fragments exceeds 5 mm. Second, the needle is turned more than 2 cm between each insertion site and no more than 2 mL of marrow should be harvested in each insertion site to reduce the degree of dilution by peripheral blood. Third, although transplantation of untreated autologous bone marrow has a good therapeutic effect on delayed union of long bone in children, the bone marrow should be concentrated before injecting into the nonunion site in adults, because osteogenic capacity of the bone marrow is positively associated with the cell concentration, which has been confirmed by many studies.14,15,17,24 Fourth, the intervening scar tissue should be peeled off with the needle to facilitate the injection of bone marrow and to restart the fracture healing process by forming a microfracture. However, no attempt should be made to remove the callus or fibrous tissue. Fifth, special attention should be paid to avoid injury of nerves and vessels during the percutaneous insertion of the needle. The bone marrow should be injected slowly to avoid marrow extravasation and a fat embolism syndrome. Sixth, the transplantation of autologous bone marrow could be repeated once every 1 or 2 months, according to the progress of bone union. But transplantation should not be repeated more than three times. If the fracture remained unhealed after three transplantations, other treatments should be considered, such as bone grafting Finally, since premature load bearing hampered the progress of bone healing, the patients should avoid load bearing during the first month after PABMT. After 1 month, if callus was observed in the X-ray films, the patients were allowed to start weight bearing gradually.
Conclusion
In this study, most children achieved bone healing by percutaneous autologous bone marrow transplantation with rigorous indications, meticulous surgical operation, and appropriate rehabilitative training. According to the empirical findings of this study and the literature, PABMT is a simple, safe, minimally invasive, and effective strategy for the treatment of delayed union of long bone in children. What is more, the early bone marrow transplants facilitate the fracture healing, reduce the number of transplantations, and shorten the course of treatment.
Acknowledgments
The authors warmly thank Bin Qin (Department of Radiology, Children’s Hospital of Chongqing Medical University, Chongqing, People’s Republic of China) for providing X-ray images. They also thank Chuankang Liu, Cong Luo, and Chao Zheng (Department of Orthopaedics, Children’s Hospital of Chongqing Medical University, Chongqing, People’s Republic of China) for their contributions to the study design and acquisition, and analysis of data. This study was funded by the National Key Clinical Specialist Construction Programs of China (2013 544) and Key Program of Health and Family Planning Commission of Chongqing (2013 39).
Disclosure
The authors report no conflicts of interest in this work.
References
Rosset P, Deschaseaux F, Layrolle P. Cell therapy for bone repair. Orthop Traumatol Surg Res. 2014;100(1 suppl):S107–S112. | ||
Santolini E, West R, Giannoudis PV. Risk factors for long bone fracture non-union: a stratification approach based on the level of the existing scientific evidence. Injury. 2015;46(suppl 8):S8–S19. | ||
Hak DJ, Fitzpatrick D, Bishop JA, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury. 2014;45(suppl 2):S3–S7. | ||
Watanabe Y, Arai Y, Takenaka N, Kobayashi M, Matsushita T. Three key factors affecting treatment results of low-intensity pulsed ultrasound for delayed unions and nonunions: instability, gap size, and atrophic nonunion. J Orthop Sci. 2013;18(5):803–810. | ||
Paterson D. The use of electricity in the treatment of nonunion. Instr Course Lect. 1988;37:155–156. | ||
Adie S, Harris IA, Naylor JM, et al. Pulsed electromagnetic field stimulation for acute tibial shaft fractures: a multicenter, double-blind, randomized trial. J Bone Joint Surg Am. 2011;93(17):1569–1576. | ||
Zelle BA, Gollwitzer H, Zlowodzki M, Bühren V. Extracorporeal shock wave therapy: current evidence. J Orthop Trauma. 2010;24(suppl 1):S66–S70. | ||
Emara KM, Diab RA, Emara AK. Recent biological trends in management of fracture non-union. World J Orthop. 2015;6(8):623–628. | ||
Phemister DB. Treatment of ununited fractures by onlay bone grafts without screw or tie fixation and without breaking down of the fibrous union. J Bone Joint Surg Am. 1947;29(4):946–960. | ||
Summers BN, Eisenstein SM. Donor site pain from the ilium: a complication of lumbar spine fusion. J Bone Joint Surg Br. 1989;71(4):677–680. | ||
Pountos I, Georgouli T, Kontakis G, Giannoudis PV. Efficacy of minimally invasive techniques for enhancement of fracture healing: evidence today. Int Orthop. 2010;34(1):3–12. | ||
Connolly JF, Shindell R. Percutaneous marrow injection for an ununited tibia. Nebr Med J. 1986;71(4):105–107. | ||
Tiedeman JJ, Connolly JF, Strates BS, Lippiello L. Treatment of nonunion by percutaneous injection of bone marrow and demineralized bone matrix: an experimental study in dogs. Clin Orthop Relat Res. 1991;268:294–302. | ||
Le Nail LR, Stanovici J, Fournier J, Splingard M, Domenech J, Rosset P. Percutaneous grafting with bone marrow autologous concentrate for open tibia fractures: analysis of forty three cases and literature review. Int Orthop. 2014;38(9):1845–1853. | ||
Sugaya H, Mishima H, Aoto K, et al. Percutaneous autologous concentrated bone marrow grafting in the treatment for nonunion. Eur J Orthop Surg Traumatol. 2014;24(5):671–678. | ||
Said GZ, Farouk O, Said HGZ. Delayed union of multifragmentary diaphyseal fractures after bridge-plate fixation. Int Orthop. 2009;33(2):549–553. | ||
Hernigou P, Mathieu G, Poignard A, Manicom O, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions: surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1):322–327. | ||
Goujon E. Recherches expérimentales sur les propriétés physiologiques de la moelle des os. [Research experiments on the physiological properties of medulla ossium]. J Anat Physiol. 1869;6:399–412. French. | ||
Connolly JF. Injectable bone marrow preparations to stimulate osteogenic repair. Clin Orthop Relat Res. 1995;313:8–18. | ||
Liebergall M, Schroeder J, Mosheiff R, et al. Stem cell-based therapy for prevention of delayed fracture union: a randomized and prospective preliminary study. Mol Ther. 2013;21(8):1631–1638. | ||
Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143–147. | ||
Niikura T, Miwa M, Lee SY, et al. Technique to prepare the bed for autologous bone grafting in nonunion surgery. Orthopedics. 2012;35(6):491–495. | ||
Braly HL, O’Connor DP, Brinker MR. Percutaneous autologous bone marrow injection in the treatment of distal meta-diaphyseal tibial nonunions and delayed unions. J Orthop Trauma. 2013;27(9):527–533. | ||
Burwell RG. The function of bone marrow in the incorporation of a bone graft. Clin Orthop Relat Res. 1985;200:125–141. | ||
Gross JB, Diligent J, Bensoussan D, Galois L, Stoltz JF, Mainard D. Percutaneous autologous bone marrow injection for treatment of delayed and non-union of long bone: a retrospective study of 45 cases. Biomed Mater Eng. 2015;25(suppl 1):187–197. | ||
Garrison KR, Shemilt I, Donell S, et al. Bone morphogenetic protein (BMP) for fracture healing in adults. Cochrane Database Syst Rev. 2010;6:CD006950. | ||
Ollivier M, Gay AM, Cerlier A, Lunebourg A, Argenson JN, Parratte S. Can we achieve bone healing using the diamond concept without bone grafting for recalcitrant tibial nonunions? Injury. 2015;38(7):1383–1388. | ||
Ghiasi MS, Chen J, Vaziri A, et al. Bone fracture healing in mechanobiological modeling: A review of principles and methods. Bone Rep. 2017;16(6):87–100. | ||
Kostenuik P, Mirza FM. Fracture healing physiology and the quest for therapies for delayed healing and nonunion. J Orthop Res. 2017;35(2):213–223. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


