Back to Journals » Journal of Pain Research » Volume 13
Perceptions and Beliefs Regarding NSAIDs in the Asia-Pacific Region
Authors Ho KY
Received 31 August 2019
Accepted for publication 12 February 2020
Published 21 February 2020 Volume 2020:13 Pages 437—446
DOI https://doi.org/10.2147/JPR.S229387
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Kok-Yuen Ho
The Pain Clinic, Mount Alvernia Hospital, Singapore
Correspondence: Kok-Yuen Ho
The Pain Clinic, Mount Alvernia Hospital, 820 Thomson Road – 07-59, 574623, Singapore
Tel/Fax +65 6 254 5447
Email [email protected]
Background: Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used in the treatment of pain and inflammation. However, chronic NSAID use may result in gastrointestinal (GI), cardiovascular (CV), renal or other safety concerns, especially in high-risk populations. The aim of this review is to systematically identify relevant literature and to organize available evidence for perceptions or beliefs of physicians and patients about the safety and efficacy of NSAIDs.
Methods: A systematic literature search was conducted in MEDLINE® (through PubMed®), Embase® (through Ovid®), and the Cochrane Library. Additional unstructured searches were conducted using Google Scholar™ and Google. The scope of this study did not include grey literature searches or handpicking of cross references. This systematic analysis was conducted with a special interest in studies conducted in the Asia-Pacific (APAC) region and information related to the COX-2 (cyclooxygenase-2) selective inhibitors.
Results: Out of a total of 2822 studies retrieved from different databases (PubMed®, Cochrane, Google Scholar™ and Embase®), 99 (3.5%) met the inclusion criteria. Further, out of these 99 studies, 23 APAC region studies were analyzed. The common perceptions were related to GI, CV, renal and respiratory safety, efficacy and COX-2 inhibitors.
Conclusion: Overall, the level of awareness among patients regarding NSAIDs was observed to be considerably poor. Moreover, risk stratification by physicians must be practiced in order to decrease the incidence of adverse events.
Keywords: cardiovascular, COX-2 inhibitors, efficacy, gastrointestinal, renal, respiratory
Introduction
Non-steroidal anti-inflammatory drugs (NSAIDs) are extensively used in the management of symptomatic pain and inflammation in several acute and chronic conditions. NSAIDs can be purchased over-the-counter (OTC) in many countries, which in turn contributes to their increased use.1,2
Chronic use of NSAIDs is associated with gastrointestinal (GI), cardiovascular (CV), and renal toxicity.3 Over the last few years, a large number of studies have been carried out to understand the toxic effects of NSAIDs and further evaluated the overall safety of non-selective and cyclooxygenase (COX)-2 selective inhibitors.3–6 However, these updates may not have reached practicing physicians due to a lack of continuing education and appropriate scientific communication. In general, NSAID users were found to have poor knowledge of NSAID-associated risks.7 As prescribers, physicians play an important role in conveying medication risk and safety information to the patients. Little is known about physicians’ attitudes to NSAIDs or their perceptions of the risks associated with NSAID use.7 The probability of under-prescription of NSAIDs due to bias among clinicians against the safety of NSAIDs cannot be eliminated, which may interfere with effective pain management strategies. The limited research in this area warrants the need to investigate the current perceptions or beliefs of physicians or patients with respect to the safety and efficacy of NSAIDs.
Methods
Definitions
Non-Steroidal Anti-Inflammatory Agents
As per Medical Subject Heading (MeSH®) dictionary of PubMed®, NSAIDs are
Anti-inflammatory agents that are non-steroidal in nature. In addition to anti-inflammatory actions, they have analgesic, antipyretic, and platelet-inhibitory actions. They act by blocking the synthesis of prostaglandins by inhibiting cyclooxygenase, which converts arachidonic acid to cyclic endoperoxides, precursors of prostaglandins. Inhibition of prostaglandin synthesis accounts for their analgesic, antipyretic, and platelet-inhibitory actions; other mechanisms may contribute to their anti-inflammatory effects.
Eligibility Criteria
Predefined unambiguous eligibility criteria have been established in order to carry out this systematic review. The types of studies, interventions and participants have been classified into the inclusion and exclusion criteria as mentioned below:
Inclusion Criteria
- Subjects of any age and sex
- Health-care professionals including specialist and general physicians or dentists, and allied health including pharmacists, nurses, physiotherapists, etc.
- Study conducted in any clinical setting or geographical area
- Any therapeutic area
- All NSAIDs
- Outcomes related to perception, knowledge, awareness, and prescribing pattern
- English language
- Human studies
- Original articles
- Opinion-based articles
- Publication between 2008 and 2018
Exclusion Criteria
- Preclinical studies
- Meta-analysis/systematic review
- Narrative reviews summarizing previously published data only
- Case reports
- Case series
- Conference abstracts
- Clinical practice guidelines
- Non-NSAIDs with anti-inflammatory activity (such as plant oils of omega-3-fatty acids)
- Outcomes related to pain perception (effect of a drug on pain intensity/pain score/patient’s perception of pain, ie, clinical efficacy endpoints of NSAIDs)
Search Strategy
A literature search through electronic platforms was conducted to identify relevant peer-reviewed, bibliographic publications. The scope of search included freely accessible data sources, except Embase®.
PubMed® Search Strategy
A MEDLINE® search through PubMed® was conducted on 30 July 2018 using the search strategy summarized in Table 1.
 |
Table 1 MEDLINE® Search Strategy Through PubMed® |
Embase® Search Strategy
An Embase® search through Ovid® was conducted using same entry terms that were used for PubMed® search on 12 September 2018 (Table 2).
 |
Table 2 Embase® Search Strategy Through Ovid® |
Data Collection and Analysis
Data Management and Storage
References retrieved from electronic databases were imported using the reference manager, EndNote™ X8 and de-duplicated using the inbuilt de-duplication functionality of EndNote. De-duplicated references were exported to Microsoft Excel from EndNote and further screened manually to validate accuracy.
Screening and Study Selection
The study selection process took place in two steps. In the first step, two reviewers independently reviewed the title and abstract of each study obtained from the electronic searches and made a decision about selection using predefined inclusion/exclusion criteria. Discrepancies were discussed, and if unresolved, a third reviewer took the final decision. The second step was based on the full-text review of the articles included in the first step by a single reviewer.
Data Extraction
Data from the full-text selected papers were extracted using a pre-approved data extraction form (DMF) and stored in MS Excel. Data extraction was carried out by a single reviewer. Since most of the data obtained were textual, large fragments of text were extracted in DMF from source articles and summarized as text documents.
Results
Overview of Search results
Of 2,822 studies retrieved from different databases, 99 (3.5%) were included in the analysis (Figure 1). Out of these 99 studies, 23 were related to the APAC (Asia-Pacific) region only, as described in Table 3.7–29
 |
Table 3 Characteristics of Asia-Pacific (APAC) Studies |
 |
Figure 1 PRISMA flow diagram, study selection flow. Abbreviation: APAC, Asia-Pacific. |
Studies that had findings related to prescription patterns only and did not report perceptions/beliefs/practices leading to those patterns were excluded from the final analysis. A wide variety of population samples were studied, which were classified as general physicians, specialists (eg, anesthesiologists, rheumatologists), paramedics, medical students, general population, subpopulation of patients, or prescriptions. The population samples were classified into four categories: physicians, patients, students, and prescriptions. Among the 23 APAC studies that were included in this review, patients comprised the highest population sample (30%) (Figure 2). Different outcomes included perceptions related to NSAIDs’ safety, efficacy, and usage; level of awareness, extent of self-medication, polypharmacy, and inappropriate usage.
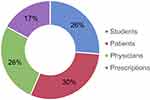 |
Figure 2 Distribution of included studies (Asia-Pacific) by population studied. |
Physicians’ Perceptions on NSAID Risks
A retrospective study from the APAC region (Hong et al, Korea) compared the prescription patterns of internists and physicians.9 Internists were unaware of the hepatic effects of acetaminophen and prescribed it to patients with liver cirrhosis, while physicians were cautious and preferred prescribing NSAIDs over acetaminophen in the same group of patients. In the study by Choudhary et al, among health-care professionals, physicians (66.7%), nurses (60.9%), and pharmacists (47.8%) displayed a moderate level of awareness regarding the major AEs (adverse events) associated with NSAID use.22 On the contrary, Phueanpinit et al, found that majority of orthopedic physicians took patients’ history (GI, CV, renal, allergy to NSAIDs, patient’s age) into consideration before prescribing non‐selective NSAIDs.7
Perceptions Related to Gastrointestinal Safety
In Thailand, 95.5% (n=63) orthopedic physicians were aware that a history of GI ulcers or bleeding must be considered before prescribing NSAIDs.7 The risk of GI ulceration or bleeding was the second most common concern after a patient’s medical history of renal impairment.7 Around 63.1% of physicians had a moderate attitude towards providing information on AE management and monitoring to patients.7
Although prescription of gastro-protective agents, such as histamine type-2 (H2) blockers and proton pump inhibitors (PPIs) is common practice in the rest of the world, only a few professionals in a few APAC regions, namely, Malaysia and Pakistan preferred prescribing PPIs and H2 receptor blockers for gastroprotection.20,26 Prescribers in the APAC region preferred COX-2 inhibitors to avoid GI AEs, especially in high-risk populations.20
Perceptions Related to Cardiovascular Safety
Amongst untoward CV effects, risk of hypertension in susceptible populations was the only identified concern.7 In an interview of 100 dentists in Chennai, India (Ravinthar et al, India), 6% of the participants identified hypertension as a contraindication of NSAIDs, indicating a low level of awareness among prescribers.28 In another study from the APAC region (Chen et al, Pakistan), it was clearly stated that physicians prescribing NSAIDs or pharmacists who dispense NSAIDs do not query patients regarding comorbidities and concomitant medications, which may further increase the incidence of CV-related AEs among patients.21
In a Thai study conducted among 206 orthopedic physicians, 72.1% of participants reported to have observed hypertension in patients taking NSAIDs.7 A very small proportion of physicians (15.6%) informed patients regarding the CV effects of NSAIDs.
Perceptions Related to Renal Safety
In north-eastern Thailand, most physicians (98.5%) were aware that NSAIDs might be associated with renal impairment and considered this factor before prescribing NSAIDs to patients who were already at a higher risk of developing renal complications.7 Renal function was deemed the risk factor of greatest concern for prescribing any NSAID. Three out of four orthopedic physicians claimed that they provided adverse drug reaction (ADR) information related to prescription NSAIDs, but ADR monitoring and management (29.7%, and 37.5%, respectively) information was provided less frequently to patients.7
Perceptions Related to Respiratory Safety
In a study involving dentists (Ravinthar et al, India), 25% of participants reported that bronchial asthma was the second most common contraindication to the use of NSAIDs.28
Patients’ Perceptions on NSAID Risks
The awareness of NSAID risks varied among patients. One Indian study (Jagdish et al) reported low NSAID awareness among patients (21.3%) while another study (Ahmad et al, India) found that a considerable proportion (75%) of patients were aware that chronic use of NSAIDs may be associated with the occurrence of AEs.11,19
Perceptions Related to Gastrointestinal and Renal Safety
Lack of awareness among patients regarding safe usage of NSAIDs was a common finding in APAC as well as the rest of the world, especially among patients practicing self-medication. One study (Phueanpinit et al, Thailand) showed that 80% of the patients (n=140) were aware that long-term therapy, high dose, and the presence of underlying GI or renal disease could increase the risk of AEs.27 In this questionnaire-based study, approximately half of NSAID users had received information about potential side effects, whether from physicians or pharmacists,27 which corroborates with the lack of sufficient knowledge transfer reported.7 They believed that physicians may be more likely to inform patients about GI risks than other risks.27
Physicians’ Perceptions Related to COX-2 Inhibitors
An observational study evaluated the use of celecoxib in hospitals across Malaysia (Chan et al, Malaysia) and assessed the perceptions of physicians regarding the use of celecoxib and non-selective NSAIDs.20 The study demonstrated that physicians considered GI safety profile (65.9%), efficacy (23.7%), and CV safety profile (3.8%) when choosing between COX-2 selective inhibitors and non-selective NSAIDs. Most physicians (51.8%) believed that celecoxib was more effective as an anti-inflammatory and analgesic agent.20 Most physicians (90%) perceived that celecoxib had a better GI safety profile than a non-selective NSAID and preferred COX-2 selective inhibitors over a combination of non-selective NSAIDs and PPIs in patients with GI risk.20 The reasons cited were similar efficacy between celecoxib and non-selective NSAIDs as well as affordability.20
A study among Filipino surgeons (de Leon et al, Philippines) observed that COX-2 selective inhibitors were preferred as the first-line treatment for pain management followed by weak opioid + COX-2 selective NSAID, weak opioid alone, and non-selective NSAID + weak opioid.23 Preference for COX-2 selective inhibitors for pain management was because of the greater efficacy and better safety profile of this class of drug.23 Also, COX-2 selective inhibitors were being marketed widely and were popular among the Filipino surgeons.23
Patients’ Perceptions Related to COX-2 Inhibitors
In an observational study (Antappan et al, India) conducted in an orthopedic department, patients were asked about risk factors including concomitant use of anticoagulants or selective serotonin reuptake inhibitors, comorbidities (CV, renal, hepatic diseases, diabetes), old age (>65 years), poor health status, history of GI symptoms, heavy smoking and drinking.29 COX-2 selective inhibitors were prescribed to patients with these risk factors in order to prevent GI-related AEs. However, the frequency of COX-2 selective inhibitors usage was lower, ranging from 1% to 11.4% of patients with these risk factors.29
Polypharmacy and Self-Medication Risks
Polypharmacy was found to be a widespread practice in the APAC region. Two Indian studies (Mudhaliar et al; Purkayastha et al) reported prevalent use of NSAID fixed dose combinations (FDCs).13,15 The authors concluded that the indiscriminate use of FDCs may increase the incidence of AEs while, combining opioid analgesics may be a better option to achieve the desired analgesic efficacy.13,15 Another study (Saurabh et al, India) found that NSAIDs or their combinations were unnecessarily used in as many as 50% of all prescriptions.14 Similarly, in a study from Pakistan (Khan et al), polypharmacy of NSAIDs was found to be prevalent.16 More than half of the study population (55.6%) had two analgesics in their prescription while 24.4% of the patients had three to four.16 Another study (Gul et al, Pakistan) showed that majority of the prescriptions (69%) included more than one NSAID. The study reported that the use of two NSAIDs was often observed in patients with arthritis or those who experienced intense unbearable pain.26
In an Indian study, Tanwar et al reported that undergraduate medical students were widely practicing self-medication, which may increase the risk of health hazards.12 The common reasons for self-medication included: unwillingness to visit a doctor; considering pain as a mild illness; and busy schedules. It was observed that a patient receiving treatment for bronchial asthma took a combination of ibuprofen and paracetamol. The authors considered this as a significant finding because NSAIDs are known to precipitate asthma attack.12
Self-medication was reported to be common among 67% of the patients in one study (Imtiaz et al, Pakistan).10 In another study (Fatima et al, India), female medical students were commonly found practicing self-medication whereas, the female paramedical students usually preferred medical consultation or use of home remedies.25 In an Indian study, Tanwar et al reported that undergraduate medical students were widely practicing self-medication, which may increase the risk of health hazards.12 It was observed that a patient receiving treatment for bronchial asthma took a combination of ibuprofen and paracetamol. The authors considered this as a significant finding because NSAIDs are known to precipitate asthma attack.12
Discussion
This study observed that physicians in the APAC region generally have lower awareness of the potentially harmful side effects of NSAIDs. Among AEs associated with NSAIDs, GI-related AEs were most commonly reported. However, physicians seldom take an adequate history to assess a patient’s risks before prescribing NSAIDs.7 There were also differences in NSAID prescription patterns when compared by physician practice type.9 In a study of Thai orthopedic surgeons, majority of surgeons reported providing patients with side effects information related to prescription NSAID.7 In the same study, surgeons who did not provide patients with the side effects information perceived that sharing AE information with patients would likely increase their anxiety and encourage non-adherence. However, there is no evidence of association between patients receiving AE information and NSAID treatment discontinuation.7
Physicians were perceived by patients as the most reliable source of information on knowledge of NSAID side effects and contraindications followed by media and relatives/friends, according to a study conducted in a Pakistan university.21 Pharmacists were perceived as a source of NSAID information by only a quarter of the participants.21 Awareness of non-prescriptions drugs, mostly NSAIDs, was higher among urban population compared with rural population, however the use of NSAIDs was higher among rural population, according to an Indian study.19 Age was also inversely associated with awareness of NSAID use.19 A study in Thai population observed that the perception of risks and knowledge of risk factors for NSAID use was generally low but was higher among those who were provided with NSAID side effects information. This lack of awareness may lead to inappropriate use of NSAIDs. Thus, there is a need for educational programs to bridge the knowledge gap in patients, particularly in rural populations, older patients and those with low educational levels.27
Widespread use of NSAID FDCs has been reported in several APAC studies.13–16,26 Combining two NSAIDs is not likely to improve efficacy as NSAIDs act on the same pathway, however the FDCs may increase the chances of AEs and drug interaction compared with both drugs administered individually.13 Use of multiple concomitant NSAIDs was attributed to irrational prescription by physicians, lack of awareness among patients and inadequate pain relief with one NSAID.26 Self-medication of NSAIDs is also prevalent in the region with high consultation costs, shortage of time, easy accessibility to drugs and lack of awareness about complications of NSAIDs contributing to the practice.10,25 The common reasons for self-medication among students included unwillingness to visit a doctor, considering pain as a mild illness and busy schedules.12
Limitations
There are some limitations to the studies sampled in this review. Several studies have limitations due to their small sample size (Table 3). The generalizability of the results of few studies were also limited as they used convenience sampling or were single-center experience.10,11 Studies that employed survey-based methodology had varied response rates and may invariably have recall bias.7,20 Use of health insurance databases, prescription databases or patient medical records in some studies may not provide accurate diagnosis information for patients which may lead to over or underestimation of the study population. Finally, most studies did not include information on the mode of NSAID administration.
Conclusion
The prescription pattern of NSAIDs was influenced by the perceptions related to the safety of NSAIDs. Physicians are also generally unaware of contraindications to NSAID use. Risk stratification and individualization of prescription were not evident. Lack of communication regarding NSAID-associated risks and AEs between patients and prescribers may also expose patients to a higher risk for AEs associated with NSAIDs. Lack of awareness among patients, tendency to self-medicate, polypharmacy of NSAIDs further escalate these risks.
Based on the findings of this review, the following recommendations are proposed:
- Greater educational efforts to teach physicians on the risks of NSAIDs, contraindications to NSAID use, risk stratification of patients and appropriate use of NSAIDs
- A treatment algorithm to assist physicians in making a choice to use COX-2 selective NSAIDs over non-selective NSAIDs in high-risk patients
- Raise public awareness of risks and AEs of NSAIDs, risks of self-medication and avoidance of NSAID polypharmacy
Acknowledgments
The author would like to thank Dr. Sonali Dighe, Senior Director, Medical Affairs, Pfizer, for her valuable inputs during design of the study. The author would also like to thank Dr. Priyan Ratnasingham, Regional Medical Director, Medical Affairs, Pfizer, for critically reviewing the manuscript. The author acknowledges Rishabh Pandey and Prabhakar Pandey at SIRO Clinpharm for their support in conducting the systematic literature search funded by Pfizer. Editorial support was provided by Tanaya Bharatan, Manager, Scientific Communications, Pfizer, and Kaveri Sidhu, Consultant, Scientific Communications, Pfizer. Manuscript development was funded by Pfizer Ltd.
Disclosure
Dr KYH has received speaker fees from Baxter Healthcare, Mundipharma, Pfizer, Procter & Gamble, and Menarini. The content of this manuscript reflects the opinion of the author. The authors report no other conflicts of interest in this work.
References
1. Karakitsiou M, Varga Z, Kriska M, Kristova V. Risk perception of NSAIDs in hospitalized patients in Greece. Bratisl Lek Listy. 2017;118(7):427–430. doi:10.4149/BLL_2017_083
2. Sulaiman W, Seung OP, Ismail R. Patient’s knowledge and perception towards the use of non-steroidal anti-inflammatory drugs in rheumatology clinic Northern Malaysia. Oman Med J. 2012;27(6):505–508. doi:10.5001/omj.2012.121
3. Chan FK, Lanas A, Scheiman J, Berger MF, Nguyen H, Goldstein JL. Celecoxib versus omeprazole and diclofenac in patients with osteoarthritis and rheumatoid arthritis (CONDOR): a randomised trial. Lancet. 2010;376(9736):173–179. doi:10.1016/S0140-6736(10)60673-3
4. Chan FKL, Ching JYL, Tse YK, et al. Gastrointestinal safety of celecoxib versus naproxen in patients with cardiothrombotic diseases and arthritis after upper gastrointestinal bleeding (CONCERN): an industry-independent, double-blind, double-dummy, randomised trial. Lancet. 2017;389(10087):2375–2382. doi:10.1016/S0140-6736(17)30981-9
5. Nissen SE, Yeomans ND, Solomon DH, et al. Cardiovascular safety of celecoxib, naproxen, or ibuprofen for arthritis. N Engl J Med. 2016;375(26):2519–2529. doi:10.1056/NEJMoa1611593
6. MacDonald TM, Hawkey CJ, Ford I, et al. Randomized trial of switching from prescribed non-selective non-steroidal anti-inflammatory drugs to prescribed celecoxib: the Standard care vs. Celecoxib Outcome Trial (SCOT). Eur Heart J. 2017;38(23):1843–1850. doi:10.1093/eurheartj/ehw387
7. Phueanpinit P, Pongwecharak J, Sumanont S, Krska J, Jarernsiripornkul N. Physicians’ communication of risks from non-steroidal anti-inflammatory drugs and attitude towards providing adverse drug reaction information to patients. J Eval Clin Pract. 2017;23(6):1387–1394. doi:10.1111/jep.12806
8. Gupta AK, Jaiswal AK, Kumar S. Assessment of C.S.J.M. University campus students awareness and attitude towards analgesics (NSAIDs). Int J Pharm Sci Res. 2014;5(2):612–618.
9. Hong YM, Yoon KT, Heo J, et al. The prescription pattern of acetaminophen and non-steroidal anti-inflammatory drugs in patients with liver cirrhosis. J Korean Med Sci. 2016;31(10):1604–1610. doi:10.3346/jkms.2016.31.10.1604
10. Imtiaz S, Kamran SNA. Conditions, frequencies, and sociodemographic factors leading self medication practice in Sargodha area of Punjab Pakistan. J App Pharm. 2013;5(4):819–826.
11. Jagdish RK, Bhatnagar MK, Malhotra A. Study of pattern of rheumatologic and musculoskeletal disorders and their awareness among patients attending rheumatology clinic. MOJ Orthop Rheumatol. 2018;10(2):139–145.
12. Tanwar K, Mathur S. To study the pattern, efficacy and tolerability of analgesic self medication among undergraduate medical students: a questionnaire based survey. Int J Basic Clin Pharmacol. 2017;4(3):3.
13. Mudhaliar MR, Neeruganti S, Yiragamreddy PR, Mude A. Prescribing patterns of non steroidal anti inflammatory drugs (NSAIDs) in out patient department of an orthopedic specialty hospital. J Global Trends Pharm Sci. 2016;7(3):3296–3301.
14. Saurabh MK, Yadav AK, Gupta P, Singhai A, Saurabh A. Comparative study of prescribing behaviors of government doctors of teaching hospital and private practitioners in Jhalawar city (Rajasthan). J Pharm Sci Res. 2010;2(4):208–215.
15. Purkayastha A, Roy D, Tigga R, Deka D. Prescription pattern of analgesics in orthopedic out patient department at a tertiary care hospital in Silchar, Assam. World J Pharm Pharm Sci. 2016;5(10):1146–1153.
16. Khan SA, Afridi R, Afridi UK, Sadozai S. Prescribing pattern and drug–drug interactions of analgesics prescribed for pain management in a Pakistani tertiary hospital. J App Pharm. 2016;8(4):2.
17. Saurabh MK, Biswas NK, Yadav AK, Singhai A, Saurabh A. Study of prescribing habits and assessment of rational use of drugs among doctors of primary health care facilities. Asian J Pharm Clin Res. 2011;4(4):102–105.
18. Sonal Sekhar M, Adheena Mary C, Anju PG, Hamsa NA. Study on drug related hospital admissions in a tertiary care hospital in South India. Saudi Pharm J. 2011;19(4):273–278. doi:10.1016/j.jsps.2011.04.004
19. Ahmad A, Khan MU, Srikanth AB, et al. Evaluation of knowledge, attitude and practice about self-medication among rural and urban north Indian population. Int J Pharm Clin Res. 2015;7(5):326–332.
20. Chan HK, Bakri E, Tan SY, Hassali M, Saleem F, Khan TM. Prescribing patterns of celecoxib and prescribers’ perceptions among three general hospitals in Northern Malaysia. Arch Pharm Pract. 2014;5(1):28–34.
21. Chen J, Murtaza G, Nadeem N, et al. A questionnaire based survey study for the evaluation of knowledge of Pakistani University teachers regarding their awareness about ibuprofen as an over the counter analgesic. Acta Pol Pharm. 2014;71(2):337–342.
22. Choudhary AK, Nivedhitha S, Radhakrishna L, Tirumalaikolundusubrimnian P, Manicvasagam S. Perception of adverse drug reaction among doctors, nurses and pharmacists of a tertiary care rural teaching hospital. Internet J Pharmacol. 2013;12(1).
23. de Leon JR, Espinosa E. Pattern of pain management practices of Filipino surgeons. Oncology. 2008;74(Suppl 1):40–45.
24. Nguyen D, Banerjee N, Abdelaziz D, Lewis JH. Trainees’ attitudes and preferences towards the use of over the counter analgesics in patients with chronic liver disease. Adv Pharmacoepidemiol Drug Saf. 2014;3:167.
25. Fatima A, Mamatha KR, Ambika B, Rajarathna K. Self-medication practice in primary dysmenorrhea among medical and paramedical students - A cross-sectional questionnaire study. Natl J Physiol Pharm Pharmacol. 2017;7(5):458–463. doi:10.5455/njppp.2017.7.1233424122016
26. Gul S, Ayub M. Prevalence of prescribing pattern of more than one NSAID in Pakistan. J Sci Innov Res. 2014;3(2):148–154.
27. Phueanpinit P, Pongwecharak J, Krska J, Jarernsiripornkul N. Knowledge and perceptions of the risks of non-steroidal anti-inflammatory drugs among orthopaedic patients in Thailand. Int J Clin Pharm. 2016;38(5):1269–1276. doi:10.1007/s11096-016-0363-9
28. Ravinthar K, Warrier ED, Roy A. Analgesic drugs in dentistry- a cross-sectional study among dentists in a private dental college. Int J Pharm Sci Res. 2016;7(12):5092–5098.
29. Antappan AP, Micheal BP, Thelappilly MA, et al. Prescription pattern of NSAIDS and the prevalence of NSAID-induced gastrointestinal risk factors of orthopaedic patients. Indian J Pharm Biol Res. 2017;5(3):17–25. doi:10.30750/ijpbr.5.3.3
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
