Back to Journals » Patient Preference and Adherence » Volume 14
Perceived Self-Efficacy and Associated Factors Among Adult Patients with Type 2 Diabetes Mellitus at Public Hospitals of Western Ethiopia, 2020
Authors Oluma A , Abadiga M , Mosisa G , Fekadu G , Turi E
Received 6 August 2020
Accepted for publication 3 September 2020
Published 24 September 2020 Volume 2020:14 Pages 1689—1698
DOI https://doi.org/10.2147/PPA.S275887
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Adugna Oluma,1 Muktar Abadiga,1 Getu Mosisa,1 Ginenus Fekadu,2 Ebisa Turi3
1School of Nursing and Midwifery, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 2Department of Pharmacy, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 3Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Correspondence: Adugna Oluma Tel +251917814582
Email [email protected]
Background: Diabetes Mellitus is a chronic disease and can be self-managed using five treatment approaches, including education, medical nutrition therapy, physical exercise, pharmacological intervention, and blood sugar monitoring. Improvement of patient compliance and self-efficacy are critical points that impact the self-care behavior in patients with type two diabetes mellitus in order to limit the morbidity and promote glycemic control. Therefore, the present study successfully assesses the effect of perceived self-efficacy and associated factors among patients with diabetes mellitus at public hospitals of western Ethiopia.
Methods: The cross-sectional study design was employed on a sample of 423 diabetic patients. A systematic random sampling method was employed. An interviewer-administered structured questionnaire was used. The data entered into Epi data version 3.1 and exported into Statistical Package for the Social Sciences window version 24 for analysis. All variables significant at p < 0.25 in bivariate were entered into multivariate analysis. The multivariable logistic regressions were used to determine factors associated with perceived self-efficacy by considering adjusted odds ratio at CI 95% and the significance level was set at p < 0.05.
Results: Out of 423 participants sampled, 398 participated in the study giving a response rate of 94.1%. The level of perceived good self-efficacy among diabetes patients was 52.5%. Being married (AOR=1.611, 95% CI = 1.003, 2.587), home blood glucose test (AOR=3.359, 95% CI = 1.912,5.903), doing exercise (AOR=11.412, 95% CI = 2.488,52.346), having good appetite (AOR=2.587, 95% CI = 1.454,4.606), having special diet (AOR=4.902, 95% CI= 1.202, 19.992), and good self-care behavior (AOR=10.320, 95% CI= 5.657, 18.824) were significantly associated with good self-efficacy.
Conclusion: The level of perceived self-efficacy was high. Home blood glucose tests, good self-care behavior, married, doing exercise, good appetite, having a special diet were significantly associated with high perceived self-efficacy. The national policymaker focused on patients’ behavioral change to develop perceived self-efficacy for confidently managing the disease.
Keywords: diabetes mellitus, glycemic control, self-efficacy, Ethiopia
Introduction
Diabetes mellitus is a chronic disease caused by inherited and/or acquired deficiency in production and/or ineffective insulin produced by the pancreas. Globally, an estimated 463 adults (20–79 years) were living with diabetes; by 2045, these numbers rose to 700 million. Approximately about 79% of adults with diabetes were living in low- and middle-income countries. In Ethiopia, the prevalence was dramatically increasing from 3.8% to 5.2%.1,2 Diabetes mellitus (DM) is a serious global public health problem that affects the whole life of the people in terms of their biological, psychological, and social effects. The cost of paying for diabetes is rising dramatically due to complications ranging from an increased risk of heart attacks, strokes, and amputations to blindness and kidney damage.3,4 Effective control of devastating diabetes complication needs behavioral changes that require self-efficacy and self-care management.5 The conception of self-efficacy is based on Bandura’s social cognitive theory, which describes the interactions of behavioral, personal, and environmental factors. Thus, self-efficacy is a people’s beliefs about their capabilities to produce designated levels of performance in terms of patients’ feel, think, and motivation toward physical therapies and related activities. In relating to the glycemic control, self-efficacy refers to one’s belief that he/she can plan and accomplish behavior change, the belief that I can do it and the perceived ability to adhere to the diabetes care regimen.6,7 Another diabetes-related study also interpreted self-efficacy in terms of three dimensions which includes patients’ perceived ability to obtain social support, manage stress, be self-motivating, and make diabetes-related decisions; patients’ perceived ability to identify aspects for caring for diabetes that they are dissatisfied with and their ability to determine when they are ready to change their diabetes self-care plan and patients’ perceived ability to set realistic goals and reach them by overcoming the barriers to achieving their goals.8 The measurement of self-efficacy was a critical concept in chronic disease management including diabetes mellitus. Self-efficacy is an essential factor influencing self-care behavior in patients with type 2 diabetes. Perceived self-efficacy helped plan patient educational programs for targeting diabetic self-management. It also helps to predict the health outcomes including hospital admissions, and quality of life of diabetic patients.9 The study indicated that self-efficacy has a significant effect on diabetes self-treatment. It leads to metabolic control and improved ability to self-treatment. Patients with good self-efficacy have 20 times the chance of undergoing diabetes treatment as compared to that had poor self-efficacy.10
The study revealed that self-efficacy plays a pivotal role in diabetes by assisting individuals to carry out daily tasks to take control of their condition. It has been used to predict behaviors and interventional plans related to diet and nutrient intakes and its outcomes in terms of glycemic and weight control. Therefore, better understandings of self-efficacy are integrated into planning self-management programs and facilitate patient empowerment for improved diabetes-related behaviors and outcomes.11
Another study showed that the risk of type 2 diabetes increases with age particularly occurring in patients older than 55 years. Type 2 diabetes also has a psychological impact that causes diabetic complications which relatively increased hospitalized 1.5–3 times than patients without the disease. The major problem in diabetes management is the patient’s attitude towards their illness due to the difference in their ideas and beliefs. Patients who gain knowledge about self-care disease management do not always implement the desired behavioral changes that require important counseling skills and need careful attention.12
Furthermore, the study indicated that self-efficacy in patients with diabetes was the first step to develop a specific individual intervention. The measurement of self-efficacy was used as diagnostic tools for diabetes patients that helps medical professionals to get information that needs about patient readiness to involve in changing behavior by diabetic education. Diabetes education was the most important task in diabetes management that minimizes the symptoms. Self-efficacy applies for both newly diagnosed patient as well as the patient who have long diagnosed which involves verbal persuasion that influences how someone act and behave and got suggestion that they can resolve their problems.13
Previous studies revealed self-efficacy is associated with numerous factors including satisfaction, better adaptation, reduced depression, proper control of diabetes, diverse diabetes management behaviors, selected nutrients, exercise, medications, blood sugar control, problem-solving, social environment support, eating patterns, reduced fat intake, and self-care behaviors. The requirement of perceived self-efficacy for diabetic patients is a baseline for routine diabetes self-management leads to good glycemic control and subsequently reduces the risk of diabetic complications.12,14–18
However, in the context of Ethiopia, there was no study conducted regarding perceived self-efficacy among patients with chronic diseases specifically diabetes. Thus, this study will fill this existing gap and contribute to minimizing the adverse effect of prolonged uses of medications through customizing self-arranged routine diabetes management. Therefore, the aim of this was to assess perceived self-efficacy and associated factors among diabetes patients attending public hospitals of western Ethiopia.
Methods
Study Setting and Population
The institutional-based cross-sectional study design was employed. The study was conducted in multi-facility-based public hospitals found in western Ethiopia from January 20-March 20, 2020. The public hospitals were selected randomly by lottery method from all public hospitals found in western Ethiopia. The four selected hospitals were Wollega university referral hospital and Nekemte specialized hospitals which are found in Nekemte town at a distance of 331km from Addis Ababa. Nekemte town has a latitude and longitude of 9º5ʹN36º33ʹE and an elevation of 2,088 meters. Ghimbi General and Nedjo General Hospital are found in West Wollega Zone. Ghimbi General Hospital has a latitude and longitude of 9º10ʹN35º50ʹE with an elevation between 1845 and 1930 meters above sea level. Nedjo General Hospital has located 518 km from Addis Ababa. The public hospitals selected for the study were serving in terms of primary, secondary, and specialized services for more than a total population of 10 million for the western part of Ethiopia.
tudy Population and Samples
First, we selected randomly four hospitals by lottery method from all public hospitals found in western Ethiopia. After the selection of hospitals, we took the sampling frame from a medical record of the diabetic patients on follow-up receiving ant diabetic medication from the chronic outpatient department of respective hospitals. Then, we calculated a constant k value and included all our potential participants from all selected hospitals. The study was conducted on a total of 1280 patients with diabetes on follow-up and receiving diabetic medications. All diabetic patients including type I and II attending selected hospitals were the source population and all the sampled patients with diabetic on follow-up receiving diabetic medication for at least six months and present during data collection period were the study population. All diabetic patients on follow-up with measured A1C ≥7.0% (53mmol/mol) were included and those taking anti-diabetic medication for less than six months were excluded from the study.
Sample Size Determination and Sampling Techniques
The sample size of the study was calculated using the formula for estimation of a single population proportion with the assumptions of 95% Confidence Level (CL), marginal error (d) of 0.05. Since there was no study conducted regarding perceived self-efficacy in Ethiopia we considered a population proportion of 0.50 (50%).
Thus, by adding a non-response rate of 10% and using the correction formula; the final sample size was 423 of people living with diabetes mellitus and treated with medication were enrolled in the study using systematic random sampling techniques from each hospital.
Data Collection Tool and Procedures
Data were collected using a structured questionnaire. Data collection tools consist of four-part questionnaires: The first part consists of demographic questions developed by investigators. Participants’ height and weight were measured as part of the physical examination. Body mass index (BMI) was classified as <18.5kg/m2 (underweight), 18.5–24.9kg/m2 (normal weight), 25–29.9 kg/m2 (overweight) and that of ≥30kg/m2 defined as obesity based on the World Health Organization criteria. The second part of the tool was a diabetes self-management questionnaire taken from the previous study originally developed by Schmitt et al19 at the Research Institute of the Diabetes Academy with Cronbach alpha of 0.856. Originally, the validated scale for diabetes self-management questionnaire has 16 items and 4 subscales: However, in the current study, three items were removed due to fewer standards of coefficients. The dimension was reduced to three components including glucose management (4 items), physical activity (4 items), and dietary control (5 items), and finally, thirteen items were used for analysis. Six items are formulated positively and the remaining seven negatively. The DSMQ has a 4-point Likert scale that starts from 0= does not apply to me, 1= applies to me to some degree, 2= applies to me to a considerable degree, and 3=applies to me very much. All negative items were reversed and the higher score indicated more effective self-care. The third part questionnaire was self-efficacy related to glycemic control collected via 8 modified questions from the diabetes mellitus self-efficacy scale (DMSES) adapted from the previous study originally developed by Wallston et al.20 The responses were rated on a 5-point Likert scale: “1=not confident, 2=not very confident, 3=confident half the time, 4=usually confident, 5=always confident”. Self-efficacy was measured by eight (8) standardized on a five-point (5) Likert scale which was 1=not confident, 2=not very confident, 3=confident half the time, 4=usually confident, and 5=always confident. Thus, respondents who answered “confident half the time and above (≥3) considered as above the mean and had good self-efficacy, and those respondents who answered less than confident half the time regarded as below the mean and had poor self-efficacy (<3)”. Cronbach’s alpha was 0.880. Finally, glycosylated hemoglobin (HbA1c) was obtained early in the morning on the same day as the measure of glycemic control using the Fast Ion Exchange Resin Separation method the value of glycated hemoglobin found on red blood cells for the previous three months. Thus, A1C levels were categorized according to American Diabetes Association into good glycemic control A1C less than 7% (53mmol/mol) and A1C over ≥7.0% (53mmol/mol) poor Glycemic control. A Close-ended interviewer-administered structured questionnaire was distributed to participants by trained data collectors. Four trained Bsc nurses’ data collectors and two supervisors were employed for consecutive two months.
Operational Definition
Self-Efficacy
“The diabetes patients’ belief and judgment of their capability of carrying out diabetes self-management activities” (Bandura, 1994) which was measured on a five-point (5) Likert scale which was 1=not confident, 2=not very confident, 3=confident half the time, 4=usually confident, and 5=always confident.
Good Self–Efficacy
Respondents who answered confident half the time and above (≥3) considered as above the mean and had good self-efficacy
Poor Self–Efficacy
Those respondents who answered less than confident half the time regarded as below the mean (<3) and had poor self-efficacy.
Self-Care Behaviors
Defined as activities performed by diabetic patients including healthy eating plan, exercise, self-glucose monitoring, and diabetes medication and/or insulin intake.
Poor Self-Care Behaviors
Those patients’ self-care behaviors scored less than 50th percentile of self-care behavior scores.
Good Self Self-Care Behaviors
Those patients’ self-care behaviors scored more than 50th percentile of self-care behavior scores.
Reliability of the Instruments
The Sampling adequacy was checked by the Kaiser Meyer Olkin test. For all scales, confirmatory factor analysis was performed to know the adequacy of all instruments (accepted standard >0.5). The reliability determined by the coefficient of loading factors by using the principal component method, Varimax rotation with Kaiser Normalization at Eigenvalue >1. The intraclass correlation coefficient was used for testing the reliability of scales. Some items were reduced based on the value of the intraclass correlation coefficient using the principal component method, Varimax rotation with Kaiser Normalization at Eigenvalue >1. Factor analysis for Diabetes self-management tools with Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.83 (DF=105, p=00). The rotated component matrix showed three dimensions (1, 2 and 3). The total variance explained for the first dimension was 23.44%, the 2nd dimension 39.28% and the third dimension was 57.69%. The overall Cronbach’s alpha of the tool was =0.86. Confirmatory factor analysis of the self-efficacy scale with Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.86 (DF=28, p=00). The rotated component matrix of loading factors resulted in two dimensions (1 and 2) with total variance explained for the 1st and 2nd dimensions (35.76% 68.76%) respectively. The overall Cronbach’s alpha =0.88.
Data Quality Control
All questionnaires adopted in the English language translated into the local language Afan Oromo and then re-translated back into English by experts. A pretest was conducted on 5% of the questionnaire on diabetic patients at Shambu hospital that was outside the actual study setting before data collection. The training was given one day for both data collectors and supervisors. Data were cleaned, coded, and checked for consistency and completeness. A consistency was checked by a double-entry method to improve the quality of the data.
Data Processing and Analysis
Data were cleaned, edited, coded, and entered into Epi data version 3.1 and was exported to SPSS windows version 24 for analysis. Descriptive statistics including, percentage, ratios, frequency distribution, mean and standard deviation, and pie chart was used to describe the data. Normalization of the data was checked using Hosmer and Lemeshow test and chi-square to know the homogeneity of variables. All variables were significant at p-value <0.25 in the bivariable were entered in multivariate regression analysis. Backward stepwise goodness of fit was used to ascertain the suitable variables in multiple logistic regression analysis. Finally, multivariate logistic regression analysis with adjusted ORs, CI at 95%, and the significance level was set at p <0.05.
Results
Socio-Demographic Characteristics of Participants
Out of 423 participants sampled, 398 participated in the study giving a response rate of 94.1%. More than half 210 (52.8%) of the participants were male with a median age of 45 (±15.876SD). The majority of the participants 168 (42.2%) were aged above 50 years followed by 40–49 (24.1%) years. Concerning their ethnicity, the majority of the participants 355 (89.2%) were Oromo with language speaker 327 (82.2%) Afan Oromo. Nearly half 189 (47.5%) of the respondents were protestant followers followed by 134 (33.7%) were an orthodox believer. Concerning marital status, about 308 (77.4%) were married. Moreover, concerning the educational status majority of the respondents were 109 (27.4%) college/university and about 97 (24.4%) had no formal education. With regard to their occupation, most of them 169 (42.5%) were employees, and about 246 (61.8%) urban indwellers (Table 1).
 |
Table 1 Distribution of Socio-Demographic Characteristics of Diabetes Patients Attending Public Hospitals of Western Ethiopia (N=398) |
Clinical Characteristics of Participants
The study results showed most of the participants (55.78%) were smokers. The majority (76.1%) of the respondents had no family history of diabetes. More than half (53.8%) of patients have suffered from diabetes mellitus for less than five years. Of the total of respondents, 68.1% of them had no diabetes-related complications (hypertension, neuropathy, diabetic coma, foot gangrene) and the remaining 31.9% had diabetes-related complications. Approximately three-fourth (74.1%) of the respondents did physical activity per week and nearly half (51.0%) of them test their blood glucose by glucometer at home. The majority (39.4%) of the respondents were overweight (BMI=25–29.9) and they reported that they experienced increased body weight (51.8%). The participants reported that about seventy percent (70.1%) of them had no special diet and 29.9% of them had a self-arranged special diet. The majority of the patients 285 (71.6%) had been taking a combination of oral hypoglycemic agents and insulin and the remaining had been taking insulin injection and non-pharmacological treatment (23.4% and 5.0%, respectively) (Table 2).
 |
Table 2 Proportion of Clinical Characteristics of Diabetes Patients Attending Public Hospitals of Western Ethiopia (N=398) |
Prevalence of Perceived Self-Efficacy and Self-Care Behavior Among Diabetes Patients
The level of perceived good self-efficacy among diabetes patients was 52.5% with a mean and standard deviation of 27.10±6.41. The level of self-care behavior was classified as poor, fair, and good using less than 25th, 25th-75th, and more than the 75th percentile of their possible scores. Thus, of 398 respondents the prevalence of good self-care behavior 20.4% (n=81), fair self-care behavior 51.0% (n=203), and 28.6% (n=114) were poor self-care behavior (Figures 1 and 2).
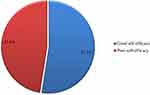 |
Figure 1 The level of perceived self-efficacy among diabetes patients attending public hospitals of west Ethiopia, 2020. |
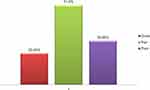 |
Figure 2 The practice of self-care behaviors among diabetes patients attending public hospitals of west Ethiopia, 2020. |
Bivariable Logistic Regression Analysis of Factors Associated with Perceived Self-Efficacy
In logistic regression good self-care behavior, unmarried, exercise per weeks, home blood glucose test, decreased body weight body overweight, good appetite, having dietary restriction, having a special diet, having food planning, being nonsmoker, were significantly associated variables with good perceived self-efficacy at p<0.25 (Table 3)
 |
Table 3 Bivariable Logistic Registration Analysis of Factors Associated with Perceived Self-Efficacy Among Diabetes Patients Attending Public Hospitals of Western Ethiopia, 2020 |
Multivariable Logistic Regression Analysis of Factors Associated with Perceived Self-Efficacy
All variables significant at bivariable level entered into multivariable logistic regression found six significantly associated variables with perceived self-efficacy including home blood glucose test, being unmarried, good self-care behavior, having a good appetite, doing exercise, having a special diet. Being unmarried was less likely to have high perceived self-efficacy compared to married (AOR=0.308, 95% CI = 0.160, 0.594). Concerning home blood glucose test participants who test their blood glucose were three times more likely to have high perceived self-efficacy than those who did not test their blood glucose at home (AOR=3.359, 95% CI = 1.912,5.903). With regards to doing exercise were eleven times more likely to have high perceived self-efficacy compared to participants who did not do exercise (AOR=11.412, 95% CI = 2.488,52.346). Regarding the description of participants, appetite participants who had a good appetite were three times more likely to have high perceived self-efficacy compared to participants who had poor appetite (AOR=2.587, 95% CI = 1.454,4.606). Concerning having special diet participants who had special diet were five times more likely to have high perceived self-efficacy compared to participants who did not have special diet recommendation (AOR=4.902, 95% CI= 1.202, 19.992). The study result also revealed that participants who had good self-care behavior were ten times more likely to have good perceived self-efficacy than participants who had poor self-care behaviors (AOR=10.320, 95% CI= 5.657, 18.824) (Table 4).
 |
Table 4 Multivariable Logistic Registration Analysis of Factors Associated with Perceived Self-Efficacy Among Diabetes Patients Attending Public Hospitals of Western Ethiopia, 2020 |
Discussion
This study aimed to determine perceived self-efficacy and its underlying factors among diabetes patients on follow up receiving anti-diabetic medications. The level of good perceived self-efficacy in this study was 52.5%. This finding was almost relatively similar to the result of a study conducted in Indonesia showing that patients who have good self-efficacy (52.4%) as well as poor self-efficacy about 47.6%. However, this finding was relatively lower than the result of a study conducted in Saudi Arabia about 53% of participants reported good self-efficacy. This similarity might justify the fact that individual confidence in self-managing diabetes through nutrition, exercise, and close monitoring of blood glucose is a common strategy across the globe.20,21
The study revealed that self-care behavior is associated with perceived self-efficacy considering the joint effect of other variables in the logistic regression model. Having good self-care behavior increased the odds of perceived self-efficacy ten times compared to poor self-care behaviors (AOR=10.320, 95% CI= 5.657, 18.824). This finding was similar to a study conducted in Iran which explained that diabetes self – management has a prominent role in perceived self-efficacy which reported that 31.3% variance of diabetes self-care behavioral intention and 11.4% of variance due to diabetes self-care.22
The finding of this study showed that participants who tested their blood glucose at home were three times more likely to have high perceived self-efficacy than those who did not test their blood glucose (AOR=3.359, 95% CI = 1.912,5.903). This finding was similar to the study done in Israel which showed self-efficacy was found to be associated with a home glucose monitoring, and lower HbA1c in young people with Type I diabetes as revealed in Pearson’s correlations (r=0.47, P < 0.01). This similarity justifies the fact that diabetic patients engaging in the self intervention of home blood glucose measuring enhance their level of confidence to reduce their blood glucose to recommended targets.23
The study result also illustrated the relationship between perceived self-efficacy and exercising physical activity per week that diabetes patients who exercise were eleven times more likely to have high perceived self-efficacy compared to participants who did not do exercise (AOR=11.412, 95% CI = 2.488,52.346). This finding was higher than the study conducted by Peyman et al in Iran which revealed patients who had self-efficacy were an important predictor of physical activity in the study, subjects showed a significantly positive correlation between physical activity and perceived self-efficacy (r= 0.176, p <0.005). This finding was also comparable with the result of the study conducted by Albargawi et al showed self-efficacy had a significant, positive correlation with participants’ adherence to exercise (r=0.491; p < 0.006). This difference might relate to a variation in economic status and national health policy guidelines for diabetes treatment modality across the countries.21,24
In this current study respondents who had a special diet were found to be a significant predictor of perceived self-efficacy among diabetes patients. Thus, participants who had a special diet were five times more likely to have high perceived self-efficacy compared to participants who did not have a special diet recommendation (AOR=4.902, 95% CI= 1.202, 19.992). This finding was similar to a study conducted in Staffordshire University England that perceived self-efficacy was associated with self-reported adherence to dietary self-care activities (r = 0.21, p < 0.05) and as well dietary self-efficacy and perceived spousal support were associated with dietary behaviors among Type 2 diabetes patients. This similar correlation related to participants’ level of confidence enhances the level of dietary adherence for controlling blood glucose levels.25,26
Limitations and Strengths of the Study
The Strength of the Study
- The concept was novel and directed the need for further scientific implications.
- The data collection tools were anonymously structured.
Limitations of the Study
- Since it was cross-sectional no comparison of cause and effect relationship.
- There was recall bias.
Study Implications
The findings of the study found important parameters related to perceived self-efficacy including self-care behaviour, blood glucose test, doing regular physical activities per week, and adherence to dietary restriction. Theses parameters were important focus areas for implications of this study in order to integrating in national health policy making and practicing individually for self-monitoring blood glucose and reduce potential complication.
Conclusion
The overall prevalence of good perceived self-efficacy was high. Home blood glucose, good self-care behavior, unmarried, exercise per week, good appetite, having dietary restriction, having a special diet were significantly associated variables with high perceived self-efficacy. Therefore, it is better if the national health policymaker focused on management modality that engages patients’ behavior change to develop good perceived self-efficacy for their better confidently managing their blood glucose level.
Abbreviations
ADA, American Diabetes Association; AOR, adjusted odds ratio; BMI, body mass index; DM, diabetes mellitus; DMSES, Diabetes Mellitus Self-efficacy Scale; DSMQ, diabetes self-management questionnaire; HIV, human immunodeficiency virus; SD, standard deviation; SMBG, self-monitoring of blood glucose.
Data Sharing Statement
The data used during this study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The study was reviewed and approved by the Institutional Review Boards of Wollega university Ethical review board. The purpose of the study was explained to the medical director and staff of the hospital and permission was obtained. We conducted the study in accordance with the Declaration of Helsinki by including basic principles of ensuring the study subject’s privacy, risk and benefit, conducted by trained professionals, true informed consent obtained, and even we allowed the right to withdraw if the study participants requested. No minors were involved in the study and the consent was obtained from the participants themselves. Moreover, the confidentiality of the information was assured.
Acknowledgments
We would like to acknowledge Wollega University for financial support. We also would like to acknowledge Wollega public hospitals. We are also grateful to the study participants who voluntarily agreed to be interviewed and participated in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research work was funded by Wollega University. The funder did not participate in designing and data collection, analysis, writing, and submission of the article for publication.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. International Diabetes Federation. IDF diabetes Atlas – 9th edition. 2019. Available from: www.idf.org/diabetesatlas.
2. Bishu KG, Jenkins C, Yebyo HG, Atsbha M, Wubayehu T, Gebregziabher M. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obes Med. 2019;15(1):100132. doi:10.1016/j.obmed.2019.100132
3. Mom O, Hentinen M. Adherence to self-care and glycemic control among people with insulin dependent diabetes mellitus. J Adv Nurs. 2001;34(1):780–786. doi:10.1046/j.1365-2648.2001.01808.x
4. Khattab M, Khader YS, Al-Khawaldeh A, et al. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complications. 2010;24(2):84–89. doi:10.1016/j.jdiacomp.2008.12.008
5. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12(1):14. doi:10.1186/2251-6581-12-14
6. Beckerle CM, Lavin MA. Association of self-efficacy and self-care with glycemic control in diabetes. Diabetes Spectr. 2013;26(3):172–178. doi:10.2337/diaspect.26.3.172
7. Liu T. A concept analysis of self-efficacy among Chinese elderly with diabetes mellitus. Nurs Forum. 2012;47(4):226–235. doi:10.1111/j.1744-6198.2012.00282.x
8. Nelson KM, Mcfarland L, Reiber G. Factors influencing disease self-management among veterans with diabetes and poor glycemic control. J Gen Intern Med. 2007;22(4):442–447. doi:10.1007/s11606-006-0053-8
9. Frei A, Svarin A, Stey SC, Puhan AM. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations – a systematic review. Health Qual Life Outcomes. 2009;86(7):1475–1477.
10. Sigurdardottir AK. Self care in diabetes: model of factors affecting self care. J Clin Nurs. 2005;14(2):301–314. doi:10.1111/j.1365-2702.2004.01043.x
11. Funnel MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(1):123–127. doi:10.2337/diaclin.22.3.123
12. Sharoni SKA, Vivienne S-F. Self-efficacy and self-care behavior of Malaysian patients with type 2 diabetes. Nurs Health Sci. 2012;14(1):38–45. doi:10.1111/j.1442-2018.2011.00658.x
13. Mishali M, Omer H, Heymann AD. The importance of measuring self-efficacy in patients with diabetes. Fam Pract. 2011;28(1):82–87.
14. Tol A, Sharifirad G, Eslami A, et al. Self efficacy: an efficient functional concept in type 2 diabetes control. Health Syst Res. 2012;8(1):339–347.
15. Naik AD, Palmer N, Petersen NJ, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics. Arch Intern Med. 2011;171(1):453–459. doi:10.1001/archinternmed.2011.70
16. Miller CK, Gutschall M. A randomized trial about glycemic index and glycemic load improves outcomes among adults with type 2 diabetes. Health Educ Behav. 2009;36(1):615–626. doi:10.1177/1090198108317598
17. Latimer L, Walker LO, Kim S, et al. Self-efficacy scale for weight loss among multi-ethnic women of lower income: a psychometric evaluation. J Nutr Educ Behav. 2011;43(1):279–283. doi:10.1016/j.jneb.2010.09.007
18. Wichi N, Mnatzaganian G, Courtney M, Schulz P, Johnson M. Randomized controlled trial of a family-oriented self-management program to improve self-efficacy, glycemic control and quality of life among Thai individuals with type 2 diabetes. Diabetes Res Clin Pract. 2017;40(1):37–48. doi:10.1016/j.diabres.2016.11.013
19. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. Diabetes self management questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycemic control. Health Qual Life Outcomes. 2013;11(2):138–143. doi:10.1186/1477-7525-11-138
20. Wallston K, Rothman R, Cherrington A. Psychometric properties of the perceived diabetes self-management scale (PDSMS). J Behav Med. 2007;30(1):395–401. doi:10.1007/s10865-007-9110-y
21. Peyman N, Esmaily H, Taghipour A, Mahdizadeh M. Using of social cognitive theory: predictors of physical activity among women with diabetes type 2. J Res Health. 2013;3(2):345–354.
22. Anna Kurnia S.Kep, HeriNugroho HS, NikenSafitriDyanKusumaningrum S.Kep. Relation between self efficacy and quality of life domain in patients with type 2 diabetes mellitus. IOSR-JNH. 2017;6:32–37.
23. Didarloo A, Shojaeizadeh D, RG Asl, Habibzadeh H, Niknami S, Pourali R. Prediction of self-management behavior among Iranian women with type 2 diabetes: application of the theory of reasoned action along with self-efficacy. Iran Red Crescent Med J. 2012;14(2):86.
24. Albargawi M, Snethen J, Gannass AA, Kelber S. Perception of persons with type 2 diabetes mellitus. Int J Nurs Sci. 2016;3(1):39–44.
25. Mishali M, Omer H, Heymann AD. The importance of measuring self-efficacy in patients with diabetes. Fam Pract. 2010;24(1):610–615. doi:10.1093/fampra/cmm057
26. Senteal C, Nouwen A, Gingras J, Gosselin M, Audet J. Motivation and dietary self-care in adults with diabetes. J Psychosom Res. 2000;19(5):352–357.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.