Back to Journals » International Medical Case Reports Journal » Volume 10
Pediatric endogenous Haemophilus influenzae endophthalmitis with presumed hyposplenism
Authors Haruta M , Yoshida Y, Yamakawa R
Received 30 September 2016
Accepted for publication 9 November 2016
Published 4 January 2017 Volume 2017:10 Pages 7—9
DOI https://doi.org/10.2147/IMCRJ.S123524
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Masatoshi Haruta, Yumiko Yoshida, Ryoji Yamakawa
Department of Ophthalmology, Kurume University School of Medicine, Kurume, Japan
Background: Endogenous bacterial endophthalmitis is a rare but potentially devastating intraocular infection that can have severe sight-threatening complications. Most patients with endogenous bacterial endophthalmitis have underlying infectious conditions, such as diabetes or malignancy, which predispose them to infection.
Case report: A 1-year-old girl presented with cloudiness of the right eye. Ocular examination showed a cloudy cornea in the right eye with conjunctival injection and hypopyon. The intraocular pressure was 43 mmHg, and the fundus could not be visualized. She had an 8-day history of fever, and cerebrospinal fluid analysis showed typical findings of bacterial meningitis. She was clinically diagnosed with bacterial meningitis and endophthalmitis in the right eye and was treated with intravenous, topical, and intravitreal antibiotics and vitrectomy. Haemophilus influenzae was isolated from the blood and cerebrospinal fluid cultures, but not from the aqueous and vitreous cultures. Four months later, her pediatrician diagnosed Streptococcus pneumoniae meningitis, but she had no clinical signs of endophthalmitis. Seven years after the initial presentation, the best-corrected visual acuity was 20/40 in the right eye.
Discussion: Endophthalmitis caused by H. influenzae is generally associated with poor visual outcomes; however, the patient in the current case responded well to the treatment. The patient had recurrent bacterial meningitis caused by H. influenzae and S. pneumoniae within a 4-month period. Magnetic resonance imaging was performed to search for underlying infectious causes and revealed that the patient had an extremely small spleen for her age. Because the spleen is critical for clearing encapsulated bacteria such as H. influenzae or S. pneumoniae, we speculated that hyposplenism led to the bloodstream infection of H. influenza and then endogenous endophthalmitis in the right eye.
Keywords: intravitreal antibiotics, meningitis, Streptococcus pneumoniae, vitrectomy
Introduction
Endogenous bacterial endophthalmitis is a rare but potentially devastating intraocular infection that can have severe sight-threatening complications.1–3 Most patients with endogenous bacterial endophthalmitis have underlying infectious conditions, such as diabetes or malignancy, which predispose them to infection.
We report the case of a 1-year-old girl who developed Haemophilus influenzae meningitis with endogenous endophthalmitis in the right eye. Although endophthalmitis caused by H. influenzae is generally associated with poor visual outcomes, the patient responded well to the treatment. Magnetic resonance imaging showed the presence of an extremely small spleen considering the patient’s age. Because the spleen is critical for clearing encapsulated bacteria such as H. influenzae or Streptococcus pneumoniae, we speculate that hyposplenism led to the bloodstream infection of H. influenzae and then endogenous endophthalmitis in the right eye.
Case report
A 1-year-old girl was referred to Kurume University Hospital because her mother noticed cloudiness of the right eye 8 hours earlier. Examination showed a cloudy cornea in the right eye with severe conjunctival injection and hypopyon. The intraocular pressure was 43 mmHg, and the fundus could not be visualized. Her left eye was normal.
The patient had an 8-day history of fever and was treated with oral cefditoren pivoxil for 5 days followed by oral azithromycin for 3 days before admission. She seemed uncomfortable. Her temperature was 38.3°C, pulse 128 beats per minute, blood pressure 118/70 mmHg, and respiratory rate 48 breaths per minute. The white cell count was 45,000 per cubic millimeter, and the C-reactive protein value was 15.4 mg/dL. Cerebrospinal fluid analysis showed typical findings of bacterial meningitis, including a white cell count of 6,400 per cubic millimeter, a protein level of 148 mg/dL, and a glucose level of 24 mg/dL.
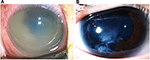
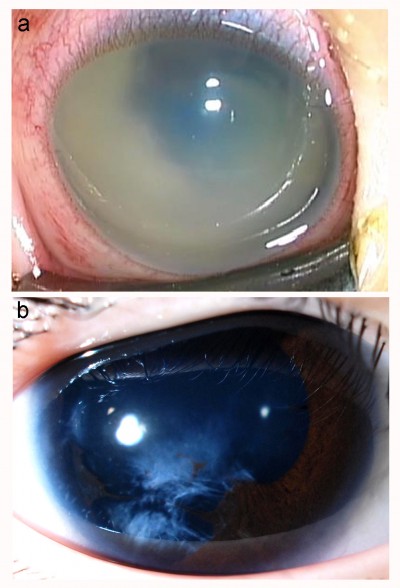
The patient was clinically diagnosed with bacterial meningitis and endophthalmitis in the right eye. Her mother was informed of the treatment and provided written informed consent for this case report. She was treated with intravenous meropenem and vancomycin for 7 days and then with meropenem alone for another 8 days. She also received topical gatifloxacin and cefmenoxime hydrochloride eye drops and received an injection of intravitreal imipenem/cilastatin and vancomycin on the third day (Figure 1A). Although the hypopyon in the right eye improved after the intravitreal injection, B-scan ultrasonography showed increased vitreous opacities in the right eye. She underwent a 25-gauge vitrectomy and received an additional intravitreal injection of imipenem/cilastatin and ceftazidime on the sixth day. During vitrectomy, the retina seemed to be intact and no tamponade was used. The appearance of the right eye returned to normal 1 month after the vitrectomy. H. influenzae was isolated from the blood and cerebrospinal fluid cultures but not from the aqueous and vitreous cultures.
Four months later, her pediatrician diagnosed S. pneumoniae meningitis, but she had no clinical signs of endophthalmitis. She was treated with intravenous panipenem/betamipron for 7 days and then with ampicillin for another 7 days. Magnetic resonance imaging showed a 1 cm soft-tissue density that was thought to be a hypoplastic spleen in the normal location of the spleen (Figure 2). After her infection, she received H. influenzae type b conjugate vaccine which was introduced in Japan in 2008. Seven years after the initial presentation, her best-corrected visual acuity was 20/40 and her intraocular pressure was 17 mmHg in the right eye (Figure 1B).
  | Figure 2 (A) Coronal and (B) axial abdominal magnetic resonance images show a 1 cm soft-tissue density (arrows) that was thought to be a hypoplastic spleen in the normal location of the spleen. |
The Ethical Committee of Kurume University approved this retrospective case report.
Discussion
Bacterial endophthalmitis can be classified as either exogenous or endogenous, depending on the route of infection. Exogenous bacterial endophthalmitis usually occurs after ocular surgery or penetrating ocular trauma. However, endogenous bacterial endophthalmitis occurs when bacteria enter the bloodstream from distant foci of infections and then cross the blood–ocular barrier into the eye. In the current case, the diagnosis of endogenous H. influenzae endophthalmitis was made because H. influenzae was isolated from the blood and cerebrospinal fluid cultures and the patient had no history of ocular surgery or trauma.
In general, endophthalmitis caused by H. influenzae is associated with poor visual outcomes despite prompt treatment with appropriate antibiotics and often with vitrectomy. Yoder et al reported that 6 of 16 eyes with endophthalmitis caused by H. influenzae had a final visual acuity of no light perception.4 Gupta et al reported that infection with H. influenzae was associated strongly with a final outcome of enucleation or evisceration.5 However, in studies that focused only on endogenous H. influenzae endophthalmitis involving children younger than 3 years of age, the prognosis with antibiotic treatment was more favorable, and enucleation was necessary in only one of seven eyes.1,6,7 The patient in the current case also responded well to the antibiotic treatment and vitrectomy despite infection with H. influenzae.
The pathogens that most commonly cause sepsis in patients who have undergone splenectomy are H. influenza and S. pneumoniae.8 The current patient had recurrent bacterial meningitis caused by H. influenzae and S. pneumoniae within a 4-month period. Magnetic resonance imaging was performed to search for underlying infectious causes and also revealed that the patient had an extremely small spleen for her age. If a small spleen is functionally impaired, a patient might be more susceptible to an infection with encapsulated bacteria, such as H. influenzae or S. pneumoniae. Therefore, in the current patient, we speculated that hyposplenism led to the bloodstream infection of H. influenza and subsequent endogenous endophthalmitis in the right eye.
Diagnosing endogenous bacterial endophthalmitis remains challenging. Jackson et al reported that the rate of diagnostic delay was as high as 26%.2,3 Due to its rarity, endogenous bacterial endophthalmitis in the pediatric population is often unsuspected and misdiagnosed.9,10 In addition, it is usually difficult to perform a detailed clinical examination on uncooperative patients. Furthermore, young children may not be able to recognize or verbalize their symptoms, making early diagnosis even more difficult. Nevertheless, early diagnosis and prompt treatment of pediatric endogenous bacterial endophthalmitis, which may lead to improved visual outcomes, should always be pursued.
Acknowledgment
The authors thank Lynda Charters for her contribution to the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Greenwald MJ, Wohl LG, Sell CH. Metastatic bacterial endophthalmitis: a contemporary reappraisal. Surv Ophthalmol. 1986;31(2):81–101. | ||
Jackson TL, Eykyn SJ, Graham EM, Stanford MR. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol. 2003;48(4):403–423. | ||
Jackson TL, Paraskevopoulos T, Georgalas I. Systematic review of 342 cases of endogenous bacterial endophthalmitis. Surv Ophthalmol. 2014;59(6):627–635. | ||
Yoder DM, Scott IU, Flynn HW, Miller D. Endophthalmitis caused by Haemophilus influenzae. Ophthalmology. 2004;111(11):2023–2026. | ||
Gupta A, Orlans HO, Hornby SJ, Bowler IC. Microbiology and visual outcomes of culture-positive bacterial endophthalmitis in Oxford, UK. Graefes Arch Clin Exp Ophthalmol. 2014;252(11):1825–1830. | ||
Sastry RV, Baker CJ. Endophthalmitis associated with Haemophilus influenzae type b bacteremia and meningitis. Am J Dis Child. 1979; | ||
Taylor JR, Cibis GW, Hamtil LW. Endophthalmitis complicating Haemophilus influenzae type B meningitis. Arch Ophthalmol. 1980;98(2): | ||
Rubin LG, Schaffner W. Clinical practice. Care of the asplenic patient. N Engl J Med. 2014;371(4):349–356. | ||
Khan S, Athwal L, Zarbin M, Bhagat N. Pediatric infectious endophthalmitis: a review. J Pediatr Ophthalmol Strabismus. 2014;51(3):140–153. | ||
Chaudhry IA, Shamsi FA, Al-Dhibi H, Khan AO. Pediatric endogenous bacterial endophthalmitis: case report and review of the literature. J AAPOS. 2006;10(5):491–493. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.