Back to Journals » Patient Preference and Adherence » Volume 15
Patients’ Involvement in Decision-Making During Healthcare in a Developing Country: A Cross-Sectional Study
Authors Nuwagaba J , Olum R , Bananyiza A, Wekha G , Rutayisire M, Agaba KK, Chekwech G, Nabukalu J, Nanyonjo GG, Namagembe R , Nantongo S, Lubwama M, Besigye I, Kiguli S
Received 19 January 2021
Accepted for publication 25 March 2021
Published 26 May 2021 Volume 2021:15 Pages 1133—1140
DOI https://doi.org/10.2147/PPA.S302784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Julius Nuwagaba,1 Ronald Olum,1 Ali Bananyiza,1 Godfrey Wekha,1 Meddy Rutayisire,1 Keneth Kato Agaba,1 Gaudencia Chekwech,1 Jalidah Nabukalu,1 Genevieve Gloria Nanyonjo,2 Robinah Namagembe,3 Sylvia Nantongo,3 Margaret Lubwama,4 Innocent Besigye,5 Sarah Kiguli6
1School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda; 2School of Public Health, College of Health Sciences, Makerere University, Kampala, Uganda; 3School of Health Sciences, College of Health Sciences, Makerere University, Kampala, Uganda; 4Department of Microbiology, School of Biomedical Science, College of Health Sciences, Makerere University, Kampala, Uganda; 5Department of Family Medicine, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda; 6Department of Pediatrics & Child Health, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda
Correspondence: Julius Nuwagaba
School of Medicine, Makerere University College of Health Sciences, P.O. Box 7072, Kampala, Uganda
Tel +256782774038
Email [email protected]
Purpose: Patient autonomy and participation have a significant impact on patient satisfaction and compliance with treatment. We aimed to establish and describe the level of shared decision-making (SDM) among the patients in a developing country. Uganda is a low resource country with a 2019 GDP of 35.17 billion US dollars. In some regions, over 60% of Ugandans live below the national poverty line and most of them depend on the underfunded health care system.
Methods: A cross-sectional, quantitative study was carried out among the outpatients attending Kisenyi Health center IV, Kampala, Uganda. An interviewer-administered questionnaire with a 5-point Likert scale was used to assess patients’ SDM. All statistical analysis was performed using STATA 15 software.
Results: A total of 326 patients participated in this study. Majority of the participants were females (n=241, 73.9%) and aged 18– 35 years (n=218, 66.9%). Only 22 (7%) of the participants knew the name of their consulting doctor. Most of the participants, 84% were given enough time to narrate their symptoms. Overall, only 11.3% (n=37) of the participants had adequately participated in SDM. The overall mean score of participation in SDM was 2.7 (SD:0.8). Participants who knew the name of their consulting doctor were approximately 11 times more likely to participate in SDM (OR: 10.7, 95% CI: 4.2– 27.0, P< 0.0001).
Conclusion: The majority of patients attending Kisenyi Health Center IV did not adequately participate in SDM. Continued medical education should be organized for healthcare professionals to promote SDM.
Keywords: shared decision making, patient involvement, information, participation
Introduction
Shared decision making (SDM) is defined as a process where clinicians collaboratively help patients to reach evidence-informed and value-congruent medical decisions.1 SDM involves clinicians and patients sharing the best available evidence when faced with the task of making decisions, and where patients are supported to consider options, to achieve informed preferences.2 For proper patient involvement, a patient must be a stakeholder in decision making including expressing opinions and ideas about the different treatment options.3 SDM is at the heart of patient-centered care and is a crucial ethical component that has the potential for improved quality and safety in health care.6 For better health outcomes, a physician (or other healthcare professional) should inform patients and engage them in SDM which will lead to the provision of appropriate and cost-effective care and ultimately leads to patient satisfaction.5–8 Evidence shows that low patient involvement in decision making in health centers increases not only treatment cost but also the risk of health care complications.9 SDM involves three key steps; making sure the patients know the reasonably available options, providing detailed information on the available options, and lastly considering patients’ preferences and considering what is best.4
In recent years, patients’ involvement in decision-making has become very essential in the strengthening of health systems and health service delivery in many countries around the world.5 Better patients’ experience, satisfaction, cost-effectiveness, and quality of care have been reported in countries where patients are fully engaged in decision making.5 However, SDM remains a challenge in the provision of patient-centered health care in developing countries.5,6 Lack of an SDM culture, healthcare worker paternalism, lack of continuity of care, low patients’ literary, and patients’ low interest in decision making coupled with trust in health workers affect SDM in developing countries.10 The low health worker-to-patient ratio in developing countries also makes the feasibility of SDM challenging with regards to consultation time.10,11 In Uganda, despite low awareness of patients’ rights, Uganda’s patient charter provides for the right of patients to make informed decisions regarding their healthcare.12,13 However, there is limited data on patient involvement in decision-making. A study done among women with breast cancer at Mulago National Referral Hospital, Uganda showed that most of them (80%) believed not satisfied with their participation in treatment selection.11 Similar findings have been reported in rural health facilities in Eastern Uganda.14,15 Patients’ participation in decision-making is reported to be high among Ugandan patients undergoing surgical procedures though there are concerns of inadequate provision of information.16 However, there is a lack of information regarding patients’ participation in shared decision-making at primary level health facilities including Health Center IVs which manage most of the patients in Uganda. In this study, we aimed to establish and describe the existing level of SDM among patients attending general consultations at Kisenyi Health Center IV in order to guide interventions for improving patient-centered care.
Methods and Materials
Study Design
A cross-sectional study.
Study Setting
The study was carried out at Kisenyi Health Centre IV, located on Mwanga II Road, in one of the biggest slum areas in Kampala, Uganda’s capital city. Kisenyi HC IV is a public urban health facility intended to serve about 100,000 people within the health sub-district, and it is administered by Kampala Capital City Authority (KCCA) (the regulatory body for Uganda’s capital city). The health facility provides a wide range of inpatient, outpatient, and emergency care services. They also provide maternal and child health services including emergency cesarean sections. It serves a population consisting of traders within the central business district and slum occupants from the nearby areas.
Study Population
The study population consisted of patients seeking care from the outpatient department (OPD) of Kisenyi Health center IV during the period of study. All patients were eligible to participate in the study irrespective of their reason for health care visit or disease condition that they were being treated for.
Selection Criteria
All adult patients aged 18 years and above seeking healthcare from the outpatient department at Kisenyi Health Center IV between December 2019 and January 22,020, were eligible for the study.
Sample Size
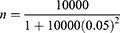
The sample size was calculated using Yamane’s formula for population survey.17
N denotes the population size and e indicates the level of precision. Kisenyi HC IV receives about 500 patients daily, with about 10,000 patients received in a month. Data collection was anticipated to take one month.
Using a monthly population size of 10,000 patients and the level of precision at 5%,
Therefore, the total sample size was 385 participants.
Sampling Procedure
Patients attending the outpatient department were consecutively approached and recruited after informed consent until the required sample size was reached.
Data Collection
A semi-structured interviewer-administered questionnaire designed in English and translated to Luganda, the commonly spoken local language in Kampala was used to collect the data. Patient-exit interviews were conducted after the patients had completed a consultation with the doctors, performed the required tests, received medications or treatment, and were leaving for home. Data was collected by members of the research team who had undergone training on the study protocol including research ethics.
Study Variables
The independent variables included sociodemographic characteristics like age, sex, highest level of education, marital status, religion, and knowledge of the doctor’s names. The dependent variable was participation in SDM.
Questionnaire Development
The questionnaire consisted of two parts.
- Part A consisted of 6 questions on the social and demographic characteristics of the participant.
- Part B included 9 questions on the various aspects of SDM. These comprised 1 question whether patients received adequate consultation time, 5 questions on adequate information, and 3 questions on decision making. A 5-point Likert scale was used with responses; strongly agree, agree, neutral, disagree, and strongly disagree. The questions were adopted from the SDM-Q-9 tool for patients and modified by the authors to suit the local context.18 The Cronbach’s alpha score of the 9 items was 0.9 indicating strong internal consistency. The 15-item questionnaire was pretested among 10 patients at Kisenyi HC IV who did not take part in the actual study. The questionnaire is provided as a Supplementary File.
Data Management and Analysis
After checking the questionnaires for completion, data was entered using EpiCollect 5 software.19 It was then exported to Microsoft Excel 2016 for cleaning and coding. All analyses were performed using STATA 15 (StataCorp LLC, College Station, Texas, United States). Categorical data were presented as frequencies and percentages, and numerical data presented as mean or medians. The 9-item 5-point Likert scale on SDM was coded and scored as follows- strongly agree with 5, agree with a 4, neutral with a 3, disagree with a 2, and strongly disagree with a 1. The mean score for the 9 items was then calculated for each participant, with a maximum of 5 and a minimum of 1. Using Bloom’s cutoff, patient’s participation in SDM was categorized as adequate (mean score ≥4), or poor (mean score <4).20 Association of patients’ adequate participation in SDM was assessed using the chi-square test and binary logistic regression. A P<0.05 was considered statistically significant.
Ethical Considerations
The study was reviewed and approved by Makerere University School of Health Sciences Research and Ethics Committee, Reference No. 2019–054. Permission to carry out the study was sought from the Office of the Director of Public Health and Environment at Kampala Capital City Authority (KCCA) and the In-Charge of Kisenyi Health Center IV. The study was conducted according to the Declaration of Helsinki. Enrolment of participants into the study was voluntary after obtaining written informed consent. Patients’ privacy and confidentiality were maintained at all times.
Results
Socio-Demographic Characteristics of Study Participants
Table 1 summarizes the socio-demographic characteristics of the participants. A total of 326 respondents with a median age of 30 years (18 to 70) participated in this study (response rate of 85%). Most of the participants were young adults aged 18 to 35 (n=218, 66.9%), female (n=241, 73.9%), and had attained secondary education as the highest level (n=147, 45.1%). Only 22 patients (7%) knew the name of the doctor they had talked to during the clinical consultation while 304 (93%) did not.
 |
Table 1 Social and Demographic Characteristics of the Participants |
Responses of Study Participants to Questions on SDM
Table 2 describes the responses of the patients to the nine questions on SDM. The majority of the patients agreed that the doctor gave them enough time to narrate all their symptoms (84%, mean score: 4.1 ± 1.0). Except for explaining the required tests and treatment options (Q4), more than half of the patients disagreed on the other aspects (Q2, Q3, Q5-Q9) of SDM. Up to 242 (74%) patients disagreed on weighing investigation and treatment options together with the doctor and (n=244, 75%) of the patients disagreed on making the decision together with the doctor on the treatment. The patients generally disagreed on statements Q2 to Q9 with mean scores below 3.0 (Table 2). These were assessing if patients were given adequate information and involved in decision making.
 |
Table 2 Responses of Patients at Kisenyi Health Center IV to Statements on Aspects of Shared Decision Making |
Shared Decision Making Among Study Participants
Only 37 patients (11.3%) had adequately participated in SDM during their consultation (Table 3). The overall mean score for participation in shared decision-making was 2.7 (SD:0.8) indicating poor participation (Table 3). At chi-square tests, only knowledge of the doctor’s name was significantly associated with adequate participation in SDM (P<0.0001). A binary logistic regression showed that patients who knew the doctor’s name were approximately 11 times more likely to have adequate participation in SDM (OR: 10.7, 95% CI: 4.2–27.0, P<0.0001).
 |
Table 3 Mean Scores and Factors Associated with Participation in Shared Decision Making Among Patients at Kisenyi Health Center IV |
Discussion
The objective of this study was to describe the level of SDM among the patients attending the outpatient department at Kisenyi Health Center IV, Kampala, Uganda to improve patient care and satisfaction. To the best of our knowledge, this is the first study in Uganda, and East Africa to investigate SDM in the general patient population. From our study, only 11.3% of the participants participated adequately in SDM. This complements findings from other developing countries that have reported low patients’ participation in decision making during their treatment.21–23 In Uganda, a study among breast cancer patients showed that 80% of them were not given a chance to participate in the selection of their treatment options.11 However, higher participation in SDM has been reported in some developed countries.24 In a clinic in Hong Kong, over 57% of the patients were involved in SDM.25
Our study agreed with previous studies that patient-related factors like social demographic characteristics affect participation in SDM.5,26 Literacy and level of education play an important role in patients’ involvement in SDM. Patients who have attained a higher level of education have a better comprehension of the medical information provided by healthcare workers.5 In our study, participation in shared decision-making increased with an increase in the level of education, although this was not significant. In a study in Tanzania, healthcare workers admitted that patients with low education status found it harder to comprehend medical information, and therefore making it difficult to engage them in SDM.23 In a qualitative study in Australia, participants with a higher level of education perceived getting involved as a shared responsibility with healthcare providers throughout the process of decision making. This included verifying information provided by the healthcare providers as well as discovering treatment options outside those presented to them by the health workers. On the other side, patients with low education however regarded their participation in decision making as agreeing and consenting to the recommendations of the healthcare provider.27 Although Uganda has a high adult literacy rate, that is, the ability to read and write (76.53%),28 this may not reflect actual comprehension which may be a possible reason for the low SDM recorded in the study.
A patient-doctor relationship is essential in the process of SDM. This relationship relies on good communication between the doctor and the patient.29 Effective communication begins with the initiation of a good rapport between the doctor and the patient. This includes components like salutations and self-introduction by the healthcare provider. Uganda’s patient charter states that a patient has a right to be cared for by a known healthcare worker.30 From our study, only 7% of the patients were aware of the doctor’s name, and these patients were more likely to have good participation in SDM. A low level of patient-doctor relationship should have led to low participation in SDM. Therefore, the patient-doctor relationship remains a keystone of patient care.31
In our study, the majority of the patients disagreed on questions regarding the provision of adequate information by the doctor. This could also have contributed to the low participation in decision making since doctors have to provide information (including information about the diagnosis, nature, goal, and seriousness of the treatment, risk of treatment, and other treatment options) to patients so they can make free and informed decisions.32 This process could have been impeded by limited consultation time coupled with a large number of patients who seek care in public health facilities like Kisenyi Health Center IV, hence the low participation in SDM. A publication by NHS England showed that patients require to be given information by the health care professionals and hence feel cared for if they participate in decision making.33 The quality of the information transfer between the physician and the patient leads to increased participation in SDM processes.34 On a positive aspect, the majority of the participants were given enough time to report their signs and symptoms to the doctors.
Levinson and colleagues showed that patients who visit a regular doctor were less likely to participate in decision making.35 The prolonged care by the same doctor fosters a good patient-doctor relationship leading to increased trust in the healthcare worker by the patients. However, a recent study among psychiatric patients (bipolar disorder and schizophrenia) suggested that patients were less likely to have compulsory admission against their decision if they had a regular doctor.36 Psychiatric patients with a regular doctor tend to have regular follow-ups by the psychiatrist subsequently leading to fewer psychiatric symptoms requiring compulsory admissions despite the reduced ability to participate in shared decision making. No study has been undertaken in Uganda to assess the impact of being attended regularly by the same doctor on patients’ decision-making. However, we believe Ugandan patients may tend to leave decision-making to their regular healthcare provider due to the trust and confidence built over time.
SDM is very important in addressing the patient’s perspective.37 Patient’s involvement in decision-making during their healthcare has far-reaching benefits in the overall outcome of treatment.5 This is the first study in Uganda to report SDM among outpatients in a primary health facility. The high response rate of the study also improves the generalizability of the study findings. However, the study has some limitations. Some factors that may affect decision-making like occupation or source of income and wealth index were not assessed. A qualitative study is necessary to explore these factors. Besides, we utilized a modified questionnaire that has not been validated in this setting. However, it had a strong internal consistency of 0.9. This is also a cross-sectional study that does not show a true cause and effect relationship but rather associations.38
Conclusion and Recommendations
There was poor patient involvement in decision making as only about 1 in 10 of the participants participated in decision making. There is a need to encourage doctors to practice a two-way form of communication where they provide information to patients and ask for a patient understanding of the illness and treatment process. This can be achieved through teaching sessions in medical school as well as Continued Medical Education sessions at the health centers and hospitals. It is further important for the health care system to establish feasible ways to improve patient participation in various health facilities.
Data Sharing Statement
The research data for this study is available on Figshare https://figshare.com/articles/Data_set_Patients_involvement_in_decision-making_at_Kisenyi_Health_Center_IV_Kampala_Central_Uganda/12519971.
Acknowledgments
We thank the patients at Kisenyi Health Center IV for taking part in the study. We also extend our gratitude to the Health Professions Education and Training for Strengthening the Health Systems and Services in Uganda (HEPI-SHSSU) team for the undergraduate research fellowship program and the guidance. We also thank Dr. Lillian Nabukeera Mukisa for guiding us through the research process. We also thank the administration at Kampala Capital City Authority and Kisenyi Health Center IV for authorizing us to collect data at the health Center.
Funding
This research was supported by the Fogarty International Center of the National Institutes of Health, US Department of State’s Office of the U.S, Global AIDS Coordinator and Health Diplomacy (S/GAC), and President’s Emergency Plan for AIDS Relief (PEPFAR) under award number 1R25TW011213. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure
Dr Keneth Kato Agaba reports grants from The Fogarty International Center of the National Institutes of Health, US Department of State’s Office of the U.S, Global AIDS Coordinator and Health Diplomacy (S/GAC), grants from President’s Emergency Plan for AIDS Relief (PEPFAR) under award number 1R25TW011213, during the conduct of the study. Dr Ali Bananyiza reports grants from Health Professional Education Partnership initiative, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Grad R, Légaré F, Bell NR, et al. Shared decision making in preventive health care: what it is; what it is not. Can Fam Physician. 2017;63(9):682–684.
2. Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341(oct14 2):c5146. doi:10.1136/bmj.c5146
3. Thompson AG. The meaning of patient involvement and participation in health care consultations: a taxonomy. Soc Sci Med. 2007;64(6):1297–1310. doi:10.1016/j.socscimed.2006.11.002
4. William G. Shared decision-making. Healthc Q. 2009;12(sp):e186–e190. doi:10.12927/hcq.2009.20947
5. Vahdat S, Hamzehgardeshi L, Hessam S, et al. Patient involvement in health care decision making: a review. Iran Red Crescent Med J. 2014;16(1):e12454. doi:10.5812/ircmj.12454
6. Towle A, Godolphin W, Greenhalgh T, Gambrill J. Framework for teaching and learning informed shared decision making. BMJ. 1999;319(7212):766–771. doi:10.1136/bmj.319.7212.766
7. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–312. doi:10.1016/j.pec.2005.06.010
8. Henley L, Benatar SR, Robertson BA, et al. Informed consent–a survey of doctors’ practices in South Africa. S Afr Med J. 1995;85(12):1273–1278.
9. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi:10.1007/s11606-012-2077-6
10. Tong WT, Lee YK, Ng CJ, et al. Factors influencing implementation of a patient decision aid in a developing country: an Exploratory Study. Implement Sci. 2017;12(1):40. doi:10.1186/s13012-017-0569-9
11. Batte A, Odoi-Adome R. Patient involvement in treatment decision making among women with breast cancer: Creating person centered and equitable health services system. 2006.
12. Ministry of Health. Uganda Patients’ Charter. Assurance DoQ, editor. Kampala, Uganda; 2009.
13. Kagoya HR, Kibuule D, Mitonga-Kabwebwe H, et al. Awareness of, responsiveness to and practice of patients’ rights at Uganda’s national referral hospital. Afr J Prim Health Care Fam Med. 2013;5(1):491. doi:10.4102/phcfm.v5i1.491
14. Waweru E, Sarkar NDP, Ssengooba F, et al. Stakeholder perceptions on patient-centered care at primary health care level in rural eastern Uganda: a qualitative inquiry. PLoS One. 2019;14(8):e0221649. doi:10.1371/journal.pone.0221649
15. Waweru E, Smekens T, Orne-Gliemann J, et al. Patient perspectives on interpersonal aspects of healthcare and patient-centeredness at primary health facilities: a mixed methods study in rural Eastern Uganda. PLoS One. 2020;15(7):e0236524. doi:10.1371/journal.pone.0236524
16. Ochieng J, Buwembo W, Munabi I, et al. Informed consent in clinical practice: patients’ experiences and perspectives following surgery. BMC Res Notes. 2015;8(1):765. doi:10.1186/s13104-015-1754-z
17. Yamane T. Research Methods: Determination of Sample Size. 1967.
18. Härter M, Scholl I. The 9-item Shared Decision Making Questionnaire (SDM-Q-9); University Medical Center, Hamburg-Eppendorf, Germany. Available from: http://www.patient-als-partner.de/index.php?article_id=20&clang=2/.
19. Aanensen DM, Huntley DM, Feil EJ, et al. EpiCollect: linking smartphones to web applications for epidemiology, ecology and community data collection. PLoS One. 2009;4(9):e6968. doi:10.1371/journal.pone.0006968
20. Kaliyaperumal K. Guideline for conducting a Knowledge, Attitude and Practice (KAP) Study. AECS Illumination. 2004;4:7–9.
21. Ambigapathy R, Chia YC, Ng CJ. Patient involvement in decision-making: a Cross-Sectional Study in a Malaysian primary care clinic. BMJ Open. 2016;6(1):e010063. doi:10.1136/bmjopen-2015-010063
22. Sam S, Sharma R, Corp N, Igwesi-Chidobe C, Babatunde OO. Shared decision making in musculoskeletal pain consultations in low- and middle-income countries: a systematic review. Int Health. 2020;12(5):455–471. doi:10.1093/inthealth/ihz077
23. Vedasto O, Morris B, Furia FF. Shared decision-making between health care providers and patients at a tertiary hospital diabetic clinic in Tanzania. BMC Health Serv Res. 2021;21(1). doi:10.1186/s12913-020-06041-4
24. Lu C, Li X, Yang K. Trends in shared decision-making studies from 2009 to 2018: a bibliometric analysis. Front Public Health. 2019;7:384. doi:10.3389/fpubh.2019.00384
25. Xu RH, Wong EL. Involvement in shared decision-making for patients in public specialist outpatient clinics in Hong Kong. Patient Prefer Adherence. 2017;11:505–512. doi:10.2147/PPA.S126316
26. Davis RE, Jacklin R, Sevdalis N, et al. Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expect. 2007;10(3):259–267. doi:10.1111/j.1369-7625.2007.00450.x
27. Smith SK, Dixon A, Trevena L, et al. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc Sci Med. 2009;69(12):1805–1812. doi:10.1016/j.socscimed.2009.09.056
28. Uganda - Literacy rate 2018, Literacy rate increase in Uganda. Available from: https://countryeconomy.com/demography/literacy-rate/uganda. Accessed April 2, 2021.
29. Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38–43.
30. Republic of Uganda MoH, Department of Quality Assurance. Patients’ Charter. 2009.
31. Dorr Goold S, Lipkin M
32. Educaloi. The duties of doctors towards patients. Available from: https://www.educaloi.qc.ca/en/capsules/duties-doctors-towards-patients.
33. NHS. Involving people in their own health and care: statutory guidance for clinical commissioning groups and NHS England; 2017. Available from: https://www.england.nhs.uk/wp-content/uploads/2017/04/ppp-involving-people-health-care-guidance.pdf.
34. Veilleux S, Noiseux I, Lachapelle N, et al. Patients’ perception of their involvement in shared treatment decision making: key factors in the treatment of inflammatory bowel disease. Patient Educ Couns. 2018;101(2):331–339. doi:10.1016/j.pec.2017.07.028
35. Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. J Gen Intern Med. 2005;20(6):531–535. doi:10.1111/j.1525-1497.2005.04101.x
36. Morán-Sánchez I, Bernal-López MA, Pérez-Cárceles MD. Compulsory admissions and preferences in decision-making in patients with psychotic and bipolar disorders. Soc Psychiatry Psychiatr Epidemiol. 2020;55(5):571–580. doi:10.1007/s00127-019-01809-4
37. Brand PL, Stiggelbout AM. Effective follow-up consultations: the importance of patient-centered communication and shared decision making. Paediatr Respir Rev. 2013;14(4):224–228. doi:10.1016/j.prrv.2013.01.002
38. Solem RC. Limitation of a Cross-Sectional Study. Am J Orthod Dentofacial Orthop. 2015;148(2):148. Letter to the Editor. doi:10.1016/j.ajodo.2015.05.006
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.