Back to Journals » Patient Preference and Adherence » Volume 14
Patient Treatment Preferences for Heart Failure Medications: A Mixed Methods Study
Authors Trinkley KE , Kahn MG , Allen LA , Haugen H, Kroehl ME, Lin CT , Malone DC, Matlock DD
Received 10 August 2020
Accepted for publication 16 October 2020
Published 10 November 2020 Volume 2020:14 Pages 2225—2230
DOI https://doi.org/10.2147/PPA.S276328
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Katy E Trinkley,1– 4 Michael G Kahn,5 Larry A Allen,2,4 Heather Haugen,6 Miranda E Kroehl,7 Chen-Tan Lin,2,3 Daniel C Malone,8 Daniel D Matlock2,4,9
1Department of Clinical Pharmacy, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, CO, USA; 2Department of Medicine, University of Colorado School of Medicine, Aurora, CO, USA; 3Clinical Informatics, University of Colorado Health, Aurora, CO, USA; 4Adult and Child Consortium for Outcomes Research and Delivery Science, Aurora, CO, USA; 5Section of Informatics and Data Science, Department of Pediatrics, University of Colorado School of Medicine, Aurora, CO, USA; 6University of Colorado, Colorado Clinical and Translational Sciences Institute (CCTSI), Aurora, CO, USA; 7Charter Communications Corporation, Greenwood Village, CO, USA; 8Department of Pharmacotherapy, University of Utah Skaggs College of Pharmacy, Salt Lake City, UT, USA; 9VA Eastern Colorado Geriatric Research Education and Clinical Center, Aurora, CO, USA
Correspondence: Katy E Trinkley
University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, 12850 E Montview Blvd., Mail Stop C238, Aurora, CO 80045, USA
Tel +1-303-724-6563
Fax +1-303-724-0979
Email [email protected]
Introduction: Consideration of patient preferences for guideline-directed medical therapies (GDMT) for heart failure with reduced ejection fraction (HFrEF) may help improve major gaps in prescribing and adherence. This study aimed to identify the range and relative priority of factors influencing patients’ decisions to take HFrEF medications.
Materials and Methods: This was a convergent mixed methods study of patients with HFrEF. Focus groups were conducted to identify a list of factors followed by individuals rating and ranking the influence of each factor on their decision to take a medication. Using thematic analysis, we summarized preferences into categories.
Results: Two focus groups with 13 participants reported 22 factors. Of the factors, “keeping you alive” was most commonly ranked in the top three (seven participants), followed by “communication and understanding” (six participants). Factors were summarized into six categories (listed in order of patient-reported influence): 1) demonstrated improvements in quality of life and longevity, 2) decreased risk of hospitalization, 3) opportunity for shared decision-making and trust in provider, 4) absence of adverse events, 5) affordability, and 6) convenience of taking and absence of interference with daily life.
Conclusion: Patients prioritize treatment benefits and being informed more than risks, cost and inconvenience of taking HFrEF medications.
Keywords: heart failure, treatment preferences, medication preferences, patient preferences
Introduction
Guideline directed management and therapy (GDMT) for heart failure and reduced ejection fraction (HFrEF) is complex. Clinicians managing HFrEF must consider multiple medications initiated in a strategic sequence and achieve specific target doses while balancing patient intolerance in addition to multiple devices and co-management of common comorbidities including diabetes, coronary artery disease and atrial fibrillation.1 Further, consideration of patient preferences and values for treatment is critical to optimizing treatment adherence and patient outcomes. Although clinicians and GDMT are aligned with or attuned to patient preferences in some clinical contexts,2,3 this is not always true.4
Others have evaluated HF treatment preferences among patients at the end of life or with advanced HF,4–7 or by focusing on preferences related to the desired outcomes of treatments.6,8,9 Given patients with more severe illness often prioritize treatments that prolong survival differently than healthier patients,10 there is a need to understand preferences across the spectrum of HF severity. There is also limited information regarding holistic factors that influence patients’ decisions to initiate and adhere to HF treatments, such as cost, convenience, or potential for adverse effects. HFrEF imposes a constellation of unique burdens on patients and it is necessary to understand their treatment preferences and factors influencing their decisions to take HFrEF medications. Therefore, the purpose of this study is to conduct a mixed methods evaluation of factors influencing patients’ decisions to take HFrEF medications.
Materials and Methods
Focus groups of adult patients with HFrEF were conducted. The purpose of the focus groups was to identify the range and relative priority of factors influencing patients’ decisions to take HFrEF medications (eg, clinical benefits, medication cost, dosing complexity).
Participants and Recruitment
Patients with established clinical relationships with a study investigator were invited to participate by phone. Purposeful sampling was used with consideration of patient demographics, disease severity and practice settings. Patients with preserved ejection fraction were excluded given differences in guideline recommended treatments. All patients received care from a primary care or outpatient cardiology practice within one academic medical center. To achieve thematic saturation, up to three sessions with 5 to 12 participants were planned.11
Data Collection
Focus groups were led by a trained investigator (KET) following a semi-structured interview guide.12 Field notes were taken to identify key issues and record salient influential factors. During a break in the focus group, the field notes were used to create a survey of influencing factors. The survey was unique for each focus group session in which the factors reflected the terminology used by the participants. When the break concluded, participants used the survey to individually rate and rank the factors. Each item on the survey was associated with a 10-point Likert scale (1=not important; 10=most important).
The patient focus groups consisted of four sequential components: 1) overview of purpose, 2) semi-structured group discussion to determine the range of factors, 3) independent rating of the importance of each factor from the survey, and 4) individuals ranking the top three most influential factors on the survey.
Analysis
Patient ratings and rankings of influential factors were summarized into categories using a thematic analysis. The factors were manually categorized into major themes iteratively using topic coding. Topic coding included general categorization of the factors into themes with some connection.13 Throughout topic coding, interpretation or analytical conclusions were applied to assess the meaning of factors.13 Likert scale scores were summarized descriptively. Participant rankings were also weighted to account for the number of participants in the focus group at which the factor was discussed. Weightings of the participant rankings were calculated by first assigning points to each participant’s response and then dividing the sum of points by the number of participants who considered each factor. To assign points, 3 points were given to a ranking of 1 (top #1 priority), 2 points to a ranking of 2, 1 point to a ranking of 3 and 0 points to no ranking (did not identify as one of the top three priorities). This study was conducted in accordance with the Declaration of Helsinki. It was approved by the Colorado Multiple Institutional Review Board and participants provided informed consent.
Results
There was general consensus regarding influential factors after two focus groups, with five and eight patients. The mean age of participants was 67 years (range 43 to 88). With one exception, all participants were male. All patients were non-Hispanic, 10 were Caucasian and 3 were Black. Most reported a cardiologist managed their HFrEF. All patients were insured. Nearly half of patients reported HFrEF symptoms at rest and most reported some discussion with their healthcare provider prior to starting HFrEF medications. Table 1 describes patient characteristics.
 |
Table 1 Patient Demographics and Reported Characteristics (n=13) |
Treatment Preferences
During the open-ended discussion, participants reported 22 factors that influenced their decision to take HFrEF medications (Table 2). These factors reflect terminology used by participants and include “information and statistics” and “getting in shape.” While participants may have used different terminology in the two focus groups, the overarching sentiment of the conversations was consistent. These 22 factors were thematically summarized into six overarching categories: 1) opportunity for shared/informed decision making and trust in provider, 2) demonstrated improvements in quality of life and longevity, 3) decreased risk of hospitalization, 4) absence of adverse events, 5) affordability, and 6) convenience of taking and absence of interference with daily life.
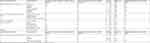 |
Table 2 Range of Patient-Reported Treatment Preferences and Degree of Influence on Decision to Take Heart Failure Medications |
Individual Rating of Factors and Categories of Influential Factors
Based on Likert scale responses, three categories were perceived to be most influential to participants’ decision to take HFrEF medications: 1) demonstrated improvements in quality of life and longevity, 2) decreased risk of hospitalization, 3) opportunity for shared decision-making and trust in provider. With the exception of “demonstrated improvements in quality of life and longevity,” the median Likert scale responses for the individual factors comprising these three categories were ten out of ten. Table 2 describes the factors that comprise these six categories and the influence of each factor on their decision to take HFrEF medications.
Individual Rankings of Factors
When asked to individually rank the factors that influenced their decision to take a HFrEF medication, “communication and understanding” and “that it works” had the most participants (three) indicating it was their top #1 priority. “Keeping you alive” was most commonly ranked in the top three (seven participants), followed by “communication and understanding” (six responses) and “that it works” (five participants). Ten factors were not selected by any participant to be in the top three priorities. Based on weighted ranking, “communication and understanding” was ranked higher than “keeping you alive” (1.15 versus 1.0, respectively). Table 2 describes participant rankings of the factors.
Discussion
In this study, patient-reported factors influencing their decisions to take HFrEF medications aligned well with GDMT recommendations. Patients prioritized medications’ benefits (morbidity, mortality, hospitalization, quality of life) over potential adverse effects. GDMT for HFrEF directly maximizes these treatment outcomes.1 Patients also reported affordability and convenience of taking medications as less important compared to being informed and positive treatment benefits. Such prioritization of positive treatment outcomes over other factors is also seen in other patient populations, notably those with cancer.2,3,14 Prior studies evaluating patient HFrEF treatment preferences focus on treatment outcomes and do not directly evaluate other factors such as adverse effects or cost.6,8,9 In our study, four patients ranked “cost or insurance coverage” or “number of times you take meds daily” among the top three priorities that impacts their decision to take a HFrEF medication (none ranked #1). These findings suggest patients are willing to risk the possibility of discomfort (adverse effects) and inconvenience in their daily lives and even pay more for a medication if there are potential treatment benefits such as quality of life and longevity.
While these findings may be generalized to similar patient populations, the results should not supplant patient-centered decisions. In fact, our findings reinforce the need to involve the patient in the decision. Patients expressed a strong desire to be informed about the benefits and risks and to be part of the decision to start a HFrEF medication. It is unclear from this research how much benefit must exist to offset the potential or actual adverse effects of HFrEF medications or other forms of HFrEF treatment such as devices. More research is needed to understand these value judgments and trade-offs, which can help inform shared decision-making discussions between patients and clinicians. Further, for shared decision-making conversations, especially for more complex therapies such as devices, there are existing frameworks that may help facilitate.15
There are several limitations to our study. First, the findings from this study may not be representative of all patients, such as those in rural or inner-city settings. Further, all focus group participants were insured and insurance coverage may have biased their stated importance of cost on their decision to start a HFrEF medication. We also did not directly evaluate patient perspectives when weighing short-term symptoms against longer-term potential benefit, which is central to GDMT for HFrEF. It is also possible that patient education and knowledge related to their HFrEF diagnosis could impact patient-stated factors that influence their decisions related to medications; however, we did not collect data related to participant education or knowledge of their diagnosis. A strength of this study is patients were included irrespective of their life expectancy or severity of HFrEF.
Conclusions
Patients prioritize treatment benefits more than risks, cost and inconvenience of taking HFrEF medications. Patients also prioritize shared decision making and being informed about their medications. These findings can be used to guide shared decision-making conversations or by health systems designing interventions to optimize care for populations of patients with HFrEF.
Abbreviations
GDMT, guideline-directed management and therapy; HFrEF, heart failure and reduced ejection fraction.
Ethics
This study was conducted in accordance with the Declaration of Helsinki.
Funding
Supported in part by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535 and by NHLBI K12 Training Grant Number K12HL137862.
Disclosure
Dr Larry A Allen reports personal fees from Novartis, Amgen, and Cytokinetics, during the conduct of the study; personal fees from Abbott and Boston Scientific, grants from NIH and PCORI, and grants and personal fees from American Heart Association, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure. J Am Coll Cardiol. 2017;70(6):776–803. doi:10.1016/j.jacc.2017.04.025
2. Mühlbacher AC, Nübling M. Analysis of physicians’ perspectives versus patients’ preferences: direct assessment and discrete choice experiments in the therapy of multiple myeloma. Eur J Health Econ. 2011;12(3):193–203. doi:10.1007/s10198-010-0218-6
3. Meads DM, O’Dwyer JL, Hulme CT, Chintakayala P, Vinall-Collier K, Bennett MI. Patient preferences for pain management in advanced cancer: results from a discrete choice experiment. Patient. 2017;10(5):643–651. doi:10.1007/s40271-017-0236-x
4. Brunner-la Rocca H-P, Rickenbacher P, Muzzarelli S, et al. End-of-life preferences of elderly patients with chronic heart failure. Eur Heart J. 2012;33(6):752–759. doi:10.1093/eurheartj/ehr404
5. MacIver J, Rao V, Delgado DH, et al. Choices: a study of preferences for end-of-life treatments in patients with advanced heart failure. J Hear Lung Transplant. 2008;27(9):1002–1007. doi:10.1016/j.healun.2008.06.002
6. Stevenson LW, Hellkamp AS, Leier CV, et al. Changing preferences for survival after hospitalization with advanced heart failure. J Am Coll Cardiol. 2008;52(21):1702–1708. doi:10.1016/j.jacc.2008.08.028
7. Klindtworth K, Oster P, Hager K, Krause O, Bleidorn J, Schneider N. Living with and dying from advanced heart failure: understanding the needs of older patients at the end of life. BMC Geriatr. 2015;15(1):125. doi:10.1186/s12877-015-0124-y
8. Hauber AB, Obi EN, Price MA, Whalley D, Chang C-L. Quantifying the relative importance to patients of avoiding symptoms and outcomes of heart failure. Curr Med Res Opin. 2017;33(11):2027–2038. doi:10.1080/03007995.2017.1355782
9. Stanek EJ, Oates MB, McGhan WF, Denofrio D, Loh E. Preferences for treatment outcomes in patients with heart failure: symptoms versus survival. J Card Fail. 2000;6(3):225–232. doi:10.1054/jcaf.2000.9503
10. Winter L, Parker B. Current health and preferences for life-prolonging treatments: an application of prospect theory to end-of-life decision making. Soc Sci Med. 2007;65(8):1695–1707. doi:10.1016/j.socscimed.2007.06.012
11. Stewart D, Shambasani P. Focus Groups: Theory and Practice.
12. Kitzinger J. Qualitative research. Introducing focus groups. BMJ. 1995;311(7000):299–302. doi:10.1136/bmj.311.7000.299
13. Castleberry A, Nolen A. Thematic analysis of qualitative research data: is it as easy as it sounds? Curr Pharm Teach Learn. 2018;10(6):807–815. doi:10.1016/j.cptl.2018.03.019
14. Rosato R, Di Cuonzo D, Ritorto G, et al. Tailoring chemotherapy supply according to patients’ preferences: a quantitative method in colorectal cancer care. Curr Med Res Opin. 2019;36:73–81. doi:10.1080/03007995.2019.1670475
15. Raia F, Deng M. Relational Medicine: Personalizing Modern Healthcare: The Practice of High-Tech Medicine as a Relational Act. World Scientific Publishing/Imperial College Press; 2015.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
