Back to Journals » Clinical Ophthalmology » Volume 13
Pathology Of “Post-Upper Blepharoplasty Syndrome”: Implications For Upper Eyelid Reconstruction
Authors Steinsapir KD , Kim YD
Received 5 April 2019
Accepted for publication 24 September 2019
Published 17 October 2019 Volume 2019:13 Pages 2035—2042
DOI https://doi.org/10.2147/OPTH.S211289
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Supplementary video demonstrating the upper eyelid surgery in a post-upper blepharoplasty patient illustrated in Figures 1E and 1F.
Views: 20187
Kenneth D Steinsapir,1 Yoon-Duck Kim2
1Orbital and Ophthalmic Plastic Surgery Division, UCLA Stein Eye Institute, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA; 2Oculoplastic and Orbital Surgery Division, Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
Correspondence: Kenneth D Steinsapir 9001 Wilshire Blvd, Suite 305, Beverly Hills, CA 90211, USA
Tel +1 310 274 7422
Fax +1 310 274 7423
Email [email protected]
Background: The anatomical basis for eyelid changes after upper blepharoplasty is largely uninvestigated. The post upper blepharoplasty syndrome (PUBS) is here defined as upper eyelid ptosis, hollow sulcus, high or absent upper eyelid crease, eyelash ptosis, loose eyelid platform skin, and compensatory brow elevation.
Objective: The anatomical basis for the post-upper blepharoplasty syndrome was investigated.
Methods: A retrospective, case-controlled, consecutive series of patients was explored for blepharoptosis after cosmetic blepharoplasty (cases) or ptosis surgery (controls). The upper eyelid crease was lowered, blepharoptosis was corrected by anterior levator aponeurosis resection ptosis surgery, eyelash ptosis was corrected with anchor blepharoplasty, and upper eyelid fold volume was restored using anterior orbital fat. Morphologic and anatomical findings were compared between case and control eyelids.
Results: Data were available for 42 patients (81 eyelids). Case and control eyelids presented with a clinically similar appearance but internally had a marked difference in their anatomical findings. Eyelids with post-upper blepharoplasty syndrome (n= 24 patients, 48 eyelids) were internally found to have a white-line disinsertion of the levator aponeurosis. The disinserted, central levator aponeurosis was bound into the septal scar created by removal of anterior orbital fat at blepharoplasty. Among the 18 controls (33 eyelids), levator disinsertion was not identified.
Conclusion: Hollowness and ptosis in post-upper blepharoplasty syndrome eyelids are related to a white-line disinsertion of the levator aponeurosis and matting of anterior orbital fat in the internal septal scar created during fat removal with blepharoplasty. Knowing where to look for the disinserted central levator is critical to surgically repairing these post-blepharoplasty eyelids.
Keywords: eyelid surgery, anchor blepharoplasty, ptosis surgery, cosmetic surgery, Asian eyelid surgery
Introduction
The post-upper blepharoplasty “look” is characterized by pretarsal skin laxity, an absence of an upper eyelid fold, and a hollow upper eyelid sulcus, encompassing a range of clinical appearances. Overresection of skin, muscle, and fat is the presumed basis for these changes.1,2 The term "look" implies the appearance is intentional. We suggest that upper eyelid ptosis, eyelash ptosis, hollow upper eyelid sulcus, superiorly displaced or absent upper eyelid crease, laxity of eyelid platform skin (with crepey skin), and compensatory brow elevation in these eyelids is an iatrogenic syndrome. We hypothesize that the internal eyelid wound from opening the orbital septum to remove anterior orbital fat causes secondary internal contraction in the eyelid. The internal healing process results in disinsertion of the distal levator aponeurosis through traction of the inferior remnant of superior orbital septum that fuses into the levator aponeurosis. We refer to this constellation of findings as the post-upper blepharoplasty syndrome (PUBS). These changes skeletonize the upper eyelid and age its appearance. A second group of patients also present with a very similar clinical appearance: those who underwent upper eyelid ptosis repair with unsatisfactory results. Their upper eyelids also present with ptosis, eyelash ptosis, a long lid platform, high lid crease, and crepey skin, and the eyebrow has a compensatory elevation.
Fat grafting, with liposuction aspirate, lumbrical and pearl fat grafts, and, increasingly, the placement of hyaluronic acid fillers, had been used to manage the hollow upper eyelid sulcus.3–5 Volume, however, does not repair eyelid and eyelash ptosis, restore the upper eyelid crease, or address compensatory changes of brow position. Newer surgical methods have been introduced to lower the eyelid crease.6,7 These methods include making a new crease at a more appropriate height, performing an anchor blepharoplasty to force a lid fold at a lower level, and reestablishing volume of the upper eyelid fold by mobilizing anterior orbital fat to fill the fold.
We examined this approach in a consecutive series of both Western and Asian patients presenting with complaints of upper eyelid hollowing and ptosis after upper blepharoplasty or ptosis surgery. Specifically, we sought to study the anatomical basis for the common features seen in PUBS and to determine whether these two groups, which look clinically similar after surgery, differed in their underlying anatomical findings. In contrast to the findings in the eyelids after ptosis surgery, the PUBS upper eyelids have a disinserted central levator aponeurosis. The aponeurosis was consistently found bound into the scar complex related to the septostomy of the orbital septum performed to gain access to and resect anterior orbital fat at the time of blepharoplasty. Knowledge of where to find the disinserted levator aponeurosis is critical in reconstructing these eyelids. To our knowledge, this is the first published description of these findings in association with the management of the PUBS eyelid. A detailed description of the procedure with a video (Supplementary Video) is provided to help others surgically mange PUBS eyelids.
Methods
Patients
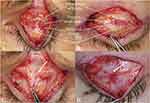
Patients referred to one of the authors (KDS) from January 2012 to January 2017 were eligible for the study if they presented with upper eyelid ptosis and hollowness 6 or more months after cosmetic upper blepharoplasty (cases) or ptosis correction surgery (controls) (see Figure 1). A high upper eyelid crease was defined as a crease height greater than 8 mm in Asian eyelids and 10 mm in Western eyelids. A hollow upper eyelid was defined as the absence of an upper eyelid fold that covers all or part of the tarsal platform (see Figure 1A, C, and E). A range of eyelid appearances was possible with these changes. Each patient had a complete oculoplastic assessment. Medical records were requested and reviewed when obtained.
The study was a retrospective chart review and qualified for an IRB waiver (Integreview IRB, Austin, Tx). The study complied with the requirements of the Declaration of Helsinki, the Belmont Report, Department of Health and Human Services Regulations, and the Health Information Portability and Accountability Act (HIPAA). Publication release was obtained for the use of clinical images and video from all patients.
Surgical Technique
Patients received intravenous sedation with sufficient local anesthesia (lidocaine 1% with 1:100,000 epinephrine) to achieve tissue anesthesia without motor akinesia. The new upper eyelid crease was positioned between 5.5 mm and 7.5 mm irrespective of the location of the prior upper eyelid incision scar. Skin excision varied from 2 to 6 mm. The procedure was identical for both Western and Asian eyelids. The skin and orbicularis oculi muscle were excised in separate layers to minimize disruption to the pretarsal and preaponeurotic space. The findings were noted. Absence of the central levator aponeurosis inserting into the tarsus identified a levator disinsertion. Patient cooperation was used to help identify the levator aponeurosis with lid excursion. A white-line disinsertion is the posterior surface of the levator aponeurosis folded back on itself. (see Figure 2A and B). White-line disinsertions were explored by dissecting superiorly in a plane immediately posterior to the orbicularis oculi muscle (Supplementary Video). The disinserted anterior levator aponeurosis was found adhering to the septostomy scar created when the orbital septum was surgically opened at the time of the original blepharoplasty. The distal orbital septum provided a landmark that could be vertically divided centrally to identify the septal fusion with the levator aponeurosis in all cases (see video). In the white-line disinsertions, there was generally loose areolar tissue above the level of the tarsus between the posterior surface of the levator aponeurosis and anterior to the superior tarsal (Müller’s) muscle, which was dissected as high as Whitnall’s ligament as needed to advance the levator aponeurosis.
For eyelids in which the anterior levator aponeurosis fused to the tarsus, the surgical approach was a routine anterior levator resection ptosis surgery, which is well described in the literature.8–11 In both types of eyelids, anterior orbital fat was mobilized from the septal scar and redraped over the anterior levator aponeurosis. This step helped to restored volume to the upper eyelid fold. In three PUBS cases, insufficient anterior orbital fat was present to provide adequate volume to the upper eyelid fold, and autogenous grafted fat was used to augment the anterior orbital fat volume. This fat was harvested from the abdomen and used with minimal processing. An upper eyelid crease was then formed with three externalized horizontal mattress sutures of 6-0 polyglactin 910 (Vicryl, Ethicon, Bridgewater, New Jersey) from the eyelid platform skin and orbicularis to the cut edge of the levator aponeurosis. These were adjusted to provide minimal tension on the eyelid platform skin and orbicularis oculi muscle to smooth the platform and gently evert the upper eyelid lashes. The incision was then run closed with 6-0 fast-absorbing gut suture. Figure 1 shows preoperative and postoperative photographs. Supplementary Video is a video that demonstrates the surgery for the patient with PUBS featured in Figure 1E and F.
The gut suture and the crease-forming sutures were removed on the sixth postoperative day. Patients were examined at 1 day, 1 and 3 weeks, and 3 and 6 months after surgery. Only patients with 6 months of follow-up were included for analysis. Patients subjectively rated the success of surgery using the following Likert-type scale of eyelid appearance: 0, worse; 1, unchanged; 2, improved; and 3, markedly improved. Brow and eyelid positions were assessed using ImageJ software (National Institutes of Health, Bethesda, MD).
Data Analysis
Morphologic and anatomical findings were compared between case and control eyelids. The Student t-test, the paired t-test, and the Χ2 test were used for statistical analysis where appropriate. Differences were considered statistically significant when the probability of the difference occurring by chance alone was 5% or less.
Results
Between July 2012 and July 2017, a total of 46 consecutive patients (34 patients with Western eyelids and 12 with Asian eyelids) met clinical criteria. This represented 9% (46/516) of all upper eyelid surgery cases performed by the senior author (KDS) during this period. Data for 6-month follow-up visits were not available for 4 patients, and these cases were excluded. Of the 42 patients with 6-month follow-up data, 37 were female and 5 were male. The mean follow-up (SD) was 43 ± 16 months (range, 15–71 months). The mean age (SD) was 45 ± 12 years (range, 28–71 years). All cases demonstrated a levator function of 12 mm or more. There were 24 patients (48 eyelids) who presented after cosmetic upper blepharoplasty and 18 patients who presented after upper eyelid ptosis surgery. Three of the upper eyelid ptosis cases were unilateral and 15 were bilateral. The original ptosis surgery was a Müller’s muscle-conjunctival resection in 73% of the ptosis cases (24/33 eyelids), and anterior levator resection ptosis surgery in 27% of the ptosis cases (9/33 eyelids).
The preoperative upper eyelid margin to central corneal light reflex (MRD1) ranged from 2.0 to 4.0 mm. In the two cases in which the MRD1 was 4.0 mm, there were noticeable postsurgical contour irregularities affecting the upper eyelid warranting anterior levator resection ptosis surgery to address the contour issue (see Figure 1C). The mean margin-to-crease distance (MCD) before surgery was 10 ± 2 mm. Postoperatively the MCD was 7.0 ± 0.6 mm (P<0.0001). The preoperative MDR1 was 3.0 ± 1.0 mm, and postoperatively the MRD1 was 3.8 ± 0.3 mm (P=0.0003). Before surgery, the brow height measured from the central cornea to the lowest brow cilia was 16.3 ± 2.7 mm, and after surgery the brow height was 15.0 + 2.8 mm (P=0.0002).
All the post-blepharoplasty patients denied a history of ptosis prior to blepharoplasty. Satisfactory clinical or social photographs were available for 71% of cases (30/42), and these images supported the contention that ptosis was not present before blepharoplasty. Most patients had a single prior eyelid surgery, but six had two or more upper eyelid surgeries (range, 2–7 procedures). There were no cases of levator attenuation.
Of the 81 eyelids included in this study, a white-line central disinsertion of the levator aponeurosis was noted in each of the 48 eyelids presenting after blepharoplasty (24 patients; Figure 2A and B). Uniformly in these cases, there was a septal scar replacing the bulk of the superior orbital septum. With dissection, the remnants of the caudal aspect of the superior orbital septum could be identified (Figure 2C), permitting its use as a landmark for identifying the levator aponeurosis where these two structures fuse (see video). While the disinsertion of the levator aponeurosis represents surgical trauma to the central levator aponeurosis insertion on the tarsus, there were no cases demonstrating evidence of direct surgical trauma to the levator aponeurosis among the blepharoplasty cases such as a severed or partially severed levator. In each of these cases, opening the orbital septum made it possible to trace out and define the distal central levator aponeurosis.
Despite the history of blepharoplasty, it was possible to mobilize remaining anterior orbital fat to cover the advanced levator and help provide volume to the reconstructed upper eyelid fold in all but three cases. In these later cases, anterior orbital fat was augmented with autologous grafted fat to create a more optimal fold volume.
There were no white-line disinsertions found in the 33 eyelids that had ptosis surgery. The external morphology of post-ptosis surgery cases resembled that of the PUBS cases. We hypothesize that this is due to the long, ptotic upper eyelid platform from inadequate levator aponeurosis advancement, compensatory eyebrow elevation lifting the retro-orbicularis oculi fat pad and reducing its contribution to upper eyelid fold volume, and matting of the anterior orbital fat by septal scarring associated with prior anterior levator dissection. It was our impression that septal scarring was less dramatic in the Müller’s muscle-conjunctival resection cases (Figure 2D), but this difference was not quantitated.
Complications in the series were minor. One patient requested revisional ptosis surgery at 1 year. Two patients required lid massage to successfully address contour issues. Two patients receive supplemental hyaluronic acid filler to the upper eyelid fold for additional fullness. Despite these challenges, all patients subjectively rated their eyelids’ appearance and function as markedly improved at 6 months (3.0 on appearance scale: 0, worse; 1, unchanged; 2, improved; and 3, markedly improved).
Discussion
We discovered that central levator disinsertion is the anatomical basis for post upper blepharoplasty syndrome (PUBS). This syndrome is not a “look” but an iatrogenic condition.1,2 It is caused by levator pathology rather than overresection of soft tissue, and it is amenable to repair using the tissues found in the eyelid in most cases. The syndrome is characterized by a high or absent upper eyelid crease, a hollow upper eyelid with a rudimentary or absent upper eyelid fold, eyelid and lash ptosis, loose eyelid platform skin, and a compensatory eyebrow elevation. Our findings stand in sharp contrast to the recent report by Mendelson and Luo,2 who found that only 12% of their secondary blepharoplasty patients presented with upper eyelid ptosis. We suspect that more of their patients with a post-blepharoplasty “look” may have had upper eyelid ptosis that went undiagnosed. Differences in their study and ours may also be due to differences in referral patterns.
We hypothesize that the morphology of the PUBS eyelid is caused by post-surgical changes to the levator aponeurosis rather than excessive tissue removal as previously thought.1,2,12 The post-ptosis surgery patients presented with an external eyelid that is morphologically similar to the PUBS eyelids with a high crease, lash ptosis, a long upper eyelid platform, and a high hollow sulcus. In these eyelids, the levator is fused to the tarsus as a consequence of the ptosis procedure. Here, the relative superior retraction of the insufficiently advanced levator aponeurosis contributes to the lack of soft-tissue volume in the anterior superior orbit. Compensatory eyebrow elevation in response to the upper eyelid ptosis also contributes to the appearance of a lack of “spare” skin in the upper eyelid fold.
To help understand these morphologic changes, we introduce two new terms to describe the configuration of the upper eyelid: antiform fold and synform fold. These terms borrow the language that geologists have for how lamellar structures fold (Figure 3A).13 Normally, the upper eyelid fold is a convex downward fold with fullness contributed by anterior orbital fat that bows forward in the relaxed septum and the subbrow fat. Borrowing from the term used by geologists, we call this an “antiform fold” (Figure 3B). The hollow upper eyelid results from an inversion of the normal upper eyelid fold with retraction of the partially disinserted levator or an inadequately advanced levator in the case of a post-ptosis surgery eyelid, matting of anterior orbital fat in the septal scar, and diminished fat volume from direct surgical resection, making for a concave downward fold. We call this a “synform fold” (Figure 3C). Upper eyelid ptosis will also cause a compensatory eyebrow elevation that contributes to the impression of a lack of upper eyelid skin and soft tissue.
Jones and co-workers11 described aponeurotic ptosis repair in the early 1970’s. Dortzbach and Sutula14 studied the histopathology of involutional blepharoptosis in 19 eyelids, and approximately 71% of their cases showed histologic evidence of disinsertion of the aponeurosis. Anderson and Beard9 described the white-line disinsertion as the “rolled edge of the retracted fibers of the aponeurosis.” All the PUBS eyelids in our series demonstrated white-line central levator disinsertion. We suspect but did not establish that this disinsertion may be more likely to occur in cases with early levator dehiscence with or without ptosis. Baylis and co-workers15 reviewed the subject of levator injury but did not describe this mechanism. We did not find in any of the 81 eyelids in our study evidence of direct surgical trauma to the levator such as a severed aponeurosis. Rather, the disinsertion of the distal aponeurosis appears related to traction on the distal septum. With the original blepharoplasty, the surgeon opens the septum to remove anterior orbital fat. Scar contraction associated with healing after the blepharoplasty septostomy appears to cause the central, white line levator disinsertion. This may only occur in predisposed eyelids. As this was not a prospective study, we can’t answer that question.
A postsurgical upper eyelid hollow has been identified as a cosmetic issue in both Asian and non-Asian eyelids. As noted in the introduction, solutions for this hollow have focused on adding volume to the superior sulcus.4 In contrast, Chen et al6 addressed these issues by making a new lower eyelid crease incision at the desired height (generally 6 mm in Asian eyelids). They corrected ptosis by reattaching the distal levator to the superior tarsus and releasing preaponeurotic fat to cover the repositioned aponeurosis, and then closing the eyelid with supratarsal fixation.6 A similar approach was also described by Kim.7 We adopted this approach in this study, which includes patients with both Western and Asian eyelids. Not previously described is the presence of a white-line disinsertion in these eyelids, which was a common feature in the post-upper blepharoplasty eyelids (48/48 eyelids). It is important to understand how to locate and manage the disinserted distal levator aponeurosis in these eyelids. It is essential to have a cooperative patient. The ability to have the patient look up and down on command during surgery makes it possible to find a white levator aponeurosis embedded in the white septal scar.
Conclusion
Post-upper blepharoplasty syndrome is characterized by upper eyelid ptosis, lash ptosis, high or indistinct upper eyelid crease, hollow upper eyelid sulcus (absent upper eyelid fold), and a compensatory eyebrow elevation. We call this configuration a “synform” upper eyelid fold. A normal outward upper eyelid fold is called an “antiform fold.” We hypothesize a synform fold is caused by the healing process associated with the internal septostomy made to access anterior orbital fat at the time of blepharoplasty through the orbital septum. We hypothesize that wound contraction draws up the distal septum, placing sufficient traction on the levator aponeurosis in predisposed eyelids to centrally disinsert the levator aponeurosis. Matting of orbital fat in the anterior septal scar tissue and compensatory eyebrow elevation in response to upper eyelid ptosis contribute to the appearance of the hollow upper eyelid sulcus. Upper eyelash ptosis and wrinkling of the upper eyelid platform skin are caused by the loss of attachment between the eyelid platform skin, underlying orbicularis oculi, and the levator aponeurosis.
Anecdotally, we have seen eyelids that were compromised by excess tissue resection, but based on the results of this series, these cases may be the exception rather than the rule. Individuals with a preexisting levator dehiscence before cosmetic blepharoplasty may be predisposed to the development of PUBS. For these individuals, the aesthetic surgeon should consider a prophylactic anchor blepharoplasty or levator advancement at the time of primary blepharoplasty. Patients with PUBS are often told by the consulting eyelid surgeon that there is “not enough skin to fix the eyelid.” This is a canard. This study establishes that these eyelids can be surgically repaired with knowledge of the underlying anatomy.
Acknowledgments
No external funding was received for this study. This paper was presented in part at the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) 47th Annual Fall Scientific Symposium, Chicago, Illinois, October 14, 2016.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fagien S. The role of the orbicularis oculi muscle and the eyelid crease in optimizing results in aesthetic upper blepharoplasty: a new look at the surgical treatment of mild upper eyelid fissure and fold asymmetries. Plast Reconstr Surg. 2010;110:653–666. doi:10.1097/PRS.0b013e3181c87cc6
2. Mendelson B, Luo D. Secondary upper lid blepharoplasty: a clinical series using the tarsal fixation technique. Plast Reconstr Surg. 2015;135:50e–515e. doi:10.1097/PRS.0000000000001042
3. Frileck SP. The lumbrical fat graft: a replacement for lost upper eyelid fat. Plast Reconstr Surg. 2002;109:1696–1705. doi:10.1097/00006534-200204150-00036
4. Shorr N, Christenbury JD, Goldberg RA. Free autogenous ‘pearl fat’ grafts to the eyelid. Ophthalmic Plast Reconstr Surg. 1988;4:37–40. doi:10.1097/00002341-198801130-00006
5. Choi HS, Whipple K, Oh SR, et al. Modifying the upper eyelid crease in Asian patients with hyaluronic acid fillers. Plast Reconstr Surg. 2011;127:844–849. doi:10.1097/PRS.0b013e3181fed6cb
6. Chen SH, Mardini S, Chen HC, et al. Strategies for a successful corrective Asian blepharoplasty after previously failed revisions. Plast Reconstr Surg. 2004;114:1270–1277. doi:10.1097/01.prs.0000135951.55118.59
7. Kim YD. Revision of Asian upper eyelid crease. In: Korn BS, Kikkawa DO, editors. Video Atlas of Oculofacial Plastic and Reconstructive Surgery.
8. Anderson RL, Dixon RS. Aponeurotic ptosis surgery. Arch Ophthalmol. 1979;97:1123–1128. doi:10.1001/archopht.1979.01020010577015
9. Anderson RL, Beard C. The levator aponeurosis: attachments and their clinical significance. Arch Ophthalmol. 1977;95:1437–1441. doi:10.1001/archopht.1977.04450080147019
10. Carroll RP. Cautery dissection in levator surgery. Ophthalmic Plast Reconstr Surg. 1988;4:243–247. doi:10.1097/00002341-198804040-00009
11. Jones LT, Quickert MH, Wobig JL. The cure of ptosis by aponeurotic repair. Arch Ophthalmol. 1975;94:629–634. doi:10.1001/archopht.1975.01010020601008
12. Rohrich RJ, Coberly DM, Fagien S, Stuzin JM. Current concepts in aesthetic upper blepharoplasty. Plast Reconstr Surg. 2004;113:32e–42e. doi:10.1097/01.prs.0000105684.06281.32
13. Fleuty MJ. The description of folds. Proc Geol Assoc. 1964;75:461–492. doi:10.1016/S0016-7878(64)80023-7
14. Dortzbach RK, Sutula FC. Involutional blepharoptosis: a histopathologic study. Arch Ophthalmol. 1980;98:2045–2049. doi:10.1001/archopht.1980.01020040897022
15. Baylis HI, Sutcliffe T, Fett DR. Levator injury during blepharoplasty. Arch Ophthalmol. 1984;102:570–571. doi:10.1001/archopht.1984.01040030448023
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.