Back to Journals » Patient Preference and Adherence » Volume 16
Parturients’ Stated Preferences for Labor Analgesia: A Discrete Choice Experiment
Authors Ozdemir S , Chen T, Tan CW , Wong WHM, Tan HS, Finkelstein EA, Sng BL
Received 9 December 2021
Accepted for publication 29 March 2022
Published 8 April 2022 Volume 2022:16 Pages 983—994
DOI https://doi.org/10.2147/PPA.S353324
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Semra Ozdemir,1– 3 Teresa Chen,4 Chin Wen Tan,4,5 Wei Han Melvin Wong,1,2 Hon Sen Tan,4,5 Eric Andrew Finkelstein,1– 3,6 Ban Leong Sng4,5
1Health Services and Systems Research, Duke-NUS Medical School, Singapore; 2Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore; 3Saw Swee Hock School of Public Health, National University of Singapore, Singapore; 4Duke-NUS Medical School, Singapore; 5Department of Women’s Anesthesia, KK Women’s and Children’s Hospital, Singapore; 6Duke University Global Health Institute, Duke University, Durham, NC, USA
Correspondence: Semra Ozdemir, Duke-NUS Medical School, 8 College Road, 169857, Singapore, Tel +65 6601 3575, Email [email protected]
Objective: The objective was to investigate the extent to which treatment benefits, risks and costs affected parturients’ preferences for labor analgesia.
Methods: We recruited 248 healthy parturients prior to labor at an antenatal ward and administered a discrete choice experiment survey. Parturients were asked to choose among four hypothetical forms of labor analgesia: epidural analgesia, pethidine, Entonox and no analgesia, which were defined by: pain score, duration of second stage of labor, risks of instrumental delivery, back pain and permanent nerve injury, and out-of-pocket cost. We used mixed logit model to calculate the relative importance of each attribute (out of 100).
Results: Parturients preferred receiving labor analgesia over not receiving analgesia and those who had positive past experience with epidural preferred epidural over other modalities. Out-of-pocket cost (28%), duration of second stage of labor (26%) and pain score following treatment (18%) were the most important attributes.
Conclusion: Out-of-pocket cost was a major concern. Parturients prioritized having lower pain and shorter labor experience over risks associated with epidural analgesia. Parturients should be presented with realistic range of risks of side-effects so that they can decide how to balance risks against benefits and costs associated with child labor.
Keywords: analgesia, epidural analgesia, labor analgesia, patient preferences
Introduction
While childbirth can be extremely painful,1 labor analgesia including epidural analgesia, pethidine, and entonox can help with pain mitigation. Epidural analgesia involves injecting local anesthetics and/or lipophilic opioids into the lumbar epidural space.2 It is considered the gold standard for labor analgesia at reducing pain and improving maternal satisfaction compared to the other non-epidural analgesia.3 Pethidine or meperidine hydrochloride is an opioid injected into the thigh or buttocks and takes about 20–30 minutes to start working. However, it is associated with neonatal respiratory depression.4 Entonox is a nitrous oxide-oxygen mixture that can be inhaled via a mouth mask and takes about 20–30 seconds to work.5
Use of epidural analgesia has increased in recent years.6,7 While epidural analgesia provides effective pain relief, its use has been associated with increased duration of second stage of labor and increased risk of instrumental delivery compared to non-epidural analgesia.3 However, the result of recent studies demonstrate no difference in duration of second stage labor between epidural analgesia and non-epidural analgesia8 or no analgesia,9 and no difference in the risk of instrumental delivery between epidural analgesia and no analgesia.3 Parturients may also be also concerned about developing back pain10,11 and risk of permanent nerve injury12 although evidence shows that the risk of long-term back pain following epidural analgesia was not significantly different than non-epidural analgesia.3 The risk of permanent nerve injury is also very rare.13
Parturients may be interested in epidural analgesia to control labor pain, while others prefer to avoid it due to their perceived concerns and risks.14,15 There might also be other factors contributing to parturients’ preferences for and satisfaction with childbirth and labor process.16 Past labor experience may also affect parturients’ future choice of analgesia. For example, women who used epidural analgesia during past labor may prefer epidural analgesia in future labor.17 The demand for epidural analgesia may also be affected by its out-of-pockettrade off benefits with the risks and cost of epidural analgesia, compared to other forms of labor analgesia (or no analgesia) remains to be explored.
Our primary objective was to investigate to what extent benefits, risks and cost affect parturients’ preferences for epidural analgesia compared to pethidine, Entonox and not receiving analgesia. We hypothesized that the predicted demand (ie, probability of choosing) for epidural analgesia would be higher for lower pain score following treatment, shorter second stage of labor, lower risks of instrumental delivery, back pain and permanent nerve injury, and lower out-of-pocket cost. The secondary objective was to investigate whether parturients’ past experience with epidural analgesia affected their preference for epidural analgesia. We hypothesized that parturients who had positive previous experience with epidural analgesia would be more likely to choose epidural analgesia over other forms of labor analgesia or not receiving analgesia. We used a Discrete Choice Experiment (DCE), a survey research method for assessing preferences for health care products and services, to achieve the objectives of this study.
Methods
Study Setting
The study was conducted from June 2018 to November 2020 in KK Women’s and Children’s Hospital (KKH), the largest maternity care institution in Singapore, as part of a larger study. Epidural analgesia is utilized in approximately 50% of the parturients undergoing labor at KKH.18 The other methods of labor analgesia commonly administered in the hospital include intramuscular pethidine and Entonox. Non-pharmacological methods such as massage and water therapy are not commonly used in Singapore, including the study setting. The care of delivery is mainly hospital based with private specialist care or team-based obstetric care.
Optional antenatal classes are available for parents to receive education on pregnancy and postpartum care at the study site. Women are briefed on the form of labor analgesia that they requested, including procedures, possible side effects, and risks. Parturients are asked to sign a separate consent form if they request epidural analgesia. Partners are allowed to stay in the delivery suite during labor, and midwives are available to offer support and guidance at all times. The organization of care did not change during the COVID-19 period.
The inclusion criteria included being 1) healthy women based on American Society of Anesthesiologist physical status and 2) at 36 weeks gestation or more (both nulliparous and multiparous) with a singleton fetus. The exclusion criteria were having 1) multiple gestations, 2) non-cephalic fetal presentation, 3) obstetric complications (eg, preeclampsia, premature rupture of amniotic membranes for more than 48 hours, gestational diabetes requiring insulin, pregnancy-induced hypertension on anti-hypertensive medications) and medical conditions that require regular management and close surveillance (eg, cardiac disease), and iv) elective caesarean section. These exclusion criteria are confounding factors that may increase the risk of neonatal complications or result in lack of labor pain experience. Trained research coordinators screened the medical records for eligibility and approached eligible parturients who were admitted to the antenatal ward prior to labor and delivery. After receiving written consent, participants were then asked to complete the survey in English as it has been the primary language for teaching in public schools in Singapore since 1987.19
Ethical Considerations
Ethical approval for this study was provided by the SingHealth Centralized Institutional Review Board in Singapore before the data collection commenced (SingHealth CIRB Reference: 2017/2090). The study was also registered on clinicaltrials.gov (NCT03167905). All participants were given a clear and detailed description of the study before they voluntarily signed informed consent forms. This study complies with the Declaration of Helsinki and adheres to the applicable Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Survey Development
DCE is a research methodology used to assess individuals’ preferences via a series of choice tasks where individuals are asked to select the utility-maximizing (ie, most preferred) alternative from two or more alternatives.20 trade off different attributes associated with a healthcare product or service, and to calculate its predicted demand given the characterizing attributes.21,22
We conducted a literature review to determine the labor analgesia attributes that mattered most to parturients. A list of attributes was shortlisted based on the literature review and through consultation with physicians. We then pretested the initial draft of the survey instrument with 10 eligible parturients following a “think-aloud” protocol23 to investigate if parturients were able to understand the questions, whether all relevant attributes were captured in the design, whether there are any important missing attributes and whether parturients were able to make trade-offs between the attributes. We refined the framing of the questions and descriptions based on the feedback from these interviews.
The final list of six attributes used in the study were 1) pain score following treatment [1: lowest possible pain, 2, 3 or 4 (out of 10: highest possible pain)]; 2) duration of second stage of labor (ie, time taken from cervical to full dilatation to delivery of fetus) (0.5, 1, 2 or 3 hours); 3) risk of instrumental delivery (15%, 30% or 50%); 4) risk of back pain (25%, 35% or 45%); 5) risk of permanent nerve injury (0.01%, 0.05% or 0.10%); and 6) out-of-pocket cost (Singapore dollars (SGD) 300, 600, 1200 or 2000). The attribute levels were derived based on the evidence from literature and discussions with clinicians.3 The levels for the cost attribute were identified based on the out-of-pocket cost that subsidized and unsubsidized parturients pay in Singapore. However, as commonly done in DCE studies, the ranges also included larger than real-life values to investigate whether patrutients were willing to accept higher risks or costs.
For each DCE task, four hypothetical forms of labor analgesia were provided: 1) epidural analgesia, 2) pethidine, 3) Entonox (introduced as “laughing gas” in the questionnaire), and 4) not receiving labor analgesia. Each form of labor analgesia was first briefly explained at the beginning of the questionnaire. To reduce the cognitive burden on respondents, the profiles for the non-epidural alternatives were kept fixed across the DCE tasks (ie, they had the same levels for each attribute in all DCE tasks). Attribute levels differed across the DCE tasks only in the case of epidural analgesia. We also added “risk of respiratory distress for the baby” as one of the attributes for pethidine, which was kept fixed across the DCE tasks. The parturients were asked to select their preferred form of labor analgesia in each DCE task (sample DCE task illustrated in Figure 1).
 |
Figure 1 Sample DCE task. |
The DCE tasks were created based on an experimental design using SAS software, which chose a design based on optimal D-efficiency.24 We allowed interaction effects between pain score following treatment and duration of second stage of labor. The design generated 48 DCE tasks, which were divided into six blocks of eight tasks. To reduce cognitive burden, each parturient was randomized to receive one of the six blocks. To test for validity of responses, we also added a manually designed DCE task where parturients were shown the best levels of each attribute for epidural analgesia. Parturients were considered not attentive if they chose epidural in any one of the eight tasks they had seen but did not choose epidural when it was presented with the best attribute levels. Each parturient was asked to answer nine DCE tasks in total.
The questionnaire first provided information about labor-pain management and the attributes used in the study. A sample DCE task was then presented providing instructions on how to answer the questions. The questionnaire also included questions on demographics (eg, age and ethnicity), parturients’ perceptions about various forms of labor analgesia (epidural, pethidine, and Entonox), previous labor experiences, and their satisfaction with previous labor experience (if any).
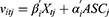
Sample Size
Based on Orme’s formula,25 the required minimum sample size is dependent on the number of maximum attribute level (m=4), the number of non-fixed alternatives (a=1), and the number of choice tasks per respondent (q=8):  .
.
Statistical Analysis
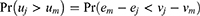
We used random utility model to analyze the responses to the DCE tasks [16]. For each analgesia alternative j, the utility (uj) is determined by the observable component (vj) and unobservable component, random error term (ej):
Respondents will choose the option that gives them the highest expected utility such that the probability of alternative j being chosen over option m is
We used a mixed logit model (also known as a random parameters logit model) to analyze the DCE choice data to allow for preference heterogeneity (ie, variation across individuals).26 The model also accounted for multiple observations from each respondent. The observable component of utility (vitj) of an individual i in choice task t for labor analgesia j is approximated by a linear combination of pain score following treatment, duration of second stage of labor, risks of instrumental delivery, back pain and permanent nerve injury, and out-of-pocket cost.
The final model did not include the interaction effects between pain score and duration of second stage of labor attributes as they were found to be not significant. We also specified an alternative specific constant (ASCj) for labor analgesia j where j indicates epidural analgesia, pethidine or Entonox. Not receiving analgesia option was set as the reference level. ASCs represent preferences for the respective alternatives that were not captured by the attributes. The risk of respiratory distress for the baby was not included in the analysis since it was kept at the same level across the DCE tasks. Any effect of “risk of respiratory distress for the baby” on preferences would be captured by the ASC associated with pethidine. The empirical model is defined as follows:
Vectors βi and αi contain individual-level random parameters for all attributes and ASCs, respectively, which are assumed to be independently and identically distributed normal with a mean and standard deviation estimated by the model. All the attribute levels were dummy coded. The worst level for each attribute was set as the reference level with a numerical value of 0. The coefficients can be interpreted as preference weights for each attribute level or specified alternative.
To address the second aim of the study, we created a dummy variable indicating having positive previous experience with epidural analgesia. Positive epidural experience was defined as using epidural in a previous labor and reporting at least 80 out of 100 in satisfaction score. Since respondent characteristics cannot enter into the model directly, we created an interaction effect between this dummy variable and ASC for epidural to denote preferences for epidural analgesia given a positive previous experience with epidural.
We calculated relative attribute importance based on the attributes and levels used in the study. The relative attribute importance shows which attributes of labor analgesia modalities are more or less important when choosing one. It is calculated as the utility difference between the best and worst levels of an attribute divided by the sum of utility differences for all attributes.27 We then scaled it out of 100 so that the relative attribute importance for each attribute can be interpreted as its contribution to the overall utility out of 100.
To calculate predicted demand for a form of labor analgesia, we calculated the utility associated with epidural analgesia, pethidine, Entonox and no labor analgesia for each respondent using individual-level random parameters. Each individual was then assigned to the form of analgesia that provided the highest utility for them. We then calculated the proportion of respondents assigned to epidural analgesia, pethidine, Entonox and no labor analgesia. For example, the predicted demand for epidural analgesia was the proportion of respondents who received the highest utility with epidural analgesia over the other alternatives. The epidural analgesia profile was selected based on the evidence on average outcomes from the literature. Accordingly, the average epidural profile had a pain score of 3, duration of second stage of labor of 1-hour, instrumental delivery risk of 15%, back pain risk of 35%, permanent nerve injury risk of 0.01%, and out-of-pocket cost of SGD600.13 We also investigated how predicted demand for epidural analgesia changes based on changes in each epidural attribute while assuming the other attributes at their values at average epidural profile. We used NLOGIT software for all statistical analysis.
Results
Sample Characteristics
Two parturients did not complete their surveys and were excluded from the analytical sample. Ten parturients failed the survey validity test; however, they were not excluded as sensitivity analysis demonstrated their exclusion did not affect the main findings (results of this sensitivity analysis are available upon request). The final analytical sample consisted of 248 parturients with complete responses to the questions used in the analysis. The majority of the parturients were Chinese (59%), married (98%), had university degrees (81%) and nulliparous (73%). The mean age of the parturients was 30.9±3.7 years. About three-fourths (73%) of the women were nulliparous parturients.
About 16% (N=41) of the parturients used epidural analgesia, 16% (N=40) used Entonox and 2% (N=5) used pethidine in their past labor experience. Those who used pethidine also used either Entonox and/or epidural analgesia. Among parturients who used Entonox, more than half used at least one of the other forms of analgesia. Among those who used epidural analgesia, 31 (out of 41) reported positive previous experience with epidural analgesia, while 21 (out of 40) and 2 (out of 5) reported positive experience with Entonox and pethidine, respectively (Table 1).
 |
Table 1 Participant Socio-Demographic Information |
Preferences for Labor Analgesia
In Table 2, the first three columns show the estimated mean preference weights for each attribute level and form of analgesia. Reference levels were fixed at zero and attribute levels associated with larger values indicate greater preference. As expected, parturients, on average, preferred lower pain score following treatment, shorter second stage of labor, lower risks of instrumental delivery, back pain and permanent nerve injury, and lower out-of-pocket cost. Those who reported positive previous experience with epidural preferred using epidural analgesia over not receiving analgesia (β=1.77, P=0.017) while the remaining parturients did not have a preference between epidural analgesia and not receiving analgesia (β=−0.39, P=0.529). Parturients, on average, also preferred pethidine (β=1.53, P<0.001) and Entonox (β=4.21, P<0.001) over not receiving analgesia. The last three columns in Table 2 show the standard deviation of the preference weights. In the final model, we assumed fixed (ie, nonrandom) distribution for the risks of instrumental delivery and back pain since all the standard deviations associated with these attributes were not significant when we assumed them random. The standard deviations were significant (P<0.050) for most (11 out of 14) variables, revealing variation of preferences across parturients. They were the largest for the ASCs for Entonox and pethidine, indicating that these variables had the highest variation in preferences.
 |
Table 2 Mixed Logit Model Estimates |
Figure 2 shows the relative attribute importance (excluding the ASC for forms of labor analgesia) out of 100%. Out-of-pocket cost had the greatest importance (28%), closely followed by duration of second stage of labor (26%) and pain score following treatment (18%). They were followed by risk of instrumental delivery (11%) and risk of back pain (10%) where the risk of permanent nerve injury (6%) was the least important given the levels used in this study.
 |
Figure 2 Relative attribute importance. |
Figure 3 shows the predicted demand for epidural, pethidine, Entonox and no labor analgesia when epidural had the average outcomes. The predicted demand for epidural was 67%; followed by 24% for Entonox and 2% for pethidine. The predicted demand for no labor analgesia was 8%.
 |
Figure 3 Predicted demand of epidural analgesia, pethidine, Entonox and no-labor-analgesia. |
Figure 4 shows the predicted demand for epidural analgesia based on the changes in each epidural outcome. For pain score following treatment, the predicted demand ranged from 63% to 74% for a pain score of 4 to 1 (out of 10). The predicted demand ranged from 50% to 73% when second stage labor lasts from 3 hours to half an hour. The predicted demand ranged from 59% to 70% when the risk of back pain ranged from 45% to 25%. In the case of risk of instrumental delivery, we observed a predicted demand of 56% to 67% for risks ranging from 50% to 15%. The predicted demand of epidural remained around 61% to 67% when the risk of permanent nerve injury ranged from 0.01% to 0.10%. The predicted demand ranged from 42% to 70% for SGD2000 to SGD300 out-of-pocket cost.
 |
Figure 4 Predicted demand of epidural analgesia based on changes in epidural outcomes. |
Discussion and Conclusion
Discussion
We assessed parturients’ preferences for labor analgesia using a DCE survey. Our findings suggest that, on average, parturients preferred using a form of labor analgesia to not receiving any analgesia. When epidural analgesia was associated with average outcomes (based on the literature), the predicted demand for epidural was about 67%. The predicted demand for Entonox was 24%, followed by 8% for no labor analgesia while it was very low at 2% for pethidine.
Our findings also suggest that previous positive experience with epidural analgesia affected preferences for epidural analgesia and other forms of labor analgesia, regardless of the levels shown for each attribute. This finding confirms the evidence from previous studies17,28 that past experience with labor influences future choices or intentions for labor analgesia.
Results also indicated that out-of-pocket cost (28%) was the most important attribute based on the attributes and levels used in the study. Cost was also reported to be one of the reasons of not utilizing epidural analgesia in other countries.14,29,30 The range of out-of-pocket costs we used covered the costs paid by parturients at the study site based on subsidy schemes. The high importance of cost attribute could be attributed to the significant maternity and labor costs.31,32 Although Singapore has a healthcare system that provides subsidies for maternity expenditures based on means-testing, it is often that only those from lower-income families quality for these subsidies. Most families pay out-of-pocket costs.33 Private insurance plans specifically targeting maternity are also available in the country since typical private health insurance plans may not cover maternity costs.
We also found that duration of second stage of labor (26%) and pain score following analgesia (18%) were important attributes when considering whether parturients would use epidural analgesia. Although epidural analgesia was found to be associated with prolonged second stage of labor in earlier studies,3 the delay might be because of reduced contractions due to low or no pain. A recent systematic review on epidural experience in labor also shows that desire to have pain-free labor and duration of labor are the main considerations for women to choose epidural analgesia.34
Risk of instrumental delivery and risk of back pain had similar importance to parturients (about 11% and 10%, respectively). These risks, however, were of secondary importance to out-of-pocket cost, pain score and duration of second stage of labor. Although risk of permanent nerve injury was a significant predictor of preferences for labor analgesia, it had the smallest importance. This may be because the risk of permanent nerve injury (ie, 0.01%)35 is low as presented in this study. However, literature indicates that women are misinformed or not fully informed about the risks and complications associated with epidural analgesia.14,36 If so, our findings suggest that although concerns regarding adverse events or complications may influence medical choices, when provided with the necessary (and accurate) information, parturients are able to balance their concerns regarding permanent nerve injury against the likelihood of these negative consequences realistically occurring.
Our study had several limitations. The parturients in this study were recruited from a single institution; thus, our results may not be generalizable to other pregnant populations. However, the study site is the largest hospital in the country specializing in healthcare for women and is the primary hospital for maternity care and childbirth. The study also did not collect information on household income, which could be correlated with preferences. Future research could investigate whether parturients from different income groups would have different preferences regarding out-of-pocket medical costs associated with labor. Lastly, findings on relative attribute importance and predicted demand are specific to the range of attribute levels used in this study. These limitations should be considered while interpreting the results of this study.
Despite these limitations, our study was one of the few to utilize a DCE method to assess parturient preferences for managing labor pain. This allowed us to systematically quantify how predicted demand for different forms of labor analgesia changes based on the changes in outcomes such as pain, duration of second stage labor, risks and out-of-pocket costs.
Conclusion
In conclusion, our study showed that parturients preferred controlling labor pain via a form of labor analgesia. Past labor experience had a significant impact on parturient preferences showing that past satisfaction with epidural analgesia had a positive influence in choosing it again. Our findings also show that out-of-pocket cost could be a major concern for parturients as it was the most important attribute. Duration of second stage of labor and pain score following treatment were more important than the risks of instrumental delivery, back pain and permanent nerve injury associated with epidural, indicating that parturients prioritized having low pain and shorter labor experience than the possible adverse event risks.
Practice Implications
Our study demonstrates the importance of providing information regarding the risks associated with epidural analgesia and specific information on how it could best support a parturient’s needs in her labor experience. When presented with realistic range of risks of side-effects, parturients focused more on other attributes: out-of-pocket cost, duration of second stage labor and pain score following treatment. We suggest that parturients’ knowledge of and preferences for labor analgesia should be assessed and any misconceptions clarified during antenatal consultations. These efforts would help parturients to develop realistic expectations and improve satisfaction with their labor experience.
Acknowledgments
Semra Ozdemir had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Semra Ozdemir confirms that all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
The authors thank all the respondents who completed the study survey.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Singapore National Medical Research Council (NMRC) Clinician Scientist Award (CSAINV16may004), and Academic Medicine-Enhancing Training, Healthcare, Outcomes and Standards (AM-ETHOS) Medical Student Research Fellowship (AM-ETHOS01/FY2020C2/31-A65).
Disclosure
The authors report no conflicts of interest for this work.
References
1. Melzack R. Labour pain as a model of acute pain. Pain. 1993;53(2):117–120. doi:10.1016/0304-3959(93)90071-V
2. Hawkins JL. Epidural analgesia for labor and delivery. N Engl J Med. 2010;362(16):1503–1510. doi:10.1056/NEJMct0909254
3. Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev. 2018;5(5):Cd000331. doi:10.1002/14651858.CD000331.pub4
4. Kadirogullari P, Yalcin Bahat P, Sahin B, Gonen I, Seckin KD. The effect of pethidine analgesia on labor duration and maternal-fetal outcomes. Acta Biomed. 2021;92(2):e2021065. doi:10.23750/abm.v92i2.10905
5. Mobaraki N, Yousefian M, Seifi S, Sakaki M. A randomized controlled trial comparing use of enthonox with pethidine for pain relief in primigravid women during the active phase of labor. Anesth Pain Med. 2016;6(4):e37420. doi:10.5812/aapm.37420
6. Lain S, Ford J, Hadfield R, Blyth F, Giles W, Roberts C. Trends in the use of epidural analgesia in Australia. Int J Gynaecol Obstet. 2008;102(3):253–258. doi:10.1016/j.ijgo.2008.04.023
7. Bos EME, Schut ME, de Quelerij M, Kalkman CJ, Hollmann MW, Lirk P. Trends in practice and safety measures of epidural analgesia: report of a national survey. Acta Anaesthesiol Scand. 2018;62(10):1466–1472. doi:10.1111/aas.13219
8. Craig MG, Grant EN, Tao W, McIntire DD, Leveno KJ. A randomized control trial of bupivacaine and fentanyl versus fentanyl-only for epidural analgesia during the second stage of labor. Anesthesiology. 2015;122(1):172–177. doi:10.1097/ALN.0000000000000454
9. Shen X, Li Y, Xu S, et al. Epidural analgesia during the second stage of labor: a randomized controlled trial. Obstet Gynecol. 2017;130(5):1097–1103. doi:10.1097/AOG.0000000000002306
10. Petruschke I, Ramsauer B, Borde T, David M. Differences in the Frequency of use of epidural analgesia between immigrant women of Turkish origin and non-immigrant women in Germany - Explanatory approaches and conclusions of a qualitative study. Geburtshilfe Frauenheilkd. 2016;76(9):972–977. doi:10.1055/s-0042-109397
11. Breen TW, Ransil BJ, Groves PA, Oriol NE. Factors associated with back pain after childbirth. Anesthesiology. 1994;81(1):29–34. doi:10.1097/00000542-199407000-00006
12. Mahomed K, Chin D, Drew A. Epidural analgesia during labour - maternal understanding and experience - informed consent. J Obstet Gynaecol. 2015;35(8):807–809. doi:10.3109/01443615.2015.1011103
13. Cook TM, Counsell D, Wildsmith JA; Royal College of Anaesthetists Third National Audit P. Major complications of central neuraxial block: report on the third national audit project of the Royal College of Anaesthetists. Br J Anaesth. 2009;102(2):179–190. doi:10.1093/bja/aen360
14. Ezeonu PO, Anozie OB, Onu FA, et al. Perceptions and practice of epidural analgesia among women attending antenatal clinic in FETHA. Int J Women's Health. 2017;9:905–911. doi:10.2147/IJWH.S144953
15. Toledo P, Sun J, Peralta F, Grobman WA, Wong CA, Hasnain-Wynia R. A qualitative analysis of parturients’ perspectives on neuraxial labor analgesia. Int J Obstet Anesth. 2013;22(2):119–123. doi:10.1016/j.ijoa.2012.11.003
16. Richardson MG, Lopez BM, Baysinger CL, Shotwell MS, Chestnut DH. Nitrous oxide during labor: maternal satisfaction does not depend exclusively on analgesic effectiveness. Anesth Analg. 2017;124(2):548–553. doi:10.1213/ANE.0000000000001680
17. Scotland GS, McNamee P, Cheyne H, Hundley V, Barnett C. Women’s preferences for aspects of labor management: results from a discrete choice experiment. Birth. 2011;38(1):36–46. doi:10.1111/j.1523-536X.2010.00447.x
18. Chan JJI, Gan YY, Dabas R, et al. Evaluation of association factors for labor episodic pain during epidural analgesia. J Pain Res. 2019;12:679–687. doi:10.2147/JPR.S185073
19. Tan J. Education and colonial transition in Singapore and Hong Kong: comparisons and contrasts. Comp Educ. 1997;33(2):303–312. doi:10.1080/03050069728587
20. Lancsar E, Savage E. Deriving welfare measures from discrete choice experiments: inconsistency between current methods and random utility and welfare theory. Health Econ. 2004;13(9):901–907. doi:10.1002/hec.870
21. Poulos C, Hauber AB, González JM, Turpcu A. Patients’ willingness to trade off between the duration and frequency of rheumatoid arthritis treatments. Arthritis Care Res. 2014;66(7):1008–1015. doi:10.1002/acr.22265
22. Finkelstein EA, Ozdemir S, Malhotra C, Jafar TH, Choong Hui Lin L, Gan Shien Wen S. Understanding factors that influence the demand for dialysis among elderly in a multi-ethnic Asian society. Health Policy (New York). 2018;122(8):915–921. doi:10.1016/j.healthpol.2018.06.008
23. Whitty JA, Walker R, Golenko X, Ratcliffe J. A think aloud study comparing the validity and acceptability of discrete choice and best worst scaling methods. PLoS One. 2014;9(4):e90635. doi:10.1371/journal.pone.0090635
24. Johnson FR, Kanninen B, Bingham M, Özdemir S. Experimental design for stated-choice studies. In: Kanninen BJ, editor. Valuing Environmental Amenities Using Stated Choice Studies: A Common Sense Approach to Theory and Practice. Dordrecht: Springer Netherlands; 2007:159–202.
25. Orme B. Sample size issues for conjoint analysis; 2019. Available from: https://sawtoothsoftware.com/resources/technical-papers/sample-size-issues-for-conjoint-analysis-studies.
26. Train KE. Discrete Choice Methods with Simulation.
27. Gonzalez JM. A guide to measuring and interpreting attribute importance. Patient. 2019;12(3):287–295. doi:10.1007/s40271-019-00360-3
28. Dickinson JE, Paech MJ, McDonald SJ, Evans SF. Maternal satisfaction with childbirth and intrapartum analgesia in nulliparous labour. Aust N Z J Obstet Gynaecol. 2003;43(6):463–468. doi:10.1046/j.0004-8666.2003.00152.x
29. Rust G, Nembhard WN, Nichols M, et al. Racial and ethnic disparities in the provision of epidural analgesia to Georgia Medicaid beneficiaries during labor and delivery. Am J Obstet Gynecol. 2004;191(2):456–462. doi:10.1016/j.ajog.2004.03.005
30. Anabah TW, Falagán AA. Investigating determinants for woman’s choice to accept an epidural for labour analgesia at the delivery unit of the Tamale Teaching Hospital. J Clin Anesth Pain Manag. 2021;5(2):235–240.
31. Maternity and Antenatal charges. Available from: https://www.sgh.com.sg/patient-care/specialties-services/obstetrics-and-gynaecology/pages/maternity-and-antenatal-charges.aspx.
32. Estimated bill calculator form delivery. Available from: https://www.kkh.com.sg/patient-care/Pages/Estimated-Bill-Calculator-Form-Delivery.aspx.
33. Government S. Marriage and parenthood scheme. Available from: https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/marriage-and-parenthood-schemes.
34. Borrelli S, Evans K, Pallotti P, Evans C, Eldridge J, Spiby H. Mixed-methods systematic review: childbearing women’s views, experiences, and decision-making related to epidural analgesia in labour. J Adv Nurs. 2020;76(12):3273–3292. doi:10.1111/jan.14555
35. Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997;87(3):479–486. doi:10.1097/00000542-199709000-00005
36. Hidaka R, Callister LC. Giving birth with epidural analgesia: the experience of first-time mothers. J Perinat Educ. 2012;21(1):24–35. doi:10.1891/1058-1243.21.1.24
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.