Back to Journals » Research and Reports in Neonatology » Volume 12
Parental Satisfaction with Neonatal Intensive Care Unit Services and Associated Factors in Jimma University Medical Center, Ethiopia
Authors Adal Z , Atomsa G , Tulu G
Received 25 November 2021
Accepted for publication 13 April 2022
Published 27 April 2022 Volume 2022:12 Pages 1—10
DOI https://doi.org/10.2147/RRN.S351224
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Schelonka
Zinash Adal,1 Gamechu Atomsa,1 Gemechu Tulu2
1School of Nursing, Faculty of Health Science, Jimma Institute of Health, Jimma University, Jimma, Ethiopia; 2Kuyu General Hospital, Oromia Regional Health Bureau, Oromia, Ethiopia
Correspondence: Gemechu Tulu, Kuyu General Hospital, Oromia Regional Health Bureau, Gerba Guracha, Ethiopia, Tel +251-901-142-299, Email [email protected]
Background: Patient satisfaction is an important aspect of the quality of care in the inpatient setting. In neonatal intensive care units (NICUs), parent satisfaction and their experiences are fundamental to assessing clinical practice and improving the quality of care delivered to infants and parents. In developing countries like Ethiopia, the satisfaction of parents of neonates requiring intensive care is often overlooked. Thus, the study aimed to assess parental satisfaction with neonatal intensive care unit services and associated factors.
Methods: A hospital-based, cross-sectional study was conducted at Jimma University Medical Center from July to August, 2021. Parents of admitted newborn infants were selected by convenience sampling. Data were collected using a structured questionnaire adapted from Empowerment of Parents in Intensive Care (EMPATHIC). Data were entered into Epidata 4.6 and exported into SPSS Version 25 for analysis. Bi-variable and multivariable logistic regression analyses were used to identify factors associated with parental satisfaction.
Results: Of 122 eligible parents, 114 (93.5%) participated. Parental satisfaction with NICU services was 57.9% [95% CI: (49.1%, 66.7%)]. More than half (60.5%) of the parents responded that their baby gets better care in the incubator/bed. Compassionate and respectful care [AOR = 5.88, 95% CI: (2.19– 15.78)] was significantly associated with parental satisfaction.
Conclusion: A sizable proportion of the parents was not satisfied with the services of the neonatal intensive care unit at Jimma Medical Centre. Compassionate and respectful care is associated with parental satisfaction. The results of this study support strengthening a culture of family-centered care via compassionate and respectful care.
Keywords: Jimma Medical Center, parental satisfaction, neonatal intensive care unit, Ethiopia
Plain Language Summary
In the neonatal intensive care unit (NICU), communication between parents and their baby’s caregivers is critical. Parents are encouraged to speak with doctors and nurses in order to gain a better understanding of their baby’s condition, participate in medical decision-making, and provide care for their child. Our study showed that parents had difficulty collaborating with healthcare providers. We attempted to identify issues that influence parental satisfaction with NICU care.
We interviewed parents of newborn babies after hospital discharge and found approximately half of newborn caregivers were satisfied with the service provided during their stay at the hospital. Established family-centered care should be a key priority to inform and engage newborn caregivers in improving outcomes of critically ill infants.
Background
Globally, newborn deaths account for 40% under age five mortality. Each year nearly one million infants die on the day of birth and two million die during the first week of age. South Asia and Sub-Saharan Africa account for about three-quarters (79%) of the total burden of neonatal deaths.1 Ethiopia has a mortality rate of at 29 per 1000 live births,2 one of the highest in all of Africa. Faced with an alarmingly high neonatal death rate, the Ethiopian Federal Ministry of Health (FMOH) launched the Newborn Corner initiative at 100 health facilities in 2009, with backing from the United Nations International Children’s Economic Fund and technical assistance from the Ethiopian Pediatric Society.3 The FMOH has paid due emphasis to expansion of quality high impact neonatal interventions in health centers and hospitals in its attempt to achieve Sustainable Development Goals (SDGs). This includes establishing basic newborn care units (newborn corners) at health centers and NICUs at hospitals. As initial activity FMOH with partners has started strengthening and/or establishing NICU in selected federal level and university teaching hospitals.4
The term “patient satisfaction “often defines healthcare quality related to patient retention, clinical outcomes, and medical malpractice claims.5 There is growing awareness that family-centered care is a vital component of overall quality in hospital based care. The American Academy of Pediatrics affirms a family-centered care approach for all pediatric care, including neonatal care, and recommends “conducting attending physician presentations and round discussions in the patients’ room with the family present should be standard practice.”6 Parental engagement and satisfaction are important factors for pediatric inpatient care as they help parents better understand their child’s illness and improve adherence to the treatment plan.7 Family engagement in the inpatient care of small and sick newborns leads to better health and developmental outcomes, improved patient and family experiences, and enhanced clinician and staff satisfaction. In addition, the family-centered care approach reduces the length of hospital stay, lessens parent stress and anxiety at discharge, and decreases the rate of readmissions to the NICU, thus increasing the parents’ satisfaction with the services.8
Parental satisfaction with NICU services varies geographically. Parental satisfaction was measured at 76% in Norway, 86% in Turkey, 70% in Germany, 80% in India, 42% in public hospitals in Addis Ababa, and 60% in TikureAnbesa Specialized Hospital in Ethiopia.9–14
Parent satisfaction with NICU services relates to maternal socio-demographics, provider communication and accessibility, laboratory procedures, availability of prescribed drugs and medications from the hospital pharmacy, cleanliness of toilets and bathrooms, and availability of drinking water.15 Previous study in this area has focused on maternal prenatal care; far less is known about inpatient neonatal care. Little is known related to perceptions of the quality of care in developing countries including Ethiopia;16 therefore, this study aims to describe provider attributes and features of neonatal critical care that influence maternal and caregiver satisfaction.
Materials and Methods
Study Design and Setting
A facility-based cross-sectional study was conducted at Jimma University Medical Center (JUMC) from July 15 to August 12, 2021. Jimma town is the capital of the Jimma zone and is located 345 km south-west of the capital of Ethiopia, Addis Ababa. Jimma University Medical Center is the tertiary and referral teaching hospital in the south-west part of the country. Ethiopian hospitals are classified into three levels based on the functional capabilities of facilities that provide inpatient care for newborn infants. Level I (Basic): organized to give services like neonatal resuscitation, postnatal evaluation and care of newborns, physiologically stable preterm babies, and stabilize and transfer preterm babies born before 35 weeks of gestation. Level II (Specialty): provides care to infants born at > 32 weeks’ gestation and weighing > 1500 g who have physiologic immaturity such as apnea of prematurity, inability to maintain body temperature, or inability to take oral feedings; who are moderately ill with problems that are expected to resolve rapidly. Level III (subspecialty): provides continuous life support and comprehensive care to extremely high-risk newborn infants as well as those suffering from complex and critical illnesses.4
Jimma University Medical Center is the only level III NICU in the city. The unit has 31 neonatal nurse staff. The unit has a total of 53 beds, including Kangaroo Mother Care (KMC) beds, 7 incubators, 19 radiant warmers, 4 Continuous Positive Airway Pressure (CPAP), and a phototherapy machine. The NICU has an average admission rate of 170 neonates every month. Another public hospital (Shenan Gibe General Hospital) in the city has a level I NICU center.
Study Participants, Sample Size, and Sampling Procedures
All parents of infants admitted to the JUMC NICU and who visited during the study interval were eligible to participate. Parents of neonates born with major congenital malformations or who died were excluded from the study.
The sample size was calculated using the single population proportion formula, assuming 59.8% for parental satisfaction (p) from a study conducted in TikurAnbessa Specialized Hospital Ethiopia,14 with a 95% confidence interval and a 5% margin of error. Since the target population was less than 10,000, the final sample estimated by the correction formula was 116. By adding a 5% non-response rate, a final sample size of 122 was obtained. A convenient sampling method was employed. All mothers or fathers whose neonates were admitted to the NICU were interviewed successively during discharge at all working times.
Study Variables
The outcome variable is parental satisfaction. The independent variables consist of socio-demographic variables including age, residency, marital status, educational level, and occupation; organizational variables including length of stay; healthcare provider variables including compassionate and respectful care (CRC); and parental variables including parental involvement.
Operational Definitions
The operational definitions are shown in Table 1.
 |
Table 1 Operational Definitions |
Data Collection Methods, Tools, and Procedures
A validated standardized questionnaire adapted from Empowerment of Parents in Intensive Care (EMPATHIC)17 was used to measure the outcome variable (parental satisfaction). The Empowerment of Parents in Neonatal Intensive Care (EMPATHIC-N) is a newly developed yet empirically reliable and valid measure for the assessment of parental satisfaction with the care provided by Neonatal Intensive Care Units (NICU). The English version of the questionnaire was translated into the local language, which is Afan Oromo, and again translated back to English by experts who were fluent in both languages to check its consistency. The validity of the tool after translation was checked by the language experts and clinicians who worked in the NICU for more than five years to check the cultural validity of the translated tool. The questionnaire contains six components with 54 items (having eight questions to assess socio-demographic characteristics; five questions related to the characteristics of the admitted neonate; six questions related to hospital services provision; five questions assessing parent experience; seven questions to measure the level of compassionate and respectful care; 10 questions related to patient care and treatment; and 13 questions related to information and communication). The overall mean score of questions on five Likert scales was 94.74 (SD = ± 11.5), with a minimum of 43 and a maximum of 126. One data collector (BSc Nurse) and one supervisor (MPH) were recruited for data collection. The parents of the admitted newborn were interviewed on the date of discharge by the data collector.
Data Quality Control
The questionnaire was pretested on 5% of the sample among parents of newborns at Shenan Ghibe Hospital in Jimma Town two weeks before the actual data collection. Based on the pretest results, the questionnaires were also evaluated and redesigned. One-day training was given to the data collector and a supervisor on the objectives of the study, how to ensure data quality, and the data collection process before they started data collection. During the data collection phase, there was constant supervision. Collected data was checked for its completeness. To achieve the reliability of the instrument in the study, Cronbach’s alpha was calculated. The Cronbach’s alpha was calculated for each subset of the questionnaire with compassionate and respectful care at 0.64, patient care and treatment at 0.63, and information and communication at 0.67. Finally, the overall Cronbach’s alpha reliability coefficient for the instrument was 0.81, which was within the acceptable reliability range.
Data Processing and Analysis
Data was entered into Epidata version 4.6 and exported to SPSS version 25 for further analysis. For socio-demographic and other key factors, descriptive analyses such as frequency distribution were calculated. Bivariate analysis was employed to show the relationship between parental satisfaction and associated factors. A multivariable logistic regression analysis was performed to control for potential confounders and identify factors independently associated with parental satisfaction with NICU services. The model fitness was checked by the Hosmer-Lemeshow test, and it was fit (P-value = 0.572). P-value 0.05 and adjusted odds ratios (AOR) with a 95% confidence interval (CI) were used to determine the strength of the association between the independent and the outcome variable.
Ethical Clearance
This study was conducted per the Declaration of Helsinki. Ethical approval was obtained from Jimma University, Institutional Review Board (IRB) of protocol No. 20/2013. A letter of permission was obtained from Jimma University Medical Center. The purpose of the study was explained to all study participants (neonate’s parents) about the information needed and written informed consent was obtained to collect data and communicate the findings through publication. The responses of participants were confidential and anonymous.
Results
Socio-Demographic Characteristics of the Respondents
Of 122 eligible parents, 114 (93.5%) participated. The mean age of the study participant was 26.8 (± 6.2 SD) years with a minimum of 18 and a maximum of 47 years. Around three-fifth (60.5%) of the participants were urban residents. The majority (78.9%) of the participants were female and 108 (94.7%) were married. Forty-seven (41.2%) attended primary education, while more than half of (62.3%) identified as house wives. On the other hand, 58 (51%) of newborns were male and the majority (60%) had a birth weight of greater than 2500g. The mean gestational age of the neonates was 36 weeks and 5 days (±2.2 SD) weeks and the average length of stay at NICU was 12.5 (± 5SD) days. Moreover, the majority (84.2%) of neonates in NICU get better after admission (Table 2).
 |
Table 2 Socio-Demographic Characteristics of the Respondents, JUMC, 2021 |
Level of Parental Satisfaction
Among the total participants, the overall parental satisfaction in the neonatal intensive care unit services of Jimma University Medical Center was 66 (57.9%) with a 95% CI (49.1%, 66.7%) (Figure 1).
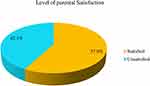 |
Figure 1 Level of parental satisfaction to NICU services, JUMC, 2021. |
Parental Experiences on NICU Services
The majority of the study participants (55.3%) report that they could not easily access the NICU room. Furthermore, nearly one-third (30%) of the participants did not get drugs from the hospital pharmacy, and 61.4% did not get laboratory tests. Around 57% of the participants get clear information on the status of their child. More than half (56.1%) of the parents were informed about the expected health outcomes of the neonate. Around 65% of the parents have received sympathy from the doctors and nurses. Approximately two-thirds of the participants believed that they received compassionate and respectful care from nurses and doctors (Table 3). The mean score of CRC was 23.82 (SD = ± 4.3) whereas the mean score of parental involvement was 14.66 (SD = ± 3.45). There is a significant association between CRC and parental satisfaction (Pearson Chi-Square= 0.000).
 |
Table 3 Parental Experience at NICU Services Response on Five-Point Likert Scale, JUMC, 2021 |
Factors Associated with Parental Satisfaction
In bi-variable analysis age, sex of the parent, marital status, residency, parental involvement, and compassionate and respectful caring were factors associated with parental satisfaction at a P-value of ≤ 0.25 (Table 4).
 |
Table 4 Bivariate Analysis of Factors Associated with Parental Satisfaction to NICU Services, JUMC, 2021 |
The variables with P-value ≤ 0.25 were subjected to multivariable logistic regression analysis and only Compassionate and respectful caring remained to have a statistically significant association with parental satisfaction on neonatal services at a P-value ≤ 0.05. Findings from this study show the odds of parents who got CRC from health care providers were 5.88 times more likely to be satisfied than those who did not get CRC (AOR = 5.88, 95% CI: 2.19–15.78) (Table 5).
 |
Table 5 Multivariable Analysis of Factors Associated with Parental Satisfaction to NICU Services, JUMC, 2021 |
Discussion
Customer satisfaction is currently a quality core metric for healthcare organizations. The NICU is a stressful environment for the parents of newborns, and family-centered care lessens parental stress and improves involvement in medical decision-making and provides continuity of care. The current study aimed to assess parental satisfaction with neonatal intensive care unit services and associated factors at Jimma University Medical Center.
The study found that 58% (95% CI [49.1%, 66.7%]) of parents were satisfied with NICU services. This is similar to results founds in a study done at the TikureAnbesa Specialized Hospital14 and higher than satisfaction rates at government hospitals in Addis Ababa.13 This might be due to the current emphasis by the government of Ethiopia to maternal and child health in the ongoing health sector transformation plan. Ethiopia’s Federal Ministry of Health incorporated compassionate and respectful care initiative to improve quality of care in the health sector transformation plan (HSTP).18 Furthermore, the authors developed standardized and validated tool that measures parent satisfaction for NICU services.
Satisfaction scores in the current study were lower than those described in Norway,9 Turkey,10 Germany,11 and India.12 This might be due to differences in socio-economic status and health service quality. Developed countries generally provide an overall higher quality of care than developing countries. In developed countries, healthcare organizations integrate technology into both their patient engagement strategy and operational framework that can improve the overall patient experience.
The impact of environmental condition on health and well‑being has been a major focus of the study for many researchers in the field of neonatal studies, but in our study environmental factors had no significant impact on parental satisfaction.19 This might be due to the Jimma Medical Center has separate ward equipped with basic equipment, medications and laboratory investigations needed for NICU services.
In this study, we show that parent satisfaction with NICU services is associated with compassionate and respectful care (CRC). The odds of parent satisfaction for their babies who received CRC from healthcare providers were six times greater compared to the parents who did not get CRC. The findings of this study are similar to the study conducted in Japan in that parents who received CRC from nurses were more satisfied.20 Parents will be more satisfied when healthcare providers have a positive attitude, use simple and clear language, recognize mothers or families of newborns, give care with respect, and can maintain their dignity.21
Our study revealed that a sizable proportion of parents are not satisfied with NICU services provided at Jimma Medical Centre. We postulate that greater implementation of family-centered care will improve parent satisfaction in the NICU. Furthermore, developing tools to elicit feedback and to facilitate communication at discharge should improve the transition out of hospital to home. Compassionate and respectful care is directly related to parent satisfaction during the NICU stay. We advocate for ongoing improvement in culture shift toward CRC delivery.
Limitations
The strength of this study was that it used standard tools for data collection. This study may have the following limitations: the sample size was small, and because it was a cross-sectional study, the cause-effect link could not be proven.
Abbreviations
AOR, adjusted odds ratio; BSc, Bachelor of Science; CI, confidence interval; COR, crude odd ratio; CRC, compassionate respectful caring; FMOH, Federal Ministry of Health; JUMC, Jimma University Medical Center; MPH, Masters of Public Health; MSc, Master of Science; NICU, Neonatal Intensive Care Unit; SD, Standard Deviation; SPSS, Statistical Packages for Social Science.
Data Sharing Statement
Data will be available upon request from the corresponding author.
Ethics Approval and Consent to Participate
Ethical approval was obtained from Jimma University, Institutional Review Board (IRB) of protocol No. Nurse 20/2013. A letter of permission was obtained from Jimma University Medical Center. Each participant’s written informed consent was gained once the purpose of the study was stated. The respondent’s confidentiality was maintained.
Acknowledgments
The authors would like to acknowledge Jimma University, School of Nursing for the approval of the ethical clearance and Jimma University Medical Center for giving data collection supportive letter, and Neonatal Intensive Care Unit for permitting us to collect the data. We also forward our gratitude to data collectors, supervisors, and study participants.
Author Contributions
All authors contributed significantly contribution to the conception, study design, execution, data acquisition, analysis and interpretation; participated in the drafting the manuscript, critical review of the manuscript; agreed on the journal to which the article was submitted; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Funding
The authors received no direct funding for this research.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Wardlaw T, You D, Hug L, Amouzou A, Newby H. UNICEF Report: enormous progress in child survival but greater focus on newborns urgently needed. Reprod health. 2014;11:1–4.
2. Berhan Y, Berhan A. Review of maternal mortality in Ethiopia: a story of the past 30 years. Ethiop J Health Sci. 2014;24:29–40. doi:10.4314/ejhs.v24i0.4S
3. Ethiopian Federal Ministry of Health. National strategy for newborn and child survival in Ethiopia; 2015.
4. Ethiopian Federal Ministry of Health. Neonatal intensive care unit training manual; 2014.
5. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010;3(3):151–155. doi:10.4103/0974-2077.74491
6. Frankowski BL. American Academy of Pediatrics guidelines for the prevention and treatment of head lice infestation. Am J Manag Care. 2002;10(9):269–272.
7. Zolaly MA. Satisfaction of parents of paediatric patients with physicians communication skills in Almadinah Almunawwarah, Kingdom of Saudi Arabia. J Taibah Univ Medical Sci. 2012;7(1):29–34. doi:10.1016/j.jtumed.2012.07.007
8. Verma A, Maria A, Pandey RM, et al. Family-centered care to complement care of sick newborns: a randomized controlled trial. Indian Pediatr. 2017;54(455–459):5.
9. Hagen IH, Iversen VC, Nesset E, et al. Parental satisfaction with neonatal intensive care units: a quantitative cross-sectional study. BMC Health Serv Res. 2019;19:37. doi:10.1186/s12913-018-3854-7
10. Oren B, Zengin N, Yildiz N. The Turkish adaptation of scale to measure patient perceptions of the quality of nursing care and related hospital services: a validity and reliability study. North Clin Istanbul. 2016;3(3):187–193. doi:10.14744/nci.2016.42650
11. Weissenstein A, Straeter A, Villalon G, et al. Parent satisfaction with a pediatric practice in Germany: a questionnaire- based study. Ital J Pediatr. 2011;37:31. doi:10.1186/1824-7288-37-31
12. Taneja R, Batra P, Sadiza J. Maternal satisfaction with services provided in the neonatal step‑down ward in a public sector hospital in North India. J. Clin. Neonatol. 2020;9:132–137. doi:10.4103/jcn.JCN_137_19
13. Endale H. Parental satisfaction concerning their Neonatal care and associated factors in Selected governmental hospital, Addis Ababa, Ethiopia; 2017.
14. Getasew T, Yosief T. Parental satisfaction and involvement concerning care of their hospitalized child. Global Sci J. 2019;7(3):341–362.
15. Srivastava A, Avan BI, Rajbangshi P, et al. Determinants of women ’ s satisfaction with maternal health care: a review of literature from developing countries. BMC Pregnancy and Child Birth. 2015;15:1–12.
16. Senarath U, Gunawardena NS. Development of an instrument to measure patient perception of the quality of nursing care and related hospital services at the National Hospital of Sri Lanka. Asian nursing research. 2011;5(2):71–80.
17. Lake ET, Smith JG, Staiger DO, et al. Measuring parent satisfaction with care in neonatal intensive care units: the EMPATHIC-NICU-USA questionnaire. Front Pediatr. 2020;8:541573. doi:10.3389/fped.2020.541573
18. Ethiopian Federal Ministry of Health. Ethiopian health sector transformation plan. 2015/16–2019/20; 2015.
19. Stevens DC. Single-room neonatal intensive care: state of the practice. Nurs Res Clin Pract. 2015;4:14–16.
20. Matziou V, Boutopoulou B, Chrysostomou A, et al. Parents ’ satisfaction concerning their child ‘s hospital care. JPN J Nurs Sci. 2011;8:163–173. doi:10.1111/j.1742-7924.2010.00171.x
21. World Health Organization. Standards for improving quality of maternal and newborn care in health facilities; 2016.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
