Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 13
P2RX7 Gene rs1718125 Polymorphism is Related with Postoperative Pain and Fentanyl Intake in Esophageal Cancer Patients
Authors Zheng C, Wang J, Xie S
Received 6 March 2020
Accepted for publication 20 August 2020
Published 12 November 2020 Volume 2020:13 Pages 585—589
DOI https://doi.org/10.2147/PGPM.S252798
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Cuijuan Zheng,1 Jiayu Wang,1 Shouxiang Xie2
1Department of Anesthesiology, The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University, Huaian, Jiangsu, People’s Republic of China; 2Department of Emergency, The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University, Huaian, Jiangsu, People’s Republic of China
Correspondence: Shouxiang Xie Tel/Fax +86-517-80878245
Email [email protected]
Background: Prevention and control of postoperative pains are essential, which affects the prognosis and life quality of patients. Fentanyl is a widely used opioid drug for pre-, intra- and postoperative analgesia. Identifying a patient’s genotype before surgery may help to control the fentanyl dose in the perioperative period.
Patients and Methods: This study enrolling 645 esophageal cancer (EC) patients was aimed to investigate the associations of P2RX7 gene rs1718125 polymorphism with fentanyl intake and postoperative pains in a Chinese Han population. Genotyping was accomplished by direct sequencing and polymerase chain reaction.
Results: The GA/AA genotype carriers showed lower visual analog scale scores at postoperative 0, 6 and 24 h, but not at 48 h, compared with the GG genotype. The fentanyl consumption of GG genotype was remarkably more relative to the GA/AA genotype at 6 and 24 h after treatment.
Conclusion: P2RX7 rs1718125 polymorphism is connected to the postoperative pains and fentanyl use for EC patients.
Keywords: esophageal cancer, fentanyl, P2RX7, single nucleotide polymorphism, postoperative pain
Introduction
Esophageal cancer (EC) ranks the sixth cause of cancer-related death globally.1 Approximately 455,800 EC patients and 400,200 deaths were reported worldwide in 2012.2 There were about 477,900 new EC patients and 375,000 deaths in 2015 in China.3 Of the two main histologic types of EC, esophageal squamous cell carcinoma (ESCC) (the other is adenocarcinoma) accounts for approximately 90% of the 456,000 incident ECs each year.4 In reality, the median survival time of EC is short, because most patients are diagnosed at the advanced stage, which is incurable. Most EC patients require effective treatments, including chemotherapy, chemoradiotherapy, and surgical operation which is the most effective one.5 Since appropriate postoperative pain management can improve the outcomes of EC patients,6 postsurgical pain managements are extremely pivotal for EC patients.
P2X7 is a non-selective purinoceptor function route stimulated by extracellular ATP. P2X7 is upregulated in the injured nerves, dorsal root ganglia, monocytes and lymphocytes of neuropathic pain patients.7,8 The purinergic receptor P2X7 (P2RX7) gene, encoding the P2X7 receptor, is associated with pains in human patients9 and regulates pains.10 P2RX7 is also related to neuropathic pain, neurodegeneration, and neuroinflammation.7,11 The P2X7 receptor may regulate variability in chronic pain sensitivity.12 P2RX7 gene variants may influence the function of P2X7 receptor protein, thereby affecting the analgesic efficacy of opioids and the patient sensitivity to postsurgical pains. Some single-nucleotide polymorphisms (SNPs) in the P2RX7 gene are correlated with pain sensitivity in a diabetic neuropathic pain patient population.13
A recent Japanese study shows that P2RX7 gene rs1718125 polymorphism influenced fentanyl intake and cold pain sensitivity following painful orofacial cosmetic operation.14 A subsequent Chinese study uncoverd a correlation of this polymorphism with post-surgical pains and fentanyl use in lung cancer patients.15 Up to date, no study has shed light on the relationship between this polymorphism and analgesic fentanyl in EC patients. Thus, we conducted this study to explore the effects of this SNP on post-surgical pains and fentanyl administration in EC patients receiving surgery in an Eastern Chinese Han population.
Patients and Methods
Patients and Ethics Statement
A total of 645 EC patients were selected from the Huaian No.1 People’s Hospital. The subjects should meet the following criteria: adult, diagnosis with EC, receiving EC resection, and native Chinese Han population. We excluded the patients with history of esophageal disease and a second primary tumor, taking pain medication within three months, and receiving preoperative chemotherapy or radiation therapy.
The study protocol was approved by the institutional review broad of the tested Hospital. Written informed consents of all individuals were obtained from each subject. Personal and medical confidentiality was carried out according to the Helsinki declaration.
Induction and Maintenance of Anesthesia
General anesthesia was initiated by administration of fentanyl (5–10 μg/kg), midazolam (0.4–0.6 μg/kg), vecuronium bromide (0.08 mg/kg), and etomidate (0.3 mg/kg). Anesthesia was maintained by a combined use of inhalation (sevoflurane, 1–2 mac) and intravenous injection (propofol, 4 mg/kg/hour). The fentanyl infusion velocity was adjusted according to bispectral index and hemodynamic parameters. The fentanyl dosage and operation time in each patient were recorded. Intravenous injection of 0.1 mg/h fentanyl was conducted 30 minutes before completion of the surgery.
Postoperative Analgesia
All patients were treated with postoperative analgesia when they were stable and awake. Postoperative patient-controlled analgesia (1 mg of fentanyl and 200 ug of dexmedetomidine in 100 mL of normal saline) was performed using an infusion auto-pump (Apon, ZZB-300), which gave a 2-mL bolus of solution at 5 min of lockout. Extra intravenous and oral opioids were administrated depending on the pain status of each patient. Dose of fentanyl was standardized to body weight. The pain severity of each patient was evaluated at 6, 24, and 48 h after surgery by use of a 100-mm visual analog scale (VAS, 0 = no pain, 10 = unbearable pain).
DNA Extraction and Genotyping
Peripheral blood Genomic DNA (2 mL) was isolated using a Puregenee DNA purifying kit (Gentra, Minneapolis, MN, US) according to standard procedures. DNA purity and concentration were detected by electrophoresis and absorbance measurement, respectively. The rs1718125 polymorphism of P2RX7 gene was genotyped by polymerase chain reaction (PCR) and direct sequencing. The primers of 5ʹ-TCA AGTCCTACAGGGTTTCTC-3ʹ (forward) and 5ʹ-GGCTGGTGCTCTTTGGTA-3ʹ (reverse) were used in PCR amplification. PCR conditions were: holding at 95°C, 8 min; denaturing at 94°C, 30 s, annealing at 55°C, 30 s, extending at 72°C, 1 min, 35 cycles; holding at 72°C, 10 min. The PCR products were detected on 2% agarose gel electrophoresis with ethidium bromide and observed under UV light. PCR products were sent to Genscript (Nanjing, Jiangsu, China) for sequencing. We repeatedly measured 5% of the samples to ensure the accuracy of genotyping.
Statistical Methods
SPSS 13.0 (IBM, Chicago, IL) was used to conduct all statistical analyses. Categorical indices (percentages) between groups were compared via Chi-squared test. Continuous indices were represented as mean ± standard deviation and compared between groups using an independent sample t-test or one-way analysis of variance (ANOVA). The significant level was P < 0.05.
Results
Population Characteristics
Table 1 shows the demographic and medical information of the EC patients. The mean age was 61.12 ± 10.41 years and the male/female ratio was 1.6. The majority of the EC cases (63.4%) were patients with ASA classification I. We also recorded the duration of operation, duration of analgesia and intraoperative fentanyl. The distributions of genotypes and alleles of the P2RX7 gene rs1718125 polymorphism in EC patients are provided in Table 2. The corresponding frequencies of the GG, AG and AA genotypes were 47.1%, 43.3% and 9.6%, respectively.
 |
Table 1 The Demographic and Clinical Characteristics of Esophageal Cancer |
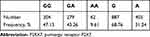 |
Table 2 The Genotype and Allele Frequencies of P2RX7 Gene rs1718125 Polymorphism in the Study Sample |
P2RX7 Gene rs1718125 Polymorphism Analysis
This study investigated the differences of clinical and demographic characteristics among three genotypes (Table 3). Our results revealed that P2RX7 rs1718125 polymorphism was associated with ASA classification I/II.
 |
Table 3 Comparison of Demographic and Clinical Characteristics Among 3 Genotypes of rs1718125 Polymorphism in Patients with Esophageal Cancer |
Later, we evaluated postoperative VAS score at 0, 6, 24 and 48 h among different genotypes (Table 4). Significant associations between the genotypes of rs1718125 polymorphism and VAS scores were found postoperatively at 0, 6 and 24 h, but not at 48 h. The VAS score of the GG genotype remarkably surpassed that of the GA or AA genotype.
 |
Table 4 Postoperative VAS Score in Different Groups (x ± s) |
Table 5 provides the postoperative fentanyl consumption at postoperative 6, 24 and 48 h among GG, GA, and AA genotype carriers. Carriers of the AA and GA genotype relative to the GG genotype showed low fentanyl consumption at postoperative 6 and 24 h. However, AA genotype but not GA genotype was associated with low fentanyl consumption at postoperative 48 h.
 |
Table 5 Postoperative Fentanyl Consumption in 3 Groups (x ± s) |
Discussion
Postoperative pains are post-surgical complications that affect the prognosis and life quality of patients.16 Data indicate that postoperative pains are still inadequately managed in the world, but the reasons are unclear.17 Nevertheless, the development of controlling postoperative pains has substantially been improved in past decades. Fentanyl is a widely used drug among all post-operative analgesics.
Fentanyl, a synthetic opioid analgesic, exerts its effects primarily on the μ–opioid receptor.18 Fentanyl blood level between 0.3 and 1.2 ng/mL usually yields sufficient analgesia.18 Fentanyl demonstrates greater analgesic potency through rapidly crossing the blood-brain barrier. Fentanyl, an opioid drug, is generally used for pre-, intra-, and postoperative analgesia.19 According to the genetics-based pain therapy, the genetics-based personalized pain therapy will be promising after the all the human DNA genes in the development of nociception neurobiology are identified.20 Identifying the patient genotype before operation may help to select the analgesic agent and dosage after operation.21 In this study, we wanted to find a target gene that can exert effects on fentanyl efficacy for EC patients.
P2RX7 gene variants are involved in the modulation of human pain sensitivity.9 Sorge et al indicated that selectively aiming at P2X7R pore generation was probably a novel scheme for personalized therapy of chronic pains.12 Ide et al uncovered that haplotypes of P2RX7 gene loci were related to both analgesia and cold pain sensitivity of fentanyl.14 Herein, we explored the connections of P2RX7 gene rs1718125 polymorphism with post-surgical pain sensitivity and fentanyl intake in 645 operation-treated EC patients. The carriers of GA and AA versus the GG genotype had significantly lower VAS scores at postoperative 6 and 24 h, but not at 48 h. Those data suggested that EC cases with GA and AA genotypes were not sensitive to pain and perceived weak pain after operation. Obviously, Ma et al obtained conflicting findings that lung cancer patients with GA and AA relative to the GG genotypes had higher VAS scores.15 Here we observed that AA genotype carriers showed low VAS score, but Ma et al showed AA genotype carriers presented high VAS score.15 Four factors may explain these inconsistent findings. First, genetic heterogeneity is different for EC and lung cancer. Second, clinical heterogeneity of these two disorders is diverse. Third, the sample sizes differ. Fourth, different exposure factors may be potential reasons. In addition, we assessed the association between postoperative fentanyl consumption and P2RX7 gene rs1718125 polymorphism genotypes among this population, and found that AA and GA genotype versus GG genotype carriers yielded low fentanyl intake at postoperative 6 h and 24 h. To sum up, the involvement of P2RX7 in the mediation of naive pain sensitivity and analgesic effectiveness is clear. However, the underlying mechanisms are not well understood. Some studies indicate that P2RX7 is associated with the hyperexcitability of nociceptive neurons by the secretion of both IL-1β22 and TNF-α,23 which play pivotal roles in the production and control of pains. Further studies are required to uncover the mechanisms.
Potential limitations in this study should be addressed. First, the sample size was not large enough. Second, only one SNP of P2RX7 gene was investigated. Third, whether P2RX7 gene rs1718125 polymorphism affected other postoperative responses was not explored. Last, the potential mechanisms of this polymorphism related to the analgesic effects and postoperative pain control of fentanyl were not investigated.
To sum up, P2RX7 rs1718125 polymorphism correlates with the postoperative pain and fentanyl consumption of EC patients.
Abbreviations
EC, esophageal cancer; PCR, polymerase chain reaction; VAS, visual analog scale; P2RX7, purinergic receptor P2X7; SNP, single-nucleotide polymorphism.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Domper Arnal MJ, Ferrandez Arenas A, Lanas Arbeloa A. Esophageal cancer: risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol. 2015;21(26):7933–7943. doi:10.3748/wjg.v21.i26.7933
2. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi:10.3322/caac.21262
3. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
4. Abnet CC, Arnold M, Wei WQ. Epidemiology of esophageal squamous cell carcinoma. Gastroenterology. 2018;154(2):360–373. doi:10.1053/j.gastro.2017.08.023
5. Lordick F, Mariette C, Haustermans K, Obermannova R, Arnold D, Committee EG. Oesophageal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v50–v57. doi:10.1093/annonc/mdw329
6. Li Y, Dong H, Tan S, Qian Y, Jin W. Effects of thoracic epidural anesthesia/analgesia on the stress response, pain relief, hospital stay, and treatment costs of patients with esophageal carcinoma undergoing thoracic surgery: a single-center, randomized controlled trial. Medicine (Baltimore). 2019;98(7):e14362. doi:10.1097/MD.0000000000014362
7. Chessell IP, Hatcher JP, Bountra C, et al. Disruption of the P2X7 purinoceptor gene abolishes chronic inflammatory and neuropathic pain. Pain. 2005;114(3):386–396. doi:10.1016/j.pain.2005.01.002
8. Luchting B, Heyn J, Woehrle T, et al. Differential expression of P2X7 receptor and IL-1beta in nociceptive and neuropathic pain. J Neuroinflammation. 2016;13(1):100. doi:10.1186/s12974-016-0565-z
9. Kambur O, Kaunisto MA, Winsvold BS, et al. Genetic variation in P2RX7 and pain tolerance. Pain. 2018;159(6):1064–1073. doi:10.1097/j.pain.0000000000001188
10. Burnstock G. Purinergic mechanisms and pain–an update. Eur J Pharmacol. 2013;716(1–3):24–40. doi:10.1016/j.ejphar.2013.01.078
11. Honore P, Donnelly-Roberts D, Namovic MT, et al. A-740003 [N-(1-{[(cyanoimino)(5-quinolinylamino) methyl]amino}-2,2-dimethylpropyl)-2-(3,4-dimethoxyphenyl)acetamide], a novel and selective P2X7 receptor antagonist, dose-dependently reduces neuropathic pain in the rat. J Pharmacol Exp Ther. 2006;319(3):1376–1385. doi:10.1124/jpet.106.111559
12. Sorge RE, Trang T, Dorfman R, et al. Genetically determined P2X7 receptor pore formation regulates variability in chronic pain sensitivity. Nat Med. 2012;18(4):595–599. doi:10.1038/nm.2710
13. Ursu D, Ebert P, Langron E, et al. Gain and loss of function of P2X7 receptors: mechanisms, pharmacology and relevance to diabetic neuropathic pain. Mol Pain. 2014;10:37. doi:10.1186/1744-8069-10-37
14. Ide S, Nishizawa D, Fukuda K, et al. Haplotypes of P2RX7 gene polymorphisms are associated with both cold pain sensitivity and analgesic effect of fentanyl. Mol Pain. 2014;10:75. doi:10.1186/1744-8069-10-75
15. Ma J, Li W, Chai Q, Tan X, Zhang K. Correlation of P2RX7 gene rs1718125 polymorphism with postoperative fentanyl analgesia in patients with lung cancer. Medicine (Baltimore). 2019;98(7):e14445. doi:10.1097/MD.0000000000014445
16. Andreetti C, Menna C, Ibrahim M, et al. Postoperative pain control: video thoracoscopic versus conservative mini-thoracotomic approach. Eur J Cardiothorac Surg. 2014;46(5):907–912. doi:10.1093/ejcts/ezu092
17. Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet. 2011;377(9784):2215–2225. doi:10.1016/S0140-6736(11)60245-6
18. Brzakala J, Leppert W. The role of rapid onset fentanyl products in the management of breakthrough pain in cancer patients. Pharmacol Rep. 2019;71(3):438–442. doi:10.1016/j.pharep.2019.01.010
19. Raffa RB, Pergolizzi JV
20. Mogil JS. Are we getting anywhere in human pain genetics? Pain. 2009;146(3):231–232. doi:10.1016/j.pain.2009.07.023
21. Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101(1):77–86. doi:10.1093/bja/aen099
22. Clark AK, Staniland AA, Marchand F, Kaan TK, McMahon SB, Malcangio M. P2X7-dependent release of interleukin-1beta and nociception in the spinal cord following lipopolysaccharide. J Neurosci. 2010;30(2):573–582. doi:10.1523/JNEUROSCI.3295-09.2010
23. Suzuki T, Hide I, Ido K, Kohsaka S, Inoue K, Nakata Y. Production and release of neuroprotective tumor necrosis factor by P2X7 receptor-activated microglia. J Neurosci. 2004;24(1):1–7. doi:10.1523/JNEUROSCI.3792-03.2004
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
